The Link Between Homeless Women's Mental Health and Service System Use
There is no question that homeless women show disproportionately high prevalence rates of lifetime mental health problems ( 1 ). The National Survey of Homeless Assistance Providers and Clients (NSHAPC), a data set comprising a nationwide sample of homeless adults, noted that approximately 43% of the homeless population are women: 10% are living as couples, 43% are mothers whose children are with them, and the rest are women living as single adults ( 1 ). The study found that only 28% of women living with children had never had any problem with alcohol, drugs, or mental health in their lifetime. Of the remaining 72% of women living with children, 54% had a mental health problem, 40% had an alcohol problem, and 46% had a drug problem ( 1 ). In this same data set, women living as individuals (including mothers without their children) had similar prevalence rates of drug and alcohol problems but higher rates of mental illness in their lifetimes. Twenty-three percent had never had a problem with alcohol, drugs, or mental health in their lifetime, 65% had a mental health problem, 43% had an alcohol problem, and 43% had a drug problem ( 1 ).
With these high rates of morbidity, homeless women need a wide variety of services, including behavioral, medical, and human services. However, no available study has compared the influences of mental illness and other comorbidities on patterns of service use among homeless women, including mothers living with their children, in a national sample. This study fills these gaps in the literature by using Aday-Andersen's health services utilization model ( 2 ) as a framework. According to this model, service utilization is a function of individuals' predisposition to use services, enabling resources, and need for services. Inequitable access occurs when factors other than need determine service utilization. The model helps to identify variables that are amenable to policy change and to promote equitable access and service ( 2 , 3 , 4 ).
The health services utilization model has been applied to samples of homeless persons ( 5 , 6 , 7 , 8 , 9 , 10 ). The model was recently expanded to improve relevance to studies of homeless and other vulnerable populations ( 7 , 10 ). In some studies, need factors were the best predictors of service utilization among homeless individuals ( 5 , 7 ). In another, need for services was more strongly related to obtaining physical or mental health care services for adults without substance abuse problems compared with those with problems ( 9 ), indicating that substance abuse may be a barrier to needed services.
Other enabling factors that impede health service utilization among homeless individuals include lack of a regular primary care provider or source of care ( 7 ) and lack of health insurance ( 6 ). Predisposing characteristics such as ethnicity and race, age, and education have been identified as increasing or posing barriers to service use. Homeless women tend to report more health services use than homeless men report ( 8 ). Being female and older are associated with having a regular source of health care ( 6 ). Homeless adults who self-identify as belonging to ethnic-racial minority groups are less likely to obtain needed services ( 6 ). There is some evidence that education level is associated with seeking mental health care and physical health services among homeless adults ( 5 ).
Because most studies of service utilization among homeless adults have been based on samples predominantly consisting of homeless men, it is yet to be determined whether the existing findings apply to homeless women. In the only study that applied the modified health services utilization model to a sample of homeless women, severity of homelessness was found to have the strongest association with health and use of health services compared with other individual characteristics ( 10 ). Furthermore, psychological distress led to more barriers to care, more illness, and fewer health care visits. However, this study focused only on health service utilization, and it did not differentiate the service use patterns of single homeless women from homeless mothers with their children. Studies have shown that homeless women living with their children, compared with homeless women living alone, obtained more public entitlements and subsidized housing ( 11 ) and were more likely to sustain public entitlement income ( 12 ). Lack of social supports and smaller social networks are indicators of social isolation and disaffiliation, and the number of social supports is limited among homeless mothers ( 13 ). Few existing studies that used the health services utilization model evaluated contacts with multiple service use sectors ( 9 ), and none used a nationally representative sample.
Using cross-sectional, nationally representative survey data for homeless persons, we evaluated service use among homeless women in the health, behavioral, and human services domains with family status as a major covariate. We aimed to answer three research questions with this study. First, how do service use patterns differ between homeless women with and without mental health problems? Second, with the health services utilization model ( 2 , 3 , 4 ), which variables differentiate service use patterns between homeless women with and without mental health problems? Third, among the breadth of services available, does use of one service enhance the likelihood of use of another, and are the patterns consistent between homeless women with and without mental health problems?
Methods
Data
The NSHAPC sample analyzed in this study included homeless women who use services designed for homeless persons in the United States ( 1 ). Within each sampling area, programs were selected with probability proportionate to size. A random sample of clients was then selected from rosters of clients in each selected program ( 14 ). After the study was completely described to the participants, their willingness to proceed with the interview was taken as consent. The U.S. Census Bureau collected the data and followed its human subjects protection procedures (its equivalent of an institutional review board) that was in place in 1996 when the data were gathered. The overall response rate was 96% ( 15 ).
We followed the definition of homelessness provided in the Stewart B. McKinney Homeless Assistance Act of 1987 to classify respondents as never homeless, formerly homeless, or currently homeless. Currently homeless included persons who were interviewed while living in housing designed for homeless individuals or who reported that nighttime residences on the day of the survey or in the seven days before the interview were in an emergency shelter or transitional housing program, a hotel or motel paid for by a shelter voucher, an abandoned building, a place of business, a car or vehicle, or anywhere outside or if the last time they had "a place of [their] own for 30 days or more in the same place was more than seven days ago." Further details of the sampling method and the definition of homelessness are published elsewhere ( 15 , 16 ).
Sample
The NSHAPC public use file contains information from 4,207 adults, of whom 2,938 were designated as currently homeless. Among 849 currently homeless women, 111 (13%) had children only over 18 years old, 405 (48%) had children 18 years of age or under living with them, 183 (21%) had minor-age children living elsewhere, and 150 (18%) had never had children. This study analyzed service use patterns from currently homeless women with minor-age children who lived or did not live with them and women who never had children (a total sample of 738 women), allowing comparisons across those with and without symptoms of mental illness.
Measures
Symptoms of mental illness were measured by eight of the 11 items in the mental health component of the Addiction Severity Index ( 17 ) regarding experiences of serious depression; serious anxiety or tension; hallucinations; trouble understanding, concentrating, or remembering; trouble controlling violent behavior; serious thoughts of suicide; attempted suicide; and having taken prescribed medications for any psychological or emotional problem. Respondents were classified as having symptoms of mental illness if they reported having any symptoms of mental illness in the past 30 days.
Service use within the past 30 days served as our outcome variable and was measured by three dichotomous variables. Human service use included getting any assistance with basic needs (clothing and transportation), finance (managing money and obtaining public benefits), housing (finding affordable housing or assistance with rent, mortgage, or utilities), job seeking or training, parenting, legal advice, or help with domestic violence problems. Health care service use included treatment or examination by a doctor or nurse. Behavioral health service use included inpatient or outpatient treatment or counseling for emotional or mental problems and alcohol or drug problems.
Guided by Aday-Andersen's health services utilization model, we considered independent variables from three domains (predisposing, enabling, and need). The predisposing factors included age, ethnicity (white, black, Latino, or others), marital status (married or single), education (high school education completed or not), family status (mothers with minor-age children living with them, mothers with minor-age children not living with them, and women who never had children), and homeless status (short term, homeless for less than 365 days and only one episode; episodic, homeless for less than 365 days and two or more episodes; and chronic, homeless for more than 365 days).
The enabling factors included current health insurance (insured or not), receipt of public entitlement (including Aid to Families With Dependent Children, general assistance, Supplemental Security Income, food stamps, or a housing subsidy or housing assistance) in the past 30 days and geographic locale (rural or urban).
Need factors were measured by four dichotomous variables indicating the presence of any acute or chronic medical conditions and alcohol or drug dependence symptoms in the past 30 days. Respondents were asked if they had any infectious acute conditions, including chest infection, cough, cold, bronchitis, pneumonia, tuberculosis, gonorrhea, syphilis, herpes, chlamydia, other sexually transmitted infections (STIs) but not AIDS (other types of STIs are not specified in survey), or any noninfectious acute conditions such as skin disease, skin infection, skin sores, skin ulcers, lice, scabies, or other similar infestations. Chronic medical conditions included reports of diabetes, anemia, high blood pressure, heart disease or stroke, problems with the liver, arthritis, rheumatism, joint problems, cancer, problems walking, lost limb, other handicap, HIV positive, or AIDS.
Symptoms of alcohol problems included craving alcohol; adverse effects from alcohol; withdrawal symptoms from alcohol, such as seizures, shaking, or hallucinations; and desire to stop drinking but inability to do so. The same set of items was asked in regard to symptoms of drug problems.
Analyses
We used the weighting variable recommended by the Urban Institute to obtain parameter estimates at the national level ( 18 ). These weights adjust for the probability that respondents will be selected into each sampling level. To ensure respondent anonymity, geographic identifiers, such as sampling stratum, and primary sampling unit identifiers were removed from the public use data set. Therefore, standard error estimations that account for survey design could not be computed. However, we used a very stringent criterion of p<.001 for significance testing to avoid detection of spurious differences.
All analyses were conducted with SAS version 9.1.3. Chi square tests of independence were used to compare differences in sample characteristics between women with and without symptoms of mental illness. Multivariate logistic regressions were conducted to assess factors associated with behavioral, medical, and human service use separately for women with and without symptoms of mental illness, except for the model with behavioral health service use as the dependent variable, where only women with symptoms of mental illness or substance use problems were considered. The first model examined the associations of predisposing, enabling, and need factors with service use. The second model included service use in the other two service sectors as additional independent variables.
Results
Sample characteristics
Among the 738 homeless women in our sample, 320 (44%, weighted) reported having symptoms of mental illness in the past 30 days. Among the predisposing factors, those with symptoms of mental illness were more likely to be women who never had children or mothers not living with their children (p<.001) ( Table 1 ). Their homelessness was also more likely to be chronic or episodic rather than short term (p<.001), and they had lower rates of receipt of public entitlement (p<.001). Overall, women with symptoms of mental illness also were more likely to report an acute or chronic medical condition (p<.001), symptoms of alcohol problems (p<.001), and symptoms of drug problems (p<.001).
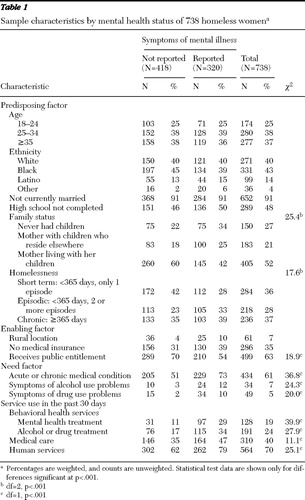 |
Service use patterns
Service use with the behavioral, medical, and human service sectors was consistently higher among homeless women with symptoms of mental illness than those without (p<.001) ( Table 1 ). Regardless of their mental health status, a majority of homeless women had human service contacts (79% and 62% for women with and without symptoms of mental illness, respectively). About half (47%) of the homeless women with symptoms of mental illness received medical services; however, rates for those without symptoms of mental illness were significantly lower (35%). Overall, 30% of those with symptoms of mental illness received behavioral health services in the past 30 days. However, 10% of the women who did not report symptoms of mental illness in the past month also received behavioral health care.
Medical care
Among homeless women without symptoms of mental illness, being single and never having children (odds ratio [OR]=6.11) or having less than a high school education (OR= 2.83) was positively associated with medical care service use in the past 30 days ( Table 2 ). Lack of health insurance (OR=.27) was negatively associated with use of medical care. Service contacts in the human service and behavioral health care sectors were not associated with use of medical care.
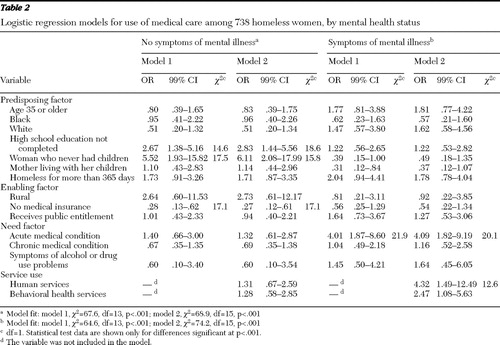 |
Among homeless women with symptoms of mental illness, presence of acute medical conditions (OR=4.09) and service contact with human service agencies (OR=4.32) were positively associated with use of medical care.
Human services
Among homeless women without symptoms of mental illness, chronic homelessness (OR=.31) and being single and never having children (OR=.25) were negatively associated with receiving human services ( Table 3 ). Behavioral health service use was positively associated with human service use (OR=2.93).
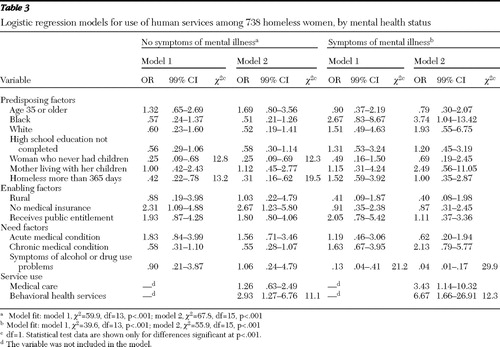 |
Among homeless women with symptoms of mental illness, presence of symptoms of alcohol or drug use problems was negatively associated with human service use (OR=.04). However, use of human services was higher among women who had received behavioral health services (OR=6.67).
Behavioral health services
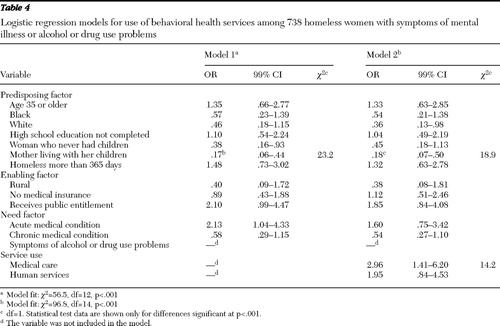
Among homeless women with symptoms of mental illness or substance use problems, being mothers living with their minor-aged children was negatively associated with behavioral health service use (OR=.18) ( Table 4 ). However, use of medical care was positively associated with receiving behavioral health services (OR=2.96).
 |
Discussion
Service use patterns
In this nationally representative sample of homeless persons, women with symptoms of mental illness consistently had more contacts across all three service domains (behavioral, medical, and human), indicating broad service utilization for this high-need group. There was a small group of women who had had no symptoms of mental illness in the past 30 days but had received behavioral health services. These women may have experienced a reduction in symptom severity as a result of behavioral health services.
Predictors of service use
Our findings indicate that predisposing and enabling variables were important predictors of service use among women without symptoms of mental illness, whereas need variables played a key role in determining service use among women with symptoms of mental illness. An important predisposing factor was the family situation that further describes women's circumstances. Homeless women living single without symptoms of mental illness were more likely to obtain medical services and less likely to receive human services. This finding suggests that there may be a larger infrastructure of human services available to women with children compared with single women, which may suggest an explanation for the quicker exits from homelessness of women living with children. Among homeless mothers with symptoms of mental illness or substance use problems, living with their minor-aged children was negatively associated with receiving behavioral health care. This might be due to the tendency of mothers to place a higher priority on their children's needs than on their own. Another possibility is that homeless mothers avoid contact with services from fear that their children will be removed by child protection services.
To ensure equitable access to services, attention should be given to the specific needs of women according to their family status by providing solutions to logistical barriers, such as child care, and engaging homeless mothers who might be fearful about losing custody. This fearfulness may be well founded; for example, as reported recently in a Los Angeles newspaper article, "the county Board of Supervisors has declared zero tolerance for families living on Skid Row [in Los Angeles] and is concentrating efforts on finding homes for children, even if that means children are eventually removed from their parents" ( 19 ).
Other predisposing factors related to service use among women without symptoms of mental illness were chronic homelessness and education. Symptoms of mental illness may be a trigger to provide services to some homeless women, but when homeless women do not have such obvious concerns, there is less impetus for providing care. Unfortunately this difference also may be due to funding streams' targeting subpopulations of homeless individuals, such as those with mental or physical health problems ( 20 ). In these situations, only individuals meeting the criteria of the funding streams qualify for services, and others may be left unserved. This inequity may be compounded by a lack of health insurance. Although it is well known that health insurance is associated with medical service use, this association is not always present with substance abuse treatment utilization ( 21 ). Consistent with these studies, we have found that health insurance status is associated with only the use of medical care but not behavioral or human services. This finding suggests that other factors such as perceived need for treatment and availability of free services might diminish the role of insurance in behavioral health service use.
Need factors played a key role in service use among homeless women with symptoms of mental illness. Having an acute medical condition increased the likelihood of getting medical care, which indicated more equitable access to medical care among women with symptoms than without. However, presence of alcohol or drug use problems was negatively associated with human service contact among homeless women with symptoms of mental illness. Providers may need to identify more effective ways to reach out and engage homeless women with comorbid mental disorders and substance use problems who might avoid human service contact out of fear or distrust.
Linkages of services
There was a positive association between use of behavioral health care services and human services for women with or without mental problems. Behavioral health care services seem to be the key for women who have substance use problems or symptoms of mental illness to connect with other types of services that may facilitate their exit from homelessness.
Evidence of linkages of services from different service sectors was more prominent among homeless women with symptoms of mental illness. Our findings suggest positive circular effects among behavioral services, human services, and medical services. Although the origination and causal direction of service connection cannot be ascertained with the cross-sectional data used in this study, the findings highlight a stronger, more integrated service delivery system that serves the needs of homeless women with mental health problems. An alternative explanation may be that some programs offer multidisciplinary providers, such as case management. No evidence for such service connection was found for women without mental health problems. It may be that some service sectors work better than others in providing service referrals. Future research is needed to optimize ways that all service sectors might serve the needs of various subgroups of homeless women.
This study is the first to describe service use patterns of homeless women across multiple service domains using nationally representative data. Findings in this study highlight important variations by subgroup and presence of symptoms of mental illness in service use patterns that have not been shown previously.
Study limitations
The age of the NSHAPC data is a limitation. However, the NSHAPC is the only nationally representative sample of homeless persons available today, and it provides a sufficiently large sample for meaningful analyses of subgroups of women. Although social change and policy change over the years may influence the point estimates of certain sample characteristics, we do not anticipate drastic changes in the strong associations reported in this study. Furthermore, findings from these data illuminate important baseline information on service use patterns that are essential for studies of change over time. Due to the cross-sectional design, findings suggest associations rather than causality. The survey relied on self-report data on sensitive issues such as mental health and substance use; consequently, recall bias and validity might be a concern.
Conclusions
Symptoms of mental illness may be a trigger for providing a wealth of services. As soon as homeless women with symptoms of mental illness gained entrance into a service system, they received many different types of services. In this situation, homeless women who did not have symptoms of mental illness were at a disadvantage.
Homeless mothers who had symptoms of mental illness or substance use problems and were living with their minor-aged children faced other barriers to services. Although they may have realized their need for assistance, gaining entrance to behavioral or other services may have increased their vulnerability to child welfare services intervention. Thus there may be a catch-22 situation—homeless mothers who have symptoms of mental illness or substance use problems and live with their minor-aged children need services to benefit themselves and their children, but attention from those very services may allow scrutiny that will involve child welfare services. Unfortunately the lack of mental health services for the mother may increase the risk to the children. This cycle needs attention. Policy makers, researchers, and providers need to identify systems that promote family maintenance while providing treatment.
Acknowledgments and disclosures
This study was funded by Substance Abuse Policy and Research Program 52826 from the Robert Wood Johnson Foundation.
The authors report no competing interests.
1. Burt MR, Aron LY, Lee E: Helping America's Homeless: Emergency Shelter or Affordable Housing? Washington, DC, Urban Institute Press, 2001Google Scholar
2. Aday L, Andersen RM: A framework for the study of access to medical care. Health Services Research 9:208–220, 1974Google Scholar
3. Andersen R, Newman JP: Societal and individual determinants of medical utilization in the United States. Milbank Memorial Fund Quarterly 51:95–124, 1973Google Scholar
4. Andersen RM: Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36:1–10, 1995Google Scholar
5. Padgett D, Struening E, Andrews H: Factors affecting the use of medical, mental health, alcohol, and drug treatment services by homeless adults. Medical Care 28: 805–821, 1990Google Scholar
6. Gallagher TC, Andersen RM, Koegel P, et al: Determinants of regular source of care among homeless adults in Los Angeles. Medical Care 35:814–830, 1997Google Scholar
7. Gelberg L, Andersen RM, Leake BD: The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Services Research 34:1273–1302, 2000Google Scholar
8. Stein JA, Andersen RM, Koegel P, et al: Predicting health services utilization among homeless adults: a prospective analysis. Journal of Health Care for the Poor and Underserved 11:212–230, 2000Google Scholar
9. Bird CE, Jinnett KJ, Burnam MA, et al: Predictors of contact with public service sectors among homeless adults with and without alcohol and other drug disorders. Journal of Studies on Alcohol 63:716–725, 2002Google Scholar
10. Stein JA, Andersen RM, Gelberg L: Applying the Gelberg-Andersen behavioral model for vulnerable populations to health services utilization in homeless women. Journal of Health Psychology 12:791–804, 2007Google Scholar
11. Zlotnick C, Robertson MJ, Lahiff M: Getting off the streets: economic resources and residential exits from homelessness. Journal of Community Psychology 27:209–224, 1999Google Scholar
12. Zlotnick C, Robertson MJ, Lahiff M: A longitudinal perspective on entitlement income among homeless adults. Psychiatric Services 49:1039–1042, 1998Google Scholar
13. Bassuk EL, Weinreb LF, Buckner JC, et al: The characteristics and needs of sheltered homeless and low-income housed mothers. JAMA 276:640–646, 1996Google Scholar
14. Tourkin S, Hubble D: National Survey of Homeless Assistance Providers and Clients: Data Collection Methods. Washington, DC, Urban Institute Press, 1997Google Scholar
15. Burt MR, Aron LY, Douglas T, et al: Homelessness: Programs and the People They Serve: Findings of the National Survey of Homeless Assistance Providers and Clients. Washington, DC, Urban Institute Press, 1999Google Scholar
16. Zlotnick C, Tam T, Bradley K: Adulthood trauma, separation from one's children and homeless mothers. Community Mental Health Journal 43:20–33, 2007Google Scholar
17. McLellan TA, Kushner H, Metzger D, et al: The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:199–213, 1992Google Scholar
18. Burt MR, Aron LY, Douglas T, et al: Homelessness: Programs and the People They Serve—Technical Report. Washington, DC, Urban Institute Press, 1999Google Scholar
19. Leonard J: LA: moving people off Skid Row, finding homes for kids. San Francisco Chronicle, May 6, 2007, p B-1Google Scholar
20. Notice of funding availability for the Collaborative Initiative to help end chronic homelessness. Federal Register 68:4018–4046, 2003Google Scholar
21. Schmidt L, Weisner C: Private insurance and the utilization of chemical dependency treatment. Journal of Substance Abuse Treatment 28:67–76, 2005Google Scholar



