Guideline-Consistent Antidepressant Treatment Patterns Among Veterans With Diabetes and Major Depressive Disorder
The prevalence of depression among persons with diabetes is very high and ranges from as low as 11%, when standardized diagnostic interviews are used, to as high as 31%, when assessed by questionnaires ( 1 ). Comorbid depression complicates diabetes care and adversely affects health care expenditures and clinical outcomes. Specifically, co-occurring depression as measured by using symptom scales or diagnostic criteria is associated with hyperglycemia ( 2 ), has been shown to lower adherence to oral hypoglycemic and lipid-lowering medications ( 3 ), and is associated with functional disability ( 4 ). Total health care expenditures of individuals with self-reported depression and diabetes are 4.5 times higher than those of individuals with diabetes without depression ( 5 ).
However, clinical trials have shown that pharmacologic treatments, specifically the new-generation antidepressants, and nonpharmacologic treatments for major depression tend to improve glycemic control ( 6 , 7 ). In a randomized double-blind placebo-controlled trial of patients with comorbid diabetes and depression, fluoxetine, as compared with a placebo, was associated with better glycemic control and reduced depressive symptoms ( 7 ).
Recent studies have documented cost advantages of treating depression among individuals with diabetes. A one-year cross-sectional observational study found that antidepressant treatment was associated with increased adherence to cardiovascular medications among individuals with diabetes and cardiovascular conditions and found that adherent patients had lower medical charges ( 8 ). A randomized controlled trial of individuals with diabetes and depression that compared a systematic depression treatment program (beginning with either problem-solving psychotherapy or a structured antidepressant pharmacotherapy program) with care as usual found that systematic depression treatment significantly reduced the cost per patient ( 9 ).
However, much remains unknown about treatment patterns for depression among individuals with diabetes and depression. Only a handful of studies have examined depression treatment among patients with diabetes and depression. Some of these studies reported very low rates of depression treatment. Among Latinos with diabetes, less than one-half of the patients with moderate or severe depression identified from self-reported symptoms received mental health treatment ( 10 ). Using 1995 Medicaid data from four states, Sambamoorthi and colleagues ( 11 ) found that among Medicaid beneficiaries with diagnosed depression and diabetes, there were significant gender, racial and ethnic, and age variations in depression treatment. Using data from a single site of the Veterans Health Administration (VHA), Jones and colleagues ( 12 , 13 ) suggested that although diabetes did not affect depression care, antidepressant treatment duration fell short of guideline recommendations, with 11% receiving adequate duration of treatment. In another study, among individuals with diabetes and diagnosed depression, only one-third were adherent to antidepressant medications ( 8 ).
The added beneficial effects of depression treatment among individuals with diabetes in improving adherence to cardiovascular medications and lower medical charges can only be realized when depression treatment rates are high and there are no subgroup differences in depression treatment. Therefore, understanding the treatment patterns will be the first step toward identifying subgroup differences in treatment to help inform strategies for increasing treatment access and realizing cost-savings associated with depression treatment. Therefore, the primary objective of this article is to examine patterns of any antidepressant treatment and of guideline-consistent antidepressant treatment among patients with diabetes and diagnosed depression by using a merged nationwide VHA and Medicare database.
Methods
Data
We used the merged VHA and Medicare database of the Diabetes Epidemiology Cohort (DEpiC), a multiyear, dynamic cohort of individuals with diabetes who use the VHA for health care. Details of identification and construction of the cohort are described elsewhere ( 14 ). We used the cohort of VHA clinic users with diabetes who were identified between fiscal year (FY) 1998 and FY 1999. Patients enrolled in Medicare health maintenance organizations (HMOs) were not included in the cohort. This study was approved by the Veterans Affairs New Jersey Health Care System (VANJHCS) Institutional Review Board (a subcommittee of the VANJHCS Research and Development Committee) and the VANJHCS Research and Development Committee.
Identification of veterans with diabetes and major depression
We required a VHA clinic user with diabetes to have a face-to-face encounter with a clinician that resulted in a diagnosis of a major depressive disorder ( 15 ). Diagnosis of a major depressive disorder was based on the following International Classification of Diseases 9th Clinical Modification ( ICD-9-CM ) codes: 296.2 (major depressive disorder, single episode) and 296.3 (major depressive disorder, recurrent episode). We restricted our analysis to those with major depressive disorder because there are established guidelines for its pharmacological treatment ( 16 ). We identified 16,449 veterans who were VHA clinic users with diabetes and had at least one face-to-face encounter with a clinician that resulted in a diagnosis of a major depressive disorder. In the rest of the article, unless otherwise specified, depression refers to diagnosed major depressive disorder.
Some individuals treated for depression during the period of available data may have had episodes of depression treatment that began before the start of our observation period (October 1, 1998). Therefore, we distinguished between prior episodes of depression and incident depression by using adapted criteria from the National Committee for Quality Assurance (NCQA)—that is, a 120-day (four-month) "negative diagnosis history" on or before the first observed depression diagnosis date and a 120-day (four-month) "negative medication history" on or before the first observed prescription date ( 17 ). On the basis of these criteria, we identified 3,953 VHA users with diabetes and an incident diagnosis of major depressive disorder between February 1, 1999, and September 30, 1999, using a four-month negative diagnosis and negative medication history between October 1, 1998, and January 30, 1999. These individuals were followed for six months (180 days) from the time of the incident depression diagnosis.
Dependent variables
Receipt of any antidepressant. Prescribed medications were obtained from pharmacy files, and antidepressant medications were identified through drug names. Among individuals with diabetes and incident depression, any individual with at least one prescription for antidepressant medications on or after the depression diagnosis date was considered to be receiving antidepressant treatment for depression. It should be noted that we evaluated only the filling of the prescription, not its actual use by the patient.
Guideline-consistent antidepressant treatment. We defined guideline-consistent antidepressant treatment of depression in terms of duration, because discontinuation in terms of duration has been associated with 30% to 50% of relapses ( 18 ). We did not assess dosage adequacy because prior work by VHA investigators indicated that an overwhelming majority of VHA patients (90%) attained dosage adequacy ( 19 ). Our measure of guideline-consistent antidepressant treatment was derived from duration of medication use, which was based on the NCQA's Health Plan Employer Data and Information Set (HEDIS) report on antidepressant medication management ( 17 ). On the basis of prior publications in the VHA ( 19 , 20 ) and guidelines for the treatment of major depression ( 21 ), we defined patients as receiving guideline-consistent antidepressant treatment if they were treated with antidepressant medications for at least three months within a six-month (180 days) follow-up period after diagnosis. The mean±SE number of days per prescription within the 180 days was 31.8±14.0, with only 5.7% having 90-day prescriptions.
Independent variables
Independent variables consisted of veterans' demographic characteristics, economic characteristics, access to care, and health status measured during FY 1999. In addition, we used glycemic control and use of antiglycemic medications before the incident depression diagnosis date as independent variables to explain variations in guideline-consistent treatment.
Demographic characteristics were represented by gender, race or ethnicity (white, African American, Latino, and other), age (under 50 years, 50–64 years, 65–74 years, and 75 and older), and marital status (married versus others). Priority group status in the VHA was used to measure coverage: service-connected disability >30% (VHA priority groups 1 and 4), service-connected disability <20% (groups 2, 3, and 6), low income (group 5), and high income (group 7). Measures of health status included physical comorbidity, other mental illness, and substance abuse. Physical comorbidity was measured by the Charlson Comorbidity Index (CCI) derived from ICD-9-CM codes ( 22 , 23 ). Other mental disorders included schizophrenia ( ICD-9 295), other psychoses ( ICD-9 296.3, 297.0, and 298.0), bipolar disorder ( ICD-9 296.0, 296.1, and 296.4–296.8), anxiety disorders ( ICD-9 300.0, 300.2, 300.3, and 308.3), and posttraumatic stress disorder (PTSD) ( ICD-9 309.81). Substance use disorders included presence of substance abuse and dependence (alcohol, tobacco, and drugs), by ICD-9 codes 304, 303, and 305.
Access-to-care variables. Access-to-care variables included dual VHA and Medicare use and mental health specialty sector care. For veterans using the VHA, Medicare is an important source of health care coverage ( 24 , 25 , 26 , 27 ). Although Medicare did not cover prescription drugs during our observation period, it is possible that dual use may lead to fragmented care and such fragmented care may result in reduced access or continuation of treatment because of the difficulty in coordinating care between the two systems.
Patients treated by psychiatrists in the mental health specialty sector tend to have more severe mental disorders than patients treated by other health care professionals ( 28 ). In addition, receipt of mental health specialty care is strongly associated with improved adherence to medications ( 29 , 30 , 31 ). In Medicare, provider specialty codes 26, 62, 80, and 86 represented visits to psychiatrists, psychologists, and clinical social workers. In VHA files, clinic stop codes were used to identify mental health specialty care. This measure was defined as use either at the start or during the incident depression treatment episode.
Antiglycemic medications and glycemic control. Concerns have been raised about the negative impact of tricyclic antidepressants on glycemic control ( 32 ). We measured glycemic control with hemoglobin A1c (HbA1c) values before the incident depression diagnosis date. We used stratification values based on guidelines suggested by the American Diabetes Association and the VA-Department of Defense ( 33 )—that is, we stratified HbA1c values taken before the incident depression into one of three groups: <7% (optimal control), 7%–9% (good or fair control), and >9% (poor control). For those who did not have an HbA1c test, we included an indicator variable. Antiglycemic medication use before the incident depression diagnosis date was grouped into four classes: no oral medication or insulin use, oral medication use only, insulin use only, and both oral medication and insulin use. Because an overwhelming majority (95%) of individuals were prescribed the new-generation antidepressant medications, we did not control for type of antidepressant medication use.
Statistical procedures
Chi square tests were used to test unadjusted subgroup differences in dependent variables. Logistic regressions were used to examine the patterns of any treatment and guideline-consistent treatment by demographic characteristics (gender, race or ethnicity, and marital status), economic characteristics (VHA priority status), access to care (dual VHA and Medicare use and mental health specialty care), health status (physical comorbidity and other mental illness), and other characteristics (HbA1c control and substance abuse). The parameter estimates were converted to odds ratios and their associated 95% confidence intervals (CIs).
Results
Table 1 describes VHA users with incident major depressive disorder and diabetes. The study population was overwhelmingly male (96%) and white (73%); 19% were African American and 7% were Latino. The median age was 64 years, and 47% of the VHA patients were over the age of 65 years. A majority of veterans (52%) were eligible for VHA enrollment because of their low income. Over half (60%) the study population had dual Medicare and VHA use. Only 2% of the study population did not have other physical illnesses, according to their CCI score. Anxiety disorders were the most common psychiatric comorbid condition (20%), followed by PTSD (15%). Over half (54%) did not have an HbA1c test before the date of their incident depression diagnosis, and 12% had poor HbA1c control.
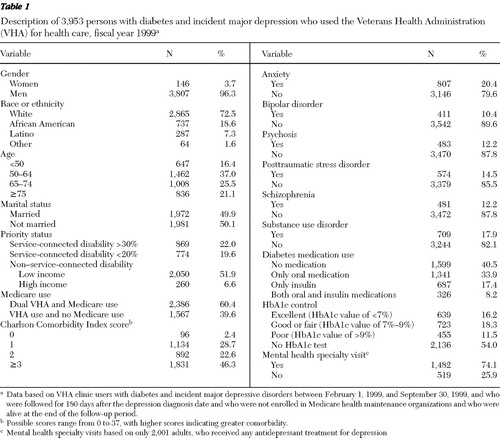 |
Among VHA users with diabetes and incident depression, 51% (N= 2,001) had at least one prescription for an antidepressant. In the multivariate analysis, the significant predictors were African-American race, older age, marital status, VHA priority group status, psychiatric comorbidities (except anxiety disorders and PTSD), diabetes medication use, and treatment by a mental health specialist ( Table 2 ). African Americans were less likely than whites to have an antidepressant prescription filled (adjusted odds ratio [AOR]=.81, p<.05). Veterans over age 65 were less likely than individuals younger than 50 years to be treated with antidepressants for depression (p<.001). Those who were seen in the mental health specialty care sector were twice as likely as those seen in primary care to fill an antidepressant prescription (AOR=2.19, 95% p<.001). Those who had a prescription for oral antiglycemic agents alone were more likely than those with no prescription for oral antiglycemic agents alone to fill an antidepressant prescription (AOR=1.27, p<.01). Prior glycemic control was not associated with the likelihood of receiving antidepressant treatment.
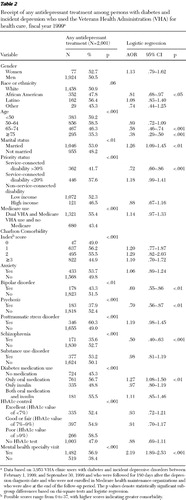 |
Among veterans with incident depression and diabetes who were treated with antidepressants, 62% had guideline-consistent treatment. Among all VHA users with diabetes and incident depression, this translates into an overall share of 31.4%. Significant predictors of guideline-consistent treatment were African-American race, older age (75 years or older), marital status, substance use disorders, and being seen in the mental health specialty sector ( Table 3 ). African-American race had a negative association with the likelihood of receipt of guideline-consistent treatment, compared with whites (AOR= .64, p<.001). Those who were seen in the mental health specialty sector were more likely than those who were not seen in that sector to receive guideline-consistent treatment (AOR= 1.62, p<.001). None of the psychiatric comorbidities were associated with the likelihood of guideline-consistent antidepressant treatment. Individuals with substance use disorders were less likely to receive guideline-consistent treatment, compared with those who did not have a diagnosis of substance use disorder.
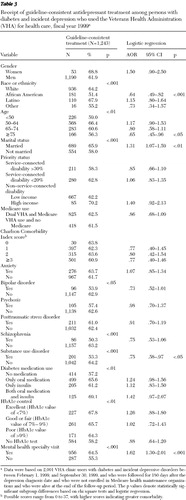 |
In assessing guideline-consistent antidepressant treatment, we counted a veteran who was given a 90-day prescription as having guideline-consistent treatment for depression. To ensure the robustness of the findings, we excluded 71 individuals whose first prescription was for a 90-day supply. Even with the exclusion of these individuals, our bivariate and multivariate findings remained consistent with those reported in the main analysis.
Because guideline-consistent treatment for depression may be related to treatment versus no treatment, a joint choice model was used to analyze treatment and continuity within a multivariate framework. An approach that accounts for the dependence between seeking treatment for depression and guideline-consistent treatment is the maximum likelihood model with selection. This specification jointly models the probability of choosing treatment and the probability of continuing treatment. This was implemented through the heckprob procedure in Stata, version 8 ( 34 ). For identification purposes, we also included additional variables (metropolitan area versus nonmetropolitan area and U.S. region [Northeast, West, Midwest, and South]) in modeling any depression treatment. The guideline-consistent treatment equation did not contain metropolitan area and U.S. region variables. The estimated models indicated that the correlation term between the two equations (rho) was not significantly different from zero ( χ2 =.33, p < χ2 =.57), suggesting that the outcomes (any treatment and continuation of treatment) could be modeled separately. Therefore, findings are based on separate regressions on any treatment and guideline-consistent treatment among those who received any antidepressants for depression treatment.
Since the publication of guidelines established by the National Depression Panel, the NCQA has developed a quality compass to establish standardized specifications and implementation of guidelines for many conditions. These guidelines are based on data gathered from HEDIS ( 35 ). NCQA's set of depression management indicators are from administrative databases in over 300 health plans and measure the population in treatment—that is, diagnosed patients who initiate antidepressant medication. NCQA has established criteria for measuring treatment of depression for adults diagnosed as having a new episode of depression and initiated on an antidepressant drug and who received a continuous trial of medication treatment during the acute treatment phase ( 36 ). The NCQA criteria include individuals diagnosed as having a new episode of major depression ( ICD-9-CM codes 296.2, 296.3, 298.0, 300.4, 309.1, and 311). Therefore, we also conducted all analyses with the broader criteria of depression diagnosis. We found that patterns were generally consistent for any antidepressant treatment and guideline-consistent antidepressant treatment. (Findings from these analyses are available from the first author on request.)
Discussion
Ours is the first nationwide study to analyze antidepressant treatment patterns among veterans with diabetes and an incident depression diagnosis. Because there have been no other nationwide studies that deal with depression treatment among adults with diabetes in the VHA, we were not able to directly compare treatment rates from our study with others. However, we did find that compared with a single-facility study that examined veterans with diabetes and depression ( 12 , 13 ), our nationwide study had higher rates of receipt of any antidepressant treatment and treatment duration; our study also had higher rates than a study of the general population ( 37 ). Guideline-consistent treatment rates in our study population were lower than the 85% observed in the general population of VHA users with major depression ( 20 ). By using a nationally representative household survey, it was found that early discontinuation of antidepressant therapy is widespread in the general population with depression, with only 27.6% of the patients continuing antidepressant therapy for more than 90 days ( 37 ). Katon and colleagues ( 8 ) found that only 36.3% of primary care patients had continued treatment for depression for 180 days.
Although receiving care in the mental health specialty sector was associated with a higher likelihood of receiving any treatment and guideline-consistent treatment, opportunities do exist to improve guideline-consistent antidepressant treatment among VHA clinic users with diabetes. There is emerging evidence that collaborative care was significantly more successful at reducing depressive symptoms than usual primary care among patients with diabetes ( 38 ). Indeed, increased primary care-mental health subspecialty care paradigms are being introduced within the VHA, which may be one way to increase guideline-consistent depression treatment among VHA users with diabetes and major depressive disorder ( 39 ).
The antidepressant prescription patterns suggest that specific comorbid mental disorders, including bipolar disorder, schizophrenia, and psychoses, were associated with lower rates of any antidepressant treatment and that substance use disorders were negatively associated with guideline-consistent antidepressant treatment. Although the reasons for these patterns remain unclear, antidepressant treatment of bipolar disorder increases the risk of treatment-emergent mania or hypomania ( 40 ), and the clinical role of antidepressants in the management of schizophrenia is limited ( 41 ). In addition, prior research has linked substance use disorders ( 42 ) and schizophrenia ( 43 ) with increased risk of antidepressant nonadherence.
Lack of an association between antidepressant treatment and poor glycemic control and the finding that a majority of individuals were on new-generation antidepressants together suggest that poor glycemic control was not a barrier to treatment. Increased use of antidepressants was observed among veterans on oral hypoglycemic medications. A plausible explanation could be that veterans are highly likely to be adherent to hypoglycemic medication. Because they have high adherence to one type of medication, they may also have high adherence to any type of prescribed medication, regardless of type of medication.
The demographic differences with respect to African-American race and older age are consistent with the existing research. As in other depression-related research ( 44 ), African Americans were less likely to receive any treatment. On the one hand, our observations are consistent with earlier work indicating that racial differences persist even when insurance status and socioeconomic status are controlled for ( 45 ). Although not specific to diabetes or the VHA, previous research suggests that persons from racial or ethnic minority groups are more likely than whites to report major depression without medication use ( 46 ). In clinical settings, white patients with major depression were nearly three times more likely than nonwhite patients with major depression to receive a recommendation for an antidepressant medication and almost twice as likely to have been treated with one ( 47 ). Despite the increase in office-based prescription of antidepressants between 1992–1993 and 1994–1995, prescription rates for African-American and Hispanic patients were less than half the rate for whites ( 48 , 49 ). Even among a poor nonelderly sample with Medicaid, racial variations in access to selective serotonin reuptake inhibitors and other antidepressants have been documented ( 50 , 51 ). However, in the VHA, racial differences are not consistent across indicators or illnesses. For example, in a study among veterans racial differences were found in some measures and not in others ( 52 ).
An increasing trend in physician recognition of depression among the elderly over 65 years of age has been documented ( 53 ). However, our finding that older individuals were less likely to be treated with antidepressants for depression is consistent with other studies in which less than one-third of elderly primary care patients diagnosed as having depression received an antidepressant ( 54 ).
The strengths of our study are a nationwide database, availability of detailed pharmacy information, comprehensive diagnostic information from both VHA and Medicare, and information on glycemic control that is not typically available in administrative databases. However, some study limitations need to be noted. A limitation that is common to all studies that focus on the veteran population is that the study population is primarily elderly, low-income, male veterans who have higher rates of comorbid physical conditions and mental disorders. This limits the generalizability of the results. Our data include only individuals with diagnosed depression and cannot capture undiagnosed depression ( 55 , 56 , 57 ). It is known that depression may be undercoded ( 58 ). Yet another limitation is our inability to capture service use in Medicare HMOs, an important source of health care delivery for veterans ( 59 ). However, an examination of a profile of individuals with HMO enrollment did suggest similar gender and racial or ethnic composition and VHA enrollment status.
Although the data terminate in 2000, they have been extensively validated ( 60 , 61 ) and permit comparison with other studies from the same period. In addition, the results will serve as a baseline against which to measure secular change. The two studies by Jones and colleagues ( 12 , 13 ), which used data from January 1997 through April 2005, show that 63% of VHA users with depression did not receive antidepressants within six weeks of a depression diagnosis. Although these studies did not model depression treatment patterns among those with diabetes and major depression, racial differences (p=.06) were apparent in the study.
Conclusions
Despite our study's limitations, our findings suggest that even in a health care system that has generous pharmacy benefits and where access is equalized, guideline-consistent depression care is lower for certain subgroups of individuals. Further research is necessary to evaluate the reasons for this finding. Our study results do point to opportunities, such as mental health specialty care, that exist for improving antidepressant treatment among veterans with diabetes and depression.
Acknowledgments and disclosures
This research was supported by grants IIR 05-016, IEA-05-255 (principal investigator, Dr. Sambamoorthi), and REA-03-021 (principal investigator, Dr. Pogach) from the Department of Veterans Affairs Health Services Research and Development Service. The findings and opinions reported here are those of the authors and do not necessarily represent the views of any other individuals or organizations.
The authors report no competing interests.
1. Anderson RJ, Freedland KE, Clouse RE, et al: The prevalence of comorbid depression in adults with diabetes: a meta analysis. Diabetes Care 6:1069–1078, 2001Google Scholar
2. Lustman PJ, Anderson RJ, Freedland KE, et al: Depression and poor glycemic control: a meta-analytic review of the literature. Diabetes Care 7:934–942, 2000Google Scholar
3. Lin EH, Katon W, Von Korff M, et al: Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care 9:2154–2160, 2004Google Scholar
4. Egede LE: Diabetes, major depression, and functional disability among US adults. Diabetes Care 2:421–428, 2004Google Scholar
5. Egede LE, Zheng D, Simpson K: Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 3:464–470, 2002Google Scholar
6. Lustman PJ, Freedland KE, Griffith LS, et al: Predicting response to cognitive behavior therapy of depression in type 2 diabetes. General Hospital Psychiatry 5:302–306, 1998Google Scholar
7. Lustman PJ, Freedland KE, Griffith LS, et al: Fluoxetine for depression in diabetes: a randomized double-blind placebo-controlled trial. Diabetes Care 5:618–623, 2000Google Scholar
8. Katon W, Cantrell CR, Sokol MC, et al: Impact of antidepressant drug adherence on comorbid medication use and resource utilization. Archives of Internal Medicine 21: 2497–2503, 2005Google Scholar
9. Simon JE, Katon WJ, Lin EH, et al: Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Archives of General Psychiatry 1:65–72, 2007Google Scholar
10. Gross R, Olfson M, Gameroff MJ, et al: Depression and glycemic control in Hispanic primary care patients with diabetes. Journal of General Internal Medicine 5:460–466, 2005Google Scholar
11. Sambamoorthi U, Olfson M, Wei W, et al: Diabetes and depression care among Medicaid beneficiaries. Journal of Health Care for the Poor and Underserved 1:141–161, 2006Google Scholar
12. Jones LE, Turvey C, Torner JC, et al: Nonadherence to depression treatment guidelines among veterans with diabetes mellitus. American Journal of Managed Care 12: 701–710, 2006Google Scholar
13. Jones LE, Turvey C, Carney-Doebbeling C: Inadequate follow-up care for depression and its impact on antidepressant treatment duration among veterans with and without diabetes mellitus in the Veterans Health Administration. General Hospital Psychiatry 6:465–474, 2006Google Scholar
14. Miller DR, Safford MM, Pogach LM: Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care 27(suppl 2):B10–B21, 2004Google Scholar
15. Spettell CM, Wall TC, Allison J, et al: Identifying physician-recognized depression from administrative data: consequences for quality measurement. Health Services Research 4:1081, 2003Google Scholar
16. Ackermann RT, Williams JW Jr: Rational treatment choices for non-major depressions in primary care: an evidence-based review. Journal of General Internal Medicine 4:293–301, 2002Google Scholar
17. HEDIS 2008: Healthcare Effectiveness Data and Information Set: Vol 2, Technical Specifications. Washington, DC, National Committee for Quality Assurance (NCQA), July 2007. Available at www.qualitymeasures.ahrq.gov/summary/summary.aspx?ss=1&docid=10059Google Scholar
18. Montgomery SA: Antidepressants in long-term treatment. Annual Review of Medicine 45:447–457, 1994Google Scholar
19. Charbonneau A, Rosen AK, Ash AS, et al: Measuring the quality of depression care in a large integrated health system. Medical Care 5:669–680, 2003Google Scholar
20. Busch SH, Leslie D, Rosenheck R: Measuring quality of pharmacotherapy for depression in a national health care system. Medical Care 6:532–542, 2004Google Scholar
21. Depression Guideline Panel. Depression in Primary Care: Vol 2. Treatment of Depression, Clinical Practice Guideline Number 5. AHCPR pub no 93-0551. Rockville, Md, Agency for Healthcare Policy and Research, 1993Google Scholar
22. Charlson ME, Pompei P, Ales KL, et al: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of Chronic Diseases 40:373–383, 1987Google Scholar
23. Deyo RA, Cherkin DC, Ciol MA: Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology 45:613–619, 1992Google Scholar
24. Weeks WB, Mahar PJ, Wright SM: Utilization of VA and Medicare services by Medicare-eligible veterans: the impact of additional access points in a rural setting. Journal of Healthcare Management 50:95–106, 2005Google Scholar
25. Shen Y, Hendricks A, Zhang S, et al: VHA enrollees' health care coverage and use of care. Medical Care Research and Review 60:253–267, 2003Google Scholar
26. Borowsky SJ, Cowper DC: Dual use of VA and non-VA primary care. Journal of General Internal Medicine 14:274–280, 1999Google Scholar
27. Wright SM, Daley J, Fisher ES, et al: Where do elderly veterans obtain care for acute myocardial infarction: Department of Veterans Affairs or Medicare? Health Services Research 6:739–754, 1997Google Scholar
28. Wells KB, Burnam MA, Camp P: Severity of depression in prepaid and fee-for-service general medical and mental health specialty practices. Medical Care 4:350–364, 1995Google Scholar
29. Robinson RL, Long SR, Chang S, et al: Higher costs and therapeutic factors associated with adherence to NCQA HEDIS antidepressant medication management measures: analysis of administrative claims. Journal of Managed Care Pharmacy 1:43–54, 2006Google Scholar
30. Stein MB, Cantrell CR, Sokol MC, et al: Antidepressant adherence and medical resource use among managed care patients with anxiety disorders. Psychiatric Services 5:673–680, 2006Google Scholar
31. Croghan TW, Melfi CA, Dobrez DG, et al: Effect of mental health specialty care on antidepressant length of therapy. Medical Care 37(suppl 4):AS20–AS23, 1999Google Scholar
32. Lustman PJ, Griffith LS, Clouse RE, et al: Effects of nortriptyline on depression and glycemic control in diabetes: results of a double-blind, placebo-controlled trial. Psychosomatic Medicine 3:241–250, 1997Google Scholar
33. American Diabetes Association: Standards of medical care for patients with diabetes mellitus. Diabetes Care 28(suppl 1):S4–S36, 2005Google Scholar
34. Stata Statistical Software: Release 8.0. College Station, Tex, Stata Corp, 2003Google Scholar
35. Thompson JW, Bost J, Ahmed F, et al: The NCQA's quality compass: evaluating managed care in the United States. Health Affairs 1:152–158, 1998Google Scholar
36. National Healthcare Quality Report, 2006: Effectiveness of Care: Mental Health and Substance Abuse: Measure Specifications Appendix. Rockville, Md, Agency for Healthcare Research and Quality. Available at www.ahrq.gov/qual/nhqr06/measurespec/mentalh.htmGoogle Scholar
37. Olfson M, Marcus SC, Tedeschi M, et al: Continuity of antidepressant treatment for adults with depression in the United States. American Journal of Psychiatry 1:101–108, 2006Google Scholar
38. Kinder LS, Katon WJ, Ludman E, et al: Improving depression care in patients with diabetes and multiple complications. Journal of General Internal Medicine 10:1036–1041, 2006Google Scholar
39. Felker BL, Chaney E, Rubenstein LV, et al: Developing effective collaboration between primary care and mental health providers. Primary Care Companion to the Journal of Clinical Psychiatry 1:12–16, 2006Google Scholar
40. Truman CJ, Goldberg JF, Ghaemi SN et al: Self-reported history of manic/hypomanic switch associated with antidepressant use: data from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BP). Journal of Clinical Psychiatry 68:1472–1479, 2007Google Scholar
41. Levinson DF, Umapathy C, Musthaq M: Treatment of schizoaffective disorder and schizophrenia with mood symptoms. American Journal of Psychiatry 156:1138–1148, 1999Google Scholar
42. Akincigil A, Bowblis JR, Levin C, et al: Adherence to antidepressant treatment among privately insured patients diagnosed with depression. Medical Care 45:363–369, 2007Google Scholar
43. Svarstad BL, Shireman TI, Sweeney JK: Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatric Services 52:805–811, 2001Google Scholar
44. Harman JS, Edlund MJ, Fortney JC: Disparities in the adequacy of depression treatment in the United States. Psychiatric Services 12:1379–1385, 2004Google Scholar
45. Skaer TL, Robison LM, Sclar DA, et al: Use of antidepressant pharmacotherapy within the first year after diagnosis of diabetes mellitus: a study of a Medicaid population. Current Therapeutic Research 8: 415–422, 1999Google Scholar
46. Green-Hennessy S, Hennessy KD: Demographic differences in medication use among individuals with self-reported major depression. Psychiatric Services 2:257–259, 1999Google Scholar
47. Sirey JA, Meyers BS, Bruce ML, et al: Predictors of antidepressant prescription and early use among depressed outpatients. American Journal of Psychiatry 5:690–696, 1999Google Scholar
48. Sclar DA, Robinson LM, Skaer TL, et al: Trends in the prescribing of antidepressant pharmacotherapy: office-based visits, 1990–1995. Clinical Therapeutics 4:871–884, 1998Google Scholar
49. Sclar DA, Robison LM, Skaer TL, et al: Ethnicity and the prescribing of antidepressant pharmacotherapy: 1992–1995. Harvard Review of Psychiatry 1:29–36, 1999Google Scholar
50. Melfi CA, Croghan TW, Hanna MP, et al: Racial variation in antidepressant treatment in a Medicaid population. Journal of Clinical Psychiatry 1:16–21, 2000Google Scholar
51. Melfi CA, Croghan TW, Hanna MP: Access to treatment for depression in a Medicaid population. Journal of Health Care for the Poor and Underserved 2:201–215, 1999Google Scholar
52. Heisler M, Smith DM, Hayward RA, et al: Racial disparities in diabetes care processes, outcomes, and treatment intensity. Medical Care 11:1221–1232, 2003Google Scholar
53. Crystal S, Sambamoorthi U, Walkup JT, et al: Diagnosis and treatment of depression in the elderly Medicare population: predictors, disparities, and trends. Journal of the American Geriatrics Society 12:1718–1728, 2003Google Scholar
54. Luber MP, Meyers BS, Williams-Russo PG, et al: Depression and service utilization in elderly primary care patients. American Journal of Geriatric Psychiatry 2:169–176, 2001Google Scholar
55. Wells KB, Hays RD, Burnam MA, et al: Detection of depressive disorder for patients receiving prepaid or fee-for-service care: results from the Medical Outcomes Study. JAMA 23:3298–3302, 1989Google Scholar
56. Garrard J, Rolnick SJ, Nitz NM, et al: Clinical detection of depression among community-based elderly people with self-reported symptoms of depression. Journals of Gerontology: Series A, Biological Sciences and Medical Sciences 2:M92–M101, 1998Google Scholar
57. Williams JW Jr, Mulrow CD, Kroenke K, et al: Case-finding for depression in primary care: a randomized trial. American Journal of Medicine 1:36–43, 1999Google Scholar
58. Rost K, Smith R, Matthews DB, et al: The deliberate misdiagnosis of major depression in primary care. Archives of Family Medicine 4:333–337, 1994Google Scholar
59. Shen Y, Hendricks A, Li D, et al: VA-Medicare dual beneficiaries' enrollment in Medicare HMOs: access to VA, availability of HMOs, and favorable selection. Medical Care Research and Review 62:479–495, 2005Google Scholar
60. Kerr EA, Smith DM, Hogan MH, et al: Comparing clinical automated, medical record, and hybrid data sources for diabetes quality measures. Joint Commission Journal Quality Improvement 10:555–565, 2002Google Scholar
61. Thomson W, Wang H, Xie M, et al: Assessing quality of diabetes care by measuring longitudinal changes in hemoglobin A1c in the Veterans Health Administration. Health Services Research 40:1818–1835, 2005Google Scholar



