Americans' Attitudes Toward Mental Health Treatment Seeking: 1990–2003
This study examined recent trends in attitudes toward treatment seeking from professionals for mental health problems and beliefs about the effectiveness of such treatment in the U.S. general population. A study that compared responses of American adults in 1957 and 1996 revealed no significant change in willingness to seek professional help for mental health problems ( 1 ). However, data from other settings have shown a positive change in attitudes toward mental health treatments in more recent years ( 2 , 3 ). Furthermore, the rapid increase in availability of online mental health information ( 4 ), public education and screening campaigns ( 5 , 6 ), and direct-to-consumer advertising of psychotropic medications in the United States ( 7 , 8 , 9 ) might have had an impact on the public's beliefs and attitudes about mental health treatments in more recent years.
Because attitudes toward mental health treatment seeking are important predictors of actual service use ( 10 ), examining time trends in attitudes has implications for understanding trends in the use of mental health services ( 11 , 12 ). Monitoring trends in public attitudes and beliefs also has implications for design of services and public health campaigns because concerns about lack of effectiveness of mental health services and stigma associated with mental illness and its treatment remain major obstacles to treatment seeking in the general population ( 13 ).
This study used data from two cross-sectional U.S. general population surveys of mental health from the early 1990s and early 2000s to compare public attitudes and beliefs across a time span of more than a decade. More specifically, the study examined trends in willingness to seek professional help, comfort level, and the perceived stigma and perceived effectiveness of mental health treatments. Analyses also examined whether variations across time were limited to, or more pronounced in, specific population subgroups.
Methods
Samples
Data were drawn from the National Comorbidity Survey (NCS) and the National Comorbidity Survey-Replication (NCS-R) ( 14 ). Briefly, NCS and NCS-R were nationally representative cross-sectional surveys of households in the 48 coterminous U.S. states. NCS was administered between September 1990 and February 1992 to 8,089 individuals between the ages of 15 and 54 and had a response rate of 82.4%. NCS-R was administered between February 2001 and April 2003 to 9,282 individuals aged 18 and older and had a response rate of 70.9%.
The NCS and NCS-R interviews each included two parts. Part 1 comprised a core diagnostic assessment module administered to all participants. Part 2 included further diagnostic assessments as well as questions about treatment-seeking attitudes and beliefs and was administered to all part 1 participants who met lifetime criteria for any core disorder and to probability subsamples of other participants. Part 2 samples comprised 5,877 participants in NCS and 5,692 in NCS-R. To make the age composition of samples comparable for the main analyses reported here, samples were further limited to 5,388 participants in NCS and 4,319 in NCS-R who were between the ages of 18 and 54.
To examine the generation effect on attitudes, further analyses were conducted in which age groups in NCS were combined with age groups in NCS-R that were, on average, 11 years older. The sample for examining the generation effect included all part 2 NCS participants (aged 15 to 54) and 4,116 part 2 NCS-R participants who were in the age range of 26 to 65 years.
Interviews were conducted in person. Informed consent was obtained before interviews. The human subjects committees of Harvard Medical School and the University of Michigan approved these recruitment and consent procedures. Secondary analyses of the data presented in this report were exempted from full review by the Institutional Review Board of the Beth Israel Medical Center, New York.
Assessments
Attitudes toward mental health treatment seeking were assessed by three questions. The first assessed willingness: "If you had a serious emotional problem, would you definitely go for professional help, probably go, probably not go, or definitely not go for professional help?" The second assessed comfort level: "How comfortable would you feel talking about personal problems with a professional—very comfortable, somewhat, not very, or not at all comfortable?" The third assessed perceived stigma: "How embarrassed would you be if your friends knew you were getting professional help for an emotional problem—very embarrassed, somewhat, not very, or not at all embarrassed?" For this study, the responses were coded from 0 to 3 so that a higher score indicates more willingness, more comfort, and less perceived stigma.
Beliefs about the effectiveness of mental health treatment and the likelihood of recovery without it were assessed by asking two questions: "Of the people who see a professional for serious emotional problems, what percent do you think are helped?" and "Of those who do not get professional help, what percent do you think get better even without it?" For this study, responses to each question were categorized into four mutually exclusive categories: 0%–24%, 25%–49%, 50%–74%, and 75%–100%.
Lifetime mental health treatment seeking was assessed by asking participants to identify from a list the types of professionals that they had ever seen for problems with their "emotions or nerves" or their "use of alcohol or drugs." The list included psychiatrists, psychologists, social workers, counselors, general practitioners or family physicians, other physicians, nurses, occupational therapists, other health professionals, ministers or priests, spiritualists, herbalists, and other professionals. Contact with any of these professionals was recorded as a positive history of lifetime mental health treatment seeking.
Psychological distress was assessed by 14 questions, mostly drawn from the Hopkins Symptom Checklist ( 15 ). The questions covered specific depressive and anxiety symptoms, such as depressed mood, loss of interest, hopelessness, trouble concentrating, inappropriate guilt or feelings of worthlessness, lack of energy, worrying too much, and feeling tense, and nonspecific symptoms of distress, such as feeling "trapped" or lonely. The participants were asked to rate the frequency of each symptom over the past 30 days on a scale ranging from never to often. For the purpose of this study, these ratings were given values ranging from 0 to 3, respectively. The possible scores on this scale, therefore, ranged from 0 to 42. The internal consistency of this symptom scale was quite high (Cronbach's α =.92), and the items were moderately correlated (average interitem correlation=.45). Principal components analysis of the items produced only one component with an eigenvalue greater than or equal to 1, indicating that one latent factor underlies all items ( 15 ). In the NCS-R sample, scores on this questionnaire correlated strongly (r=.73) with scores on K6 ( 16 )—another measure of distress commonly used in general population surveys.
To identify participants with significant distress on the symptom scale, a cutoff point was chosen that would identify the 5% of individuals in the general population who were most distressed (≥27 compared with <27). In the NCS-R sample, this cutoff score was strongly associated with the presence of common 12-month DSM-IV ( 17 ) disorders (major depression, dysthymia, generalized anxiety disorder, posttraumatic stress disorder, panic disorder with or without agoraphobia, and social anxiety) as ascertained by the Composite International Diagnostic Interview ( 18 ) (odds ratio [OR]=15.47, 95% confidence interval [CI]=9.42–25.42; t=11.13, df=42, p<.001). Of participants with a symptom score of 27 or higher, 77.4% met criteria for one or more of these DSM-IV conditions, compared with 18.1% of those with a symptom score of less than 27.
NCS and NCS-R used different versions of the Composite International Diagnostic Interview, based on different diagnostic criteria— DSM-III-R ( 19 ) in NCS and DSM-IV ( 17 ) in NCS-R. For this reason, diagnoses were not included in this study ( 20 ).
Impairment in functioning was assessed by three similarly structured sets of questions about the number of days in the past 30 days in which the participant was "totally unable to work or carry out normal activities" or had to "cut down" on what he or she did or "did not get as much done as usual" or in which it took the participant "an extreme effort" to perform up to his or her "usual level" ( 15 ). After each question about the number of days, the participant was asked to estimate the number of days of impairment that was attributable to "emotions, nerves, mental health, or use of alcohol or drugs." For this study, impairment was operationalized as having one or more impaired days in the past 30 days according to any of the above definitions.
Sociodemographic variables included sex, age (18–24, 25–34, 35–44, and 45–54 years), race-ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, other), years of education (0–11, 12, 13–15, 16 or more), family income as a percentage of the federal poverty level for 1990 in the NCS and for 2001 in the NCS-R (low income, less than 150%; low to average, 150% to 299%; high to average, 300% to 599%; and high, 600% or greater) ( 20 ). For the analysis of generation effect, four mutually exclusive generations were constructed which combined each NCS age group with an NCS-R age group that was on average 11 years older (for example, the NCS participants who were from 15 to 24 years old were combined with NCS-R participants who were 26 to 35 years old).
Data analysis
Data were analyzed in four stages. First, attitudes and beliefs about mental health treatment seeking were compared across NCS and NCS-R by using bivariate proportional-odds ordinal logistic regression models. The independent variable in these analyses was the dummy-coded variable of time (1990–1992 [NCS]=0, and 2001–2003 [NCS-R]=1). To adjust for multiple testing, a cutoff p value of .01 was used for determining statistical significance in these analyses. Because only attitudes showed significant variation across time, further analyses were limited to attitudes.
Second, sociodemographic and clinical correlates of attitudes were examined by using a series of bivariate proportional-odds ordinal logistic regression analyses. For variables with multiple categories, such as race-ethnicity, overall adjusted Wald tests were computed. To limit the number of regression models fitted and thus minimize type I error, the three attitude variables were combined into one multivariate proportional-odds ordinal logistic regression model by using the methodology proposed by Horton and Fitzmaurice ( 21 ) for analysis of multiple variables from the same individuals in complex survey designs. This method is conceptually similar to multivariate analysis of variance and allows for efficient modeling of multiple ratings for the same individuals in one regression model while adjusting for lack of independence among ratings. By entering an independent dummy variable as an identifier for different ratings, variations among these different ratings can be modeled. Thus, to model variations among the three attitude ratings, two dummy variables were entered into the model as independent variables.
When exponentiated, ordinal logistic regression coefficients can be interpreted as odds ratios (ORs), representing the ratio of odds of having a higher (more positive) attitude rating compared with the odds in the reference group. For example, an OR of 1.41 associated with female gender compared with male gender indicates that females have 41% greater odds of having a more positive attitude rating than males.
Third, to further evaluate the magnitude of variations in attitudes across different sociodemographic and clinical subgroups, a set of bivariate proportional-odds ordinal logistic regression analyses were conducted that stratified the sample on the basis of population subgroups. The attitude rating was the dependent variable in these analyses, and the time variable (1990–1992 [NCS]=0, and 2001–2003 [NCS-R]=1) was the independent variable of interest. These analyses were repeated within each stratum.
Fourth, a multivariate proportional-odds ordinal logistic regression analysis was conducted to examine the characteristics associated with attitudes as well the interaction terms of different characteristics with the variable of time. As recommended by Hosmer and Lemeshow ( 22 ), variables that were associated with attitude ratings at a p level of less than .25 in the bivariate analyses in the second stage above were entered in the multivariate model. In addition to main effects, two-way interaction terms of each variable with the time variable (1990–1992 [NCS]=0, and 2001–2003 [NCS-R]=1) were also tested, and those associated with attitude ratings at a p level of less than .25 were entered into the multivariate regression model. These interaction terms tested whether changes in attitudes across time varied in different subgroups of the population ( 23 ). For example, a significant age-by-time interaction would indicate that attitudes of individuals from different age groups varied differently across time. Main effects and interaction terms were maintained in the final multivariate model if they were associated with attitude ratings at the predefined significance level of less than .01 (based on adjusted Wald tests for multicategory variables).
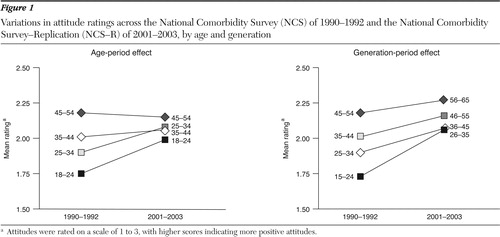
Age variations in attitudes can be attributed to either period effect or generation effect. However, because of collinearity, these effects cannot be simultaneously modeled. By comparing participants in the same age groups across time, the main analyses focused on age-period effect. To examine the generation-period effect, further analyses were conducted in which NCS participants were compared with NCS-R participants who were 11 years older, on average. These analyses were limited to all NCS part 2 participants and NCS-R part 2 participants between the ages of 26 and 65 years, as noted above.
NCS and NCS-R used complex stratified sampling designs. Survey weights, stratification, and clustering (primary sampling units) were included in the analyses to adjust for their effects and make samples representative of the U.S. population. Clustering at the level of primary sampling units also adjusted for lack of independence in multiple attitude ratings from the same individuals. Stata 9.2 software was used for all analyses ( 24 ). All percentages presented here are weighted.
Results
In bivariate ordinal logistic regression analyses, the 2001–2003 participants were more likely than the 1990–1992 participants to report a willingness to seek mental health treatment for serious emotional problems (OR=1.24, CI=1.11–1.39; t=3.84, df=84, p< .001), to feel comfortable seeking such help (OR=1.27, CI=1.07–1.50; t=2.82, df=84, p=.006), and to be less embarrassed if friends found about it (OR=1.33, CI=1.17–1.51; t=4.43, df=84, p<.001). The raw data on attitudes are presented in Table 1 . As these data indicate, the change was particularly pronounced for the most positive attitudes: 41.4% in 2001–2003 reported that they would "definitely go" for professional help for a serious emotional problem compared with 35.6% in 1990–1992. Similarly, 32.4% in 2001–2003 reported feeling "very comfortable" talking about personal problems with a professional compared with 27.1% in 1990–1992, and 40.3% in 2001–2003 reported being "not at all embarrassed" if friends knew about their getting professional help compared with 33.7% in 1990–1992.
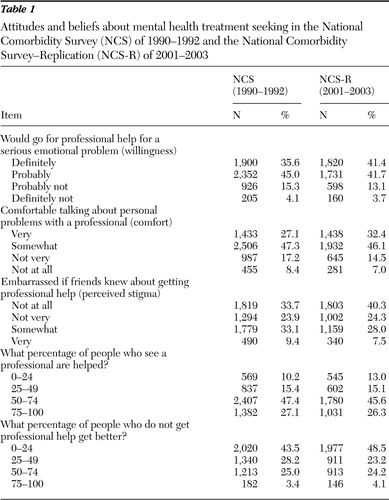 |
Participants' beliefs about the effectiveness of psychiatric treatment showed smaller, statistically nonsignificant differences across surveys (belief about the percentage who are helped by seeing a professional, OR=.91, CI=.80–1.02; p=.109; belief about the percentage who get better without getting professional help, OR=.88, CI=.78–1.01; p=.062). Participants in both surveys estimated that more than half of the people who see a professional are helped, whereas less than half of those who do not obtain professional help get better ( Table 1 ).
The variation across time was corroborated in bivariate analyses of the combined attitude ratings ( Tables 2 and 3 ). In addition, analyses presented in Table 2 show that participants' sex, racial-ethnic group, age, generation, education, income, and lifetime history of mental health treatment seeking were associated at a statistically significant level with attitude ratings. Females had 41% higher odds of reporting a more positive attitude toward mental health treatment seeking than males. Table 2 also shows that non-Hispanic black respondents had a more positive attitude toward mental health treatment seeking than non-Hispanic whites, as did adults in the 25- to 54-year age range compared with younger adults, participants in the older generations compared with the youngest generation (15–24 years in 1990–1992), participants with high family income (600% of the federal poverty level or higher) compared with those with low family income (less than 150% of the poverty level), and participants with a history of mental health treatment seeking compared with those with no such history.
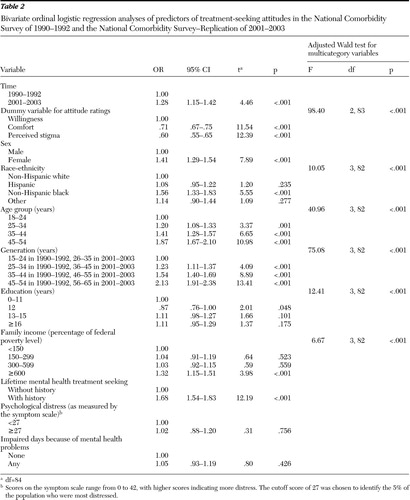 |
 |
The effect of education was not linear. Participants with 12 years of education had a less positive attitude than those with less than 12 years of education, whereas participants with more than 12 years of education did not have a less positive attitude than those with less than 12 years of education ( Table 2 ). Psychological distress (as indicated by symptom score of 27 or higher) and impairment in functioning were not associated with attitudes at a statistically significant level.
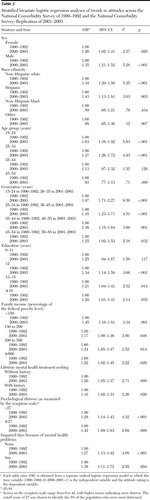
As the stratified analyses in Table 3 suggest, improvement in attitudes occurred in most sociodemographic and clinical subgroups. Not all ORs were different from 1 at a statistically significant level. However, most were larger than 1, many at a statistically significant level. The magnitude of change in attitudes was modest because most ORs were smaller than 1.5, which is generally considered a small effect size, and none reached 2.5, which is considered a medium effect size.
On the basis of the bivariate analyses reported in Table 2 , variables of time, sex, race-ethnicity, age, education, income, and lifetime history of mental health treatment seeking met the inclusion criterion of p<.25 and were entered into the multivariate model ( Table 4 ). In addition, the dummy-coded variable for individual attitude ratings was included to adjust for variations among the three ratings. Finally, the interaction terms of sex by time, age by time, and race-ethnicity by time, which met the criterion of p<.25, were entered into the multivariate model.
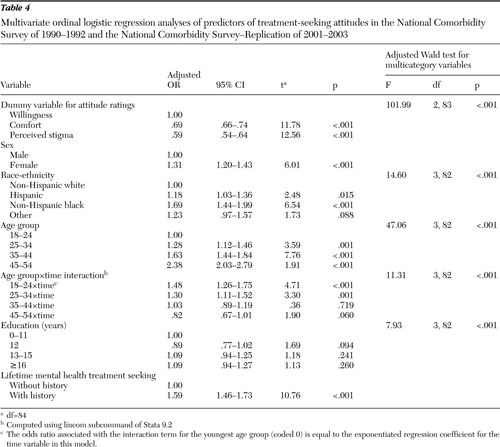 |
Income and the interaction terms of sex by time and race-ethnicity by time were not associated with attitudes at a statistically significant level (p<.01) in the multivariate model and were excluded from the final model. The main effects of sex, race-ethnicity, education, and lifetime mental health treatment seeking, as well as the interaction of age by time were statistically significant, and the significance was maintained in the final model ( Table 4 ). The main effect of age group in this model compares the odds of having a higher (more positive) attitude rating across age groups in 1990–1992 (time=0), whereas the interaction term of age by time compares the odds of having a higher attitude rating across the two times within each age group. The main effect of time in this model compares the odds of having a higher attitude rating across the two time points in the youngest age group (18 to 24 years).
The generation and the age group variables could not be entered into the same model because of collinearity. Thus a separate multivariate regression analysis with generation and the generation-by-time interaction term instead of age and the age-by-time interaction term was conducted. The sociodemographic and clinical variables used in the multivariate model described above were also included in this model. The main effect of generation (adjusted Wald test F=56.00, df=3 and 82, p<.001) and the interaction term of generation by time (adjusted Wald test=4.37, df=3 and 82, p=.007) were statistically significant in this model.
The interactions of age by time and generation by time represent the age-period effect and generation-period effect, respectively, and are also presented in Figure 1 . The age-period effect curves suggest that the attitude of younger adults (less than 35 years of age) toward mental health treatment seeking in 2001–2003 was more positive than the attitude of adults of the same age in 1990–1992, whereas the attitude of adults 35 years old or older was similar across the two time points. The generation-period effect curves in Figure 1 reflect a general improving trend in attitudes across time in all generations. The improvement, however, was much more pronounced in the younger generation (15 to 24 years old in 1990–1992).
Discussion
Americans' attitudes toward mental health treatment seeking improved modestly over the past decade. The improvement has occurred in comfort level and willingness to seek care as well as in perceived stigma. This finding is consistent with reports from other settings ( 2 , 3 ). Because stigma and poor attitudes toward mental illness and its treatment have traditionally been considered major barriers to treatment seeking ( 13 , 25 ), these recent improvement in attitudes should be considered a welcome development.
The finding of a positive association between service use and attitudes toward treatment seeking in this study suggests that attitudes may play a role in treatment-seeking behavior. However, a causal relationship cannot be examined in cross-sectional data such as the data from the NCS and NCS-R, in which the reciprocal effects of treatment seeking on attitudes and of attitudes on treatment seeking cannot be separated. The relationship between attitudes and treatment-seeking behavior needs to be examined in future longitudinal studies in which the temporal order between attitudes and behaviors can be established.
It is, nevertheless, noteworthy that some of the correlates of attitudes toward mental health treatment seeking in this study are also positively correlated with treatment-seeking behavior, such as female sex and middle age ( 20 ). On the other hand the finding of more positive attitudes among non-Hispanic blacks is puzzling because persons from minority groups generally use fewer services ( 20 ). This finding, however, is consistent with previous analyses of the NCS data, which also found a more positive attitude toward mental health treatment seeking among black respondents ( 26 ).
It should also be noted that the changes in attitudes were modest, whereas the use of mental health services during the period examined grew markedly ( 11 , 20 ). On the basis of the NCS and NCS-R data, Kessler and colleagues ( 20 ) reported that 20.1% of the population in the 2001–2003 period received mental health treatments, compared with 12.2% in 1990–1992, which represents an increase of about 65%. Thus changes in service use can be only partly attributed to changes in individual attitudes. A full understanding of the reasons for recent changes in service use requires exploration of other individual determinants of treatment seeking, such as perceived need and access to services, and of contextual factors, such as attitudes and beliefs of family members, friends, and coworkers ( 27 , 28 ). The attitudes and beliefs of a person's social network not only influence treatment-seeking behavior but also recognition and labeling of problems as mental health problems in need of treatment. Analyses that examine the influence of attitudes and beliefs on treatment-seeking behavior at the individual level may not fully capture these broader contextual influences.
An interesting finding of the study was the age and generation variations in trends in attitudes across time. Adults between the ages of 18 and 34 in 2001–2003 had a more positive attitude toward mental health treatment seeking than adults of the same age in 1990–1992, whereas adults in the 35- to 54-year age group had similar attitudes at the two time points. Results of the generation analysis also support this finding. Although attitudes toward mental health treatment seeking improved in all generations, which possibly represents the effect of maturation, the improvement was greatest in the generation that was 15 to 24 years old in 1990–1992. This generational effect is intriguing and may reflect the impact of formal education or mass media to which the younger generation is generally more exposed. This generation effect is a welcome development because young adults tended to have a poorer attitude toward mental health treatment seeking in 1990–1992 and have traditionally used fewer services than middle-aged adults ( 10 ).
Perhaps as important as the significant variations across age and generation subgroups is the consistent improvement in attitudes across genders and social classes and levels of distress, as indicated by the odds ratios associated with the time variable in each of these subgroups ( Table 3 ). Whatever factors have brought about the changes in attitudes across time, their effects appear to be global and to transcend the gender and social class boundaries that have traditionally shaped disparities in use of mental health services in the United States.
In contrast to changes in attitudes, beliefs about the effectiveness of mental health treatment and about recovery without such treatment did not change appreciably across time. Thus increased use of mental health services and improved attitudes toward mental health treatment seeking in more recent years cannot be attributed to changes in beliefs about the effectiveness of mental health treatments or about the likelihood of recovery without treatment. This finding indirectly points to reduction in psychological barriers, such as the stigma associated with the receipt of mental health care, as a major cause of improved attitudes to mental health treatment seeking and also, possibly, a contributing factor to increased use of mental health services in recent years.
The findings from this study should be viewed in the context of its limitations. First, assessments of attitudes and beliefs did not distinguish between pharmacological and psychosocial treatments. Attitudes and beliefs about these different forms of treatment might have changed differently in recent years ( 29 , 30 ). Second, the general public is able to distinguish between different forms of mental illness and the appropriateness of various treatments for each condition ( 30 )—a distinction not captured by the NCS and NCS-R questions. Third, stigma associated with mental illness and its treatment is complex ( 31 ), encompassing both cognitive evaluations and emotional reactions. Furthermore, stigma associated with treatment seeking for severe mental illnesses might have different correlates and time trends than stigma associated with treatment seeking for the less severe mental health problems. Of note, there is some evidence that the public perception of violence among persons with mental illness in the United States significantly increased between 1950 and 1996 ( 1 , 32 ). Whereas, in the same study, Americans were more likely in 1996 than they were in 1950 to admit having experienced a "nervous breakdown" in their lifetime ( 1 ). A full evaluation of the multiple aspects of stigma associated with mental illness and its treatment requires more detailed information than is captured by the NCS and NCS-R questions. Finally, accurate ascertainment of a generation or cohort effect requires that the same individuals be followed over time. However, this study is based on data from two cross-sectional surveys. Findings with regard to generation effect would be valid only with the assumption that the age groups in each survey were representative of their generations.
Conclusions
In the context of the study's limitations, comparison of the data from 1990–1992 and 2001–2003 suggests a modest improvement in Americans' attitudes toward mental health treatment seeking over a period of more than a decade. The improvement was more pronounced among the younger generation. Coupled with the growing perception of psychological distress in the general public ( 1 ), these trends in attitudes toward mental health treatment seeking will likely contribute to an increased demand for mental health services in the coming years.
Acknowledgments and disclosures
The National Comorbidity Survey was supported by grants R01-MH-46376, R01-MH-49098, and R01-MH-52861 from the National Institute of Mental Health (NIMH), with supplemental support from grant MH-46376 from the National Institute of Drug Abuse (NIDA) and grant 90135190 from the William T. Grant Foundation. The National Comorbidity Survey Replication is supported by grant U01-MH 60220 from NIMH, with supplemental support from grants from the NIDA, the Substance Abuse and Mental Health Services Administration, the Robert Wood Johnson Foundation (grant 044708), and the John W. Alden Trust.
The author reports no competing interests.
1. Pescosolido BA, Martin JK, Link BG, et al: Americans' Views of Mental Health and Illness At Century's End: Continuity and Change. Bloomington, Indiana University, Indiana Consortium of Mental Health Services Research, 2000Google Scholar
2. Jorm AF, Angermeyer MC, Katschnig H: Public knowledge of and attitudes to mental disorders: a limiting factor in the optimal use of treatment services, in Unmet Need in Psychiatry. Edited by Andrews G, Henderson S. Cambridge, United Kingdom, Cambridge University Press, 2000Google Scholar
3. Angermeyer MC, Matschinger H: Have there been any changes in the public's attitudes towards psychiatric treatment? Results from representative population surveys in Germany in the years 1990 and 2001. Acta Psychiatrica Scandinavica 111:68–73, 2005Google Scholar
4. Dearness KL, Tomlin A: Development of the national electronic library for mental health: providing evidence-based information for all. Health Information Library Journal 18:167–174, 2001Google Scholar
5. Greenfield SF, Reizes JM, Muenz LR, et al: Treatment for depression following the 1996 National Depression Screening Day. American Journal of Psychiatry 157:1867–1869, 2000Google Scholar
6. Regier DA, Hirschfeld RM, Goodwin FK, et al: The NIMH Depression Awareness, Recognition, and Treatment Program: structure, aims, and scientific basis. American Journal of Psychiatry 145:1351–1357, 1988Google Scholar
7. Curry TJ, Jarosch J, Pacholok S: Are direct to consumer advertisements of prescription drugs educational? Comparing 1992 to 2002. Journal of Drug Education 35:217–232, 2005Google Scholar
8. Goldman R, Montagne M: Marketing "mind mechanics": decoding antidepressant drug advertisements. Social Science and Medicine 22:1047–1058, 1986Google Scholar
9. Nikelly AG: Drug advertisements and the medicalization of unipolar depression in women. Health Care for Women International 16:229–242, 1995Google Scholar
10. Mojtabai R, Olfson M, Mechanic D: Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry 59:77–84, 2002Google Scholar
11. Mojtabai R: Trends in contacts with mental health professionals and cost barriers to mental health care among adults with significant psychological distress in the United States: 1997–2002. American Journal of Public Health 95:2009–2014, 2005Google Scholar
12. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:203–209, 2002Google Scholar
13. Wrigley S, Jackson H, Judd F, et al: Role of stigma and attitudes toward help-seeking from a general practitioner for mental health problems in a rural town. Australian and New Zealand Journal of Psychiatry 39:514–521, 2005Google Scholar
14. Kessler RC, Chiu WT, Demler O, et al: Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:617–627, 2005Google Scholar
15. Mojtabai R: Residual symptoms and impairment in major depression in the community. American Journal of Psychiatry 158:1645–1651, 2001Google Scholar
16. Kessler RC, Andrews G, Colpe LJ, et al: Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine 32:959–976, 2002Google Scholar
17. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
18. Wittchen HU: Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. Journal of Psychiatric Research 28:57–84, 1994Google Scholar
19. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, rev. Washington, DC, American Psychiatric Association, 1987Google Scholar
20. Kessler RC, Demler O, Frank RG, et al: Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine 352:2515–2523, 2005Google Scholar
21. Horton NJ, Fitzmaurice GM: Regression analysis of multiple source and multiple informant data from complex survey samples. Statistics in Medicine 23:2911–2933, 2004Google Scholar
22. Hosmer DW, Lemeshow S: Applied Logistic Regression. New York, Wiley, 2000Google Scholar
23. Newsom JT, Prigerson HG, Schulz R, et al: Investigating moderator hypotheses in aging research: statistical, methodological, and conceptual difficulties with comparing separate regressions. International Journal of Aging and Human Development 57:119–150, 2003Google Scholar
24. Stata Statistical Software, Release 9.2. College Station, Tex, Stata Corp, 2007Google Scholar
25. Van Voorhees BW, Fogel J, Houston TK, et al: Beliefs and attitudes associated with the intention to not accept the diagnosis of depression among young adults. Annals of Family Medicine 3:38–46, 2005Google Scholar
26. Diala CC, Muntaner C, Walrath C, et al: Racial/ethnic differences in attitudes toward seeking professional mental health services. American Journal of Public Health 91:805–807, 2001Google Scholar
27. Kadushin C: Why People Go to Psychiatrists. New York, Atherton, 1969Google Scholar
28. Pescosolido B, Boyer CA: How do people come to use mental health services? Current knowledge and changing perspectives, in A Handbook for the Study of Mental Health. Edited by Horwitz AV, Scheid TL. Cambridge, United Kingdom, Cambridge University Press, 1999Google Scholar
29. Croghan TW, Tomlin M, Pescosolido BA, et al: American attitudes toward and willingness to use psychiatric medications. Journal of Nervous and Mental Disease 191:166–174, 2003Google Scholar
30. Jorm AF, Christensen H, Griffiths KM: The public's ability to recognize mental disorders and their beliefs about treatment: changes in Australia over 8 years. Australian and New Zealand Journal of Psychiatry 40:36–41, 2006Google Scholar
31. Link BG, Yang LH, Phelan JC, et al: Measuring mental illness stigma. Schizophrenia Bulletin 30:511–541, 2004Google Scholar
32. Phelan JC, Link BG: The growing belief that people with mental illnesses are violent: the role of the dangerousness criterion for civil commitment. Social Psychiatry and Psychiatric Epidemiology 33(suppl 1):S7–12, 1998Google Scholar



