Tenant Outcomes in Supported Housing and Community Residences in New York City
This study examined whether outcomes in housing, clinical status, and well-being of persons with severe mental illness and a history of homelessness differ between those in supported housing and those in community residences. Supported housing, in its ideal form, fosters independence by providing tenure rights and flexible levels of support that are not a condition of tenancy. To promote community integration, tenants with mental disorders in supported housing are not distinguished from others and are presented with choices about housing and services. Supported housing advocates contend that these operating principles ( 1 , 2 , 3 , 4 , 5 ) are associated with both housing stability and appropriate use of mental health services, effects that in turn are expected to result in improved clinical and daily living functioning. Housing preference surveys among homeless persons with psychiatric disabilities have found that they prefer independent housing with features of supported housing rather than group residential treatment facilities ( 6 , 7 , 8 , 9 ).
Others argue that supported housing disregards clinical reality ( 10 ), that only a "small, high-functioning group" ( 11 ) can succeed in these settings ( 12 , 13 , 14 ), and that without mandatory services those with lower functioning can suffer feelings of isolation. A continuum of options based on the services and supports provided and levels of autonomy afforded to the tenant is seen as a preferable approach ( 11 , 15 , 16 ). Most often, the entry point into the housing continuum for persons who are homeless or who are released from hospitals is a community residence in which participation of residents in mental health services is typically mandatory and the daily life of a resident is highly structured. Tenants are expected to transition to more autonomous forms of housing when they are "ready" ( 17 , 18 ).
In a 2004 article Rog ( 19 ) reviewed ten studies of supportive and supported housing, including the McKinney Demonstration Program, the Center for Mental Health Services (CMHS) Homeless Prevention Program, and the CMHS Housing Initiative. She concluded, as did Lipton and colleagues ( 20 ), that "once in housing with supports, a majority of individuals with serious mental illness stay in housing" regardless of the housing model. However, comparisons of supported housing models and other models have yielded inconsistent results ( 19 ). Of note is the cost-effectiveness of supported housing compared with that of "evolving consumer households" ( 21 ) and homelessness ( 22 ).
To expand the knowledge base, the Substance Abuse and Mental Health Services Administration (SAMHSA) funded a multisite study to compare housing, clinical, and well-being outcomes of persons with severe mental illness in supported housing as described above and in other models in the continuum. This article reports findings from the New York City site-specific study, in which two distinct types of supported housing were compared with nine fairly similar community residences operated by three agencies. All the housing providers believed that they had been accepting similar populations, which provided a basis for comparisons. The predominately homeless, ethnically diverse sample in the New York City sites provided an additional opportunity to reexamine the role of factors that have been reported to contribute to housing instability—abusing substances, being a male, being nonwhite, and having a diagnosis of schizophrenia or schizoaffective disorder ( 23 , 24 ). Individuals involved in site management, tenant representatives, housing specialists, and consumer advocates were collaborative partners in all phases of the study.
Methods
Design
Conducting services research within a large complex system, such as the system in New York City, presents many design challenges. Neither the sites nor the participants were randomly chosen, and participants could not be randomly assigned to housing types. Selection of housing sites was based on recommendations from housing specialists in New York City. Study participants were consecutive tenants who entered the selected sites between October 14, 1998, and April 19, 2000, and who provided informed consent to participate. Tenants were referred to housing from hospitals, shelters, the streets, and clinics. Participants had a primary diagnosis of schizophrenia, schizoaffective disorder, or bipolar or depressive disorders. All were 18 years of age or older and had not been housed at the entry site during the past three months. Research approval was obtained from the institutional review board of the Nathan Kline Institute for Psychiatric Research.
Prestudy analysis of similar cohorts was conducted, which indicated that persons in the two housing models had sufficient commonalities to allow use of a stratified analysis approach to compensate for nonrandomization.
Baseline interviews took place as soon as possible after the tenant moved into the housing. For tenants in both housing models, the interview took place an average of 3.5 weeks after housing entry. Two follow-up interviews were conducted at approximately six and 12 months later. At 18 months, only a subset of tenants (those enrolled during the earlier months of the study) was interviewed because of limited project funds.
Sample
Housing sites. A fidelity instrument expressly developed for the SAMHSA multisite study was used to score the housing models on a number of dimensions that, taken together, encompass the ideal characteristics of supported housing. In New York City, supported housing scored higher on this instrument than the community residences in terms of the level of integration of the housing population with community populations, the separation of service and housing functions, and the provision of rights of tenure. Community residences generally scored higher on the quality of the housing. Little difference was found in individualization of services and the privacy afforded by the housing.
In all participating sites, tenants were helped to obtain any public assistance to which they were entitled. The two participating supported housing models offer services and supports through an agency that is independent of the housing, but the models have differing philosophies of housing and community integration ( 25 ). In the first variant, tenants, mostly living alone, reside in studio or one-bedroom apartments located throughout the city. Sobriety and treatment are not preconditions for housing ( 26 ). An assertive community treatment team that sees tenants at least once a week and provides medication and money management also provides support and treatment services. The team is available around the clock. Recreational programs, such as art, photography, and writing classes, are offered at a central location.
In the second variant, tenants live in a renovated residential hotel in studio apartments, each with a bathroom and kitchenette. Thirty percent of units in the hotel are for persons with mental illness. All tenants are prescreened for evidence of six months of clean and sober behavior, and they can be asked to leave if they do not maintain good-neighbor status—for example, without too many complaints from neighbors. On-site crisis services are continuously available to tenants in coordination with a New York City psychiatric emergency service. On-site case managers are available to all tenants, as are additional services and amenities, such as a job training program, gym, and computer room. Use of these resources is voluntary.
In each supported housing program, tenants pay 30 percent of their income toward rent, and their respective agency guarantees the remainder of the rent. Tenants are responsible for meals and utility expenses. A money management program ensures payment for rent and utilities. Other monies are discretionary tenant income. The total direct cost for shelter and services in both models is approximately $1,200 per tenant per month ( 27 ).
The three agencies that operate the nine community residences provide intensive supportive services in the residences, which are only for persons with mental illness. These residences are in buildings with single or shared rooms or with studio apartments. All buildings have common dining, meeting, and services space. All new tenants are required to use a meal plan. It is strongly recommended that consumers attend a continuing day treatment or rehabilitation program. Each tenant is assigned a housing case manager and may have other case managers. Three community residence sites are designed to serve clients with both mental illness and substance use disorders. At all community residence sites, sobriety is closely monitored, and loss of sobriety results in mandatory treatment or expulsion from housing. Housing staff are available around the clock. Recreational activities are provided at each site.
Tenants in community residence programs turn their monthly income over to the housing agency, from which they receive an agency-specified personal needs allowance. Expenses for meals and utilities are deducted from the monthly allowance. The total direct cost for shelter and services averages approximately $2,400 per tenant per month ( 27 ).
Tenants. Consent rates for study-eligible tenants in both models were over 95 percent. Initially 157 persons enrolled, 75 (48 percent) in supported housing and 82 (52 percent) in community residences. Eight participants in supported housing and ten in community residences completed only a baseline interview and were dropped from the study, which resulted in a sample of 139. The 18 persons not included in the study were not significantly different from the remaining group on any baseline characteristics. Overall, 80 percent of persons were available for the 12-month interview. The 18-month interviews were conducted with only 91 enrollees (those with the earliest enrollment dates). Nineteen persons had at least two interviews but subsequently refused to participate, were lost to follow-up, or died (one death in each housing condition). Field staff boosted follow-up rates by searching shelter and jail records, canvassing participants' old haunts, and contacting friends and relatives identified by participants and workers from participants' initial placements.
Measurement
Descriptors. Baseline data were from self-reports of demographic characteristics, homelessness, treatment history, physical and mental status, and referral source. Substance use and psychiatric diagnoses were obtained from two sources: a centralized housing placement data set maintained for all sites by the New York City Center for Urban and Community Services, which is part of New York/New York housing, and directly from the agency providing supports to participants in scatter-site New York City apartments.
Outcomes. Days in initial placement were obtained from a self-report residential history instrument ( 28 ). The instrument asks tenants about the places where they have slept, starting with the night before the interview and for the previous six months. Places include other housing, housing of family and friends, treatment facilities, shelters, and the street or jail. Tenants were considered to be in their housing unit if it was held for them while they were in the hospital or in jail, which would be the case for any person whose rent is paid through a period of time spent in a hospital or jail.
Housing satisfaction was measured with a scale developed for the SAMHSA multisite study ( 29 ). Analyses of overall housing satisfaction were conducted, and subscales assessed a tenant's perceptions of the housing condition (environment), levels of independence and physical autonomy afforded by the housing (autonomy), and facilitation of social interactions (social). Two additional single items assessed economic satisfaction (available money to spend after housing costs are met) and program satisfaction (the ease of contacting a program case manager).
Clinical outcomes included emergency department and crisis service use and the total and subscale scores on the depression-anxiety, impulsivity, and psychosis subscales of the Basis-32, a clinical and functioning assessment scale ( 30 ). Personal well-being outcomes were an aggregate score of a subset of items on "community integration" adapted from the Social Integration Scales ( 31 ), which inventories "community-type" activities; "isolation" items from the UCLA Loneliness Scale, Version 3 ( 32 ); the Overall Choice and Empowerment Scale ( 33 ); and the item on global quality of life from the Lehman Quality of Life Scale ( 34 ).
Statistical analyses
Propensity scoring. Propensity scoring, widely applied in health-related research since 1983 ( 35 ), was used because randomization was not possible. Randomization allows causal inference to be made about the effect of the housing condition on outcome. With propensity scoring, randomization is mimicked and causal inferences can be made. The propensity score for each study participant is the probability of being assigned to supported housing. It is used to form groups (strata) of persons with similar probabilities of being assigned to supported housing. The score was obtained by using logistic regression. The dependent variable in the model is "being assigned to supported housing" (yes or no), and the covariates included a person's background characteristics. Covariates were education, age, having children younger than 18 years, gender, ethnicity, homeless days in the previous 12 months, perceived health status, age at first contact with the mental health system, lifetime hospitalizations, diagnosis, Basis-32 depression subscale score, Supplemental Security Income and Social Security Disability Insurance status, number of times arrested or picked up for any crime in the past six months, referral source into housing, lifetime alcohol use, and drug use in the previous six months.
The propensity scores were used to form three groups (strata) of persons defined by low, medium, and high scores. Within strata, randomization is mimicked as all persons have a similar probability of being assigned to supported housing, and thus causal inferences can be made. Tenants in stratum 1 represent what the current system would view as the least likely candidates for supported housing (because they have the smallest probability of being assigned there), whereas those in stratum 3, would be considered the most likely.
In our use of propensity scores, outcome comparisons are made within strata and not directly for the total sample. However, the effect can be tested for significance for the sample as a whole if the directionality of the effect size is the same in each stratum. In this case, effects are essentially averaged across strata and tested for significance. In theory, persons within a stratum in the two housing conditions are not expected to differ in the multivariate distribution of their covariates ( 36 ), but as in randomization, univariate differences in characteristics may be seen and controlled for by the use of covariates in regression models.
Statistical models
Several modeling techniques were used in our analysis. For all analyses, finding are reported at the p<.05 level.
Survival models. Kaplan-Meier survival models were used to estimate the amount of time in initial placement for each housing type within a propensity stratum. These distributions were compared by using a logrank test. Cox models were used to examine the impact on time in initial placement by means of a stepwise entry mode of housing model, propensity stratum, propensity-by-housing model interactions, and baseline covariates.
Regression models. Hierarchical linear models were used to examine the effects of time and housing model on tenant outcomes. These models included the propensity stratum, interaction terms to allow propensity-specific stratum analysis of housing effects, and baseline variables that were hypothesized to moderate all outcomes: the Basis-32 depression score, diagnosis, substance abuse status, and referral source. Additional baseline covariates were not included, as they would have saturated the models. In these models, under the assumption of data missing at random, participants who had missing data but who had completed at least two interviews were included because their linear trend could be deduced.
Point-in-time regression models were used to examine the effects of a larger number of covariates on outcomes than could be handled in the more complex models. In these analyses, propensity stratum was included as a covariate. Models were fit for each outcome variable at each interview time point. Across these models, sample sizes vary because of changes in response rates over time.
Intent-to-treat and "true-stayer" samples. For the hierarchical and regression models, analyses were performed on both intent-to-treat (N=139) and "true-stayer" (N=80) samples. The intent-to-treat analyses in effect examined the impact of the initial assignment on outcome, because tenants were identified with their initial placement even if they moved, dropped out of housing, or had long residential treatment stays or time in jail. The true-stayer analysis examined the impact of the housing itself and required a sample of participants who had had a "sufficient dose" of their initial placement. The true-stayer analysis approach that we used is based on Little and Rubin's ( 37 ) potential outcomes model.
To be a true stayer, a tenant had to be in the study for at least 365 days, of which at least 180 days (not necessarily sequential) were spent in the housing in which he or she was initially placed. Days in treatment settings and brief sojourns elsewhere were allowed if the housing slot was maintained, but persons who had multiple moves to jail or prison, to a shelter, or to the street—or who had a single stay in these settings of more than 20 days—were excluded. Second, the potential-outcomes model also requires that true stayers in one condition be true stayers in the alternate condition—a "potential outcome" that can only be predicted because it is not observed. We used a logistic regression model to predict if a true stayer in one condition would have been a true stayer in the alternate condition. Causal inference about the efficacy of the housing intervention can be made for the potential-outcome true-stayer sample ( 37 ).
Results
Baseline characteristics
Intent-to-treat sample. In the intent-to-treat sample (N=139), participants in supported housing differed significantly (p<.05) from those in community residences on a number of characteristics. The supported housing participants were older, more likely to be white and less likely to be black, and less likely to have children younger than 18. They also had, on average, fewer lifetime hospitalizations and were less likely to take medications for mental health, to have diagnoses of psychosis, and to have abused substances in the past. Because we conducted outcome analyses only within propensity strata, the population differences that were observed for the total sample were mitigated.
True-stayer sample. The true-stayer sample (N=80) was somewhat older than the other participants (N=59), more likely to be white, less likely to be black, and more likely to have major depression than schizophrenia. The differences between the supported housing tenants and the community residence tenants were similar to those found for the intent-to-treat sample, but no direct comparisons are made of these groups in total.
Propensity stratum samples
Between-stratum comparisons. Compared with tenants in strata 2 and 3, stratum 1 tenants were significantly younger, less educated, more likely to be black, and younger at first contact with the mental health system; they also had more lifetime hospitalizations. They were more likely to have schizophrenia or schizoaffective disorder than tenants in stratum 3, who were more likely to have bipolar disorder or major depression. Stratum 1 tenants were more likely to have been referred from hospitals and shelters or the street and to have children younger than 18 than tenants in the other two strata. As expected, in propensity strata 1 and 3, the number of participants in each housing type differed considerably, with a larger number in community residences in propensity stratum 1 and a larger number in supported housing in propensity stratum 3.
Within-stratum comparisons.Tables 1 and 2 present the baseline characteristics of tenants in each housing condition by propensity stratum for the intent-to-treat sample and for the true-stayer sample. For both samples, tenants' characteristics within a propensity stratum are better balanced between the housing conditions.
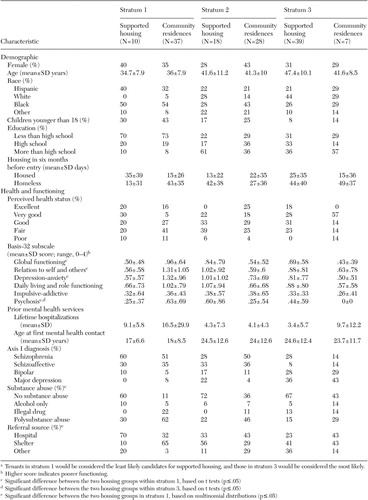 |
a Tenants in stratum 1 would be considered the least likely candidates for supported housing, and those in stratum 3 would be considered the most likely.
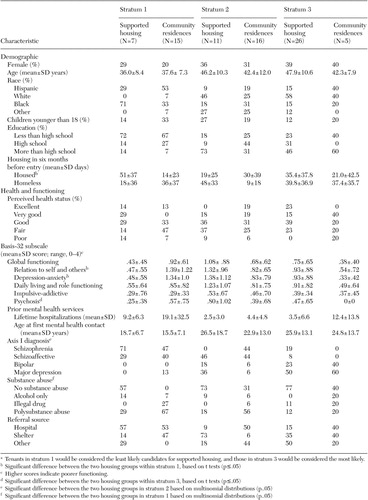 |
a Tenants in stratum 1 would be considered the least likely candidates for supported housing, and those in stratum 3 would be considered the most likely.
At baseline, in stratum 1 in both the intent-to-treat and true-stayer samples, persons in supported housing reported greater housing stability before study entry than those in community residences. They also had better Basis-32 scores on subscales measuring relation to self and others and depression-anxiety. They were also less likely to report previous use of substances. For the intent-to-treat sample only, persons in supported housing had better scores on the Basis-32 global score and on the psychosis subscale than those in community residences. In the true-stayer sample only, persons in supported housing were more likely to have been referred from hospitals and those in community residences were more likely to have been referred from shelters.
At baseline, in stratum 2 in the intent-to-treat sample, no statistical differences were found between tenants in housing models. In the true-stayer sample, proportionately more persons in supported housing had mood disorders and none had schizophrenia. At baseline, in stratum 3 in both the intent-to-treat and true-stayer samples, persons in supported housing had poorer psychosis scores.
Outcomes
Days in initial placement.Table 3 presents the model estimates of the percentage of tenants in each propensity stratum who remained housed in their initial placement at six, 12, and 18 months. Log-rank tests indicate that in each stratum, there was no statistical difference between the housing model survival curves. The estimated percentage of tenants still in initial placement at 12 months ranged among the strata from 72 to 87 percent for supported housing and from 62 to 71 percent for community residences. At 18 months, the range was 64 to 80 percent for supported housing and 37 to 71 percent for community residences.
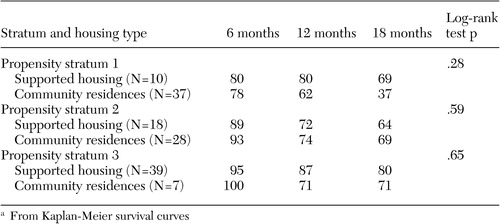 |
a From Kaplan-Meier survival curves
Although the differences are not statistically significant, the data suggest a comparatively longer time in initial placement for participants in supported housing in stratum 1. Several persons left community residences in less than 100 days, whereas in supported housing, the earliest exit occurred well after 100 days. By 18 months, 31 percent of those in supported housing were estimated to have left, compared with 63 percent of those in community residences. In stratum 3, exits from supported housing occurred later than in the other strata, with 80 percent estimated to still be in supported housing at 18 months, compared with 71 percent in community residences.
The Cox models, in agreement with the log-rank tests, showed no statistically significant impact on time in initial placement of the housing model, propensity stratum, or propensity-by-group interaction. Participants most likely to exit, in stepwise order, were younger, had less education, were more likely to have a diagnosis of bipolar disorder than any of the other diagnoses, and had more previous lifetime hospitalizations.
Housing satisfaction and clinical and well-being outcomes.Table 4 summarizes the significant treatment effects of housing model in relation to other outcome measures. This table combines findings from the intent-to-treat and true-stayer samples that resulted from the hierarchical linear approach. All estimates of the coefficients of each of the models are not displayed; however, we do indicate whether the treatment effect was significant (p<.05) at a given time point. In the table a significant treatment effect in the intent-to-treat analysis is denoted by an open box and by a partially filled box in the true-stayer analysis. A significant treatment effect in both analyses is denoted by a filled box. A plus sign indicates that the outcome in supported housing was significantly better than in community residences, and a minus sign indicates that the relationship was reversed. (More details of the statistical analysis can be obtained from the corresponding author.)
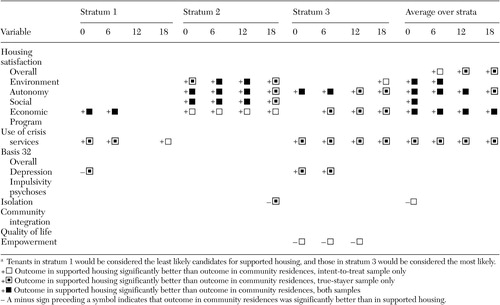 |
Housing satisfaction. For effect size averaged over strata and for each time point, the true stayers in supported housing reported significantly greater autonomy and economic satisfaction in regard to their housing than the true stayers in community residences. True stayers in stratum 2 were significantly more satisfied with their environments and socializing opportunities at each time point.
Clinical outcomes. For effect size averaged over strata and for each time point, the true stayers in supported housing had significantly less use of crisis services than those in community residences.
Well-being. In stratum 2, true stayers in supported housing reported significantly greater feelings of isolation than those in community residences at 18 months. At 12 months they also reported greater feelings of isolation, but the difference was not significant (p<.06). For propensity stratum 3, in the intent-to-treat analysis only, from baseline to 12 months those in supported housing reported significantly less empowerment than those in community residences.
Modifiers of outcome
Regression analyses indicated that many baseline covariates influenced outcomes (data not shown). We report here only on the mutable factors of depression-anxiety symptoms and substance abuse—and only if the factors had a significant impact on more than one outcome at more than one time point in the true-stayer analysis.
Higher baseline scores on depression-anxiety had sustained impact throughout the study period for persons in both housing models. As a result, people experienced less housing satisfaction, greater use of crisis services, more isolation, less community integration, less empowerment, and poorer quality of life. For both housing models, polysubstance abusers (persons who abused both alcohol and drugs) reported less community integration and less satisfaction with the autonomy and social aspects of their housing situation than did those who abused only alcohol. Polysubstance abusers also had higher overall Basis-32 scores than those who abused only drugs or who did not abuse substances.
Discussion
As a likely result of triage decisions made by the existing placement system, participants who enrolled in supported housing were less likely than those in community residences to have thought disorders and poly-substance abuse and also less likely to have extensive histories of hospitalization. Our study was not conducted to examine the appropriateness of the triaging system, a system that appears to place persons in housing according to their clinical histories. Rather, it was undertaken to compare the outcomes of similar tenants in two different housing models. If tenants had been randomly assigned to housing, the differences in clinical status may not have occurred. Propensity scoring was used to mimic randomization. It acted to balance the distribution of diagnoses in the true-stayer sample in strata 1 and 3 but not in stratum 2; it also balanced hospitalization histories in all strata in both analyses.
If we notionally interpret propensity strata as the system's view of appropriate placement, then the fact that stratum-specific survival curves did not differ by housing type—a robust finding across the two analyses—suggests that residential success may be independent of the triaging rules in place for housing referral. Undetectable differences may be due to small sample sizes. However, we note that the empirical data do suggest that in propensity stratum 1, tenants in supported housing were more likely to remain in their initial placement than their counterparts in community residences, which was not the case in strata 2 and 3. However, the survival curves of tenants in strata 2 and 3 appear very similar.
Demographic characteristics that are commonly reported to influence housing stability played no consistent role in this study. No gender differences were found. Being nonwhite did not have an impact on housing tenure. In contrast to what others have reported ( 19 , 38 ), younger tenants tended to fare worse than older ones. Mood disorders did affect tenure as expected ( 38 ), although bipolar disorder, rather than depression or anxiety, predicted the poorest outcomes.
Supported housing and community residences were markedly different in terms of fidelity scores on community integration and in rights of tenure, two critical measures of normalized housing. Tenants in supported housing reported having more physical autonomy and more pocket money after paying rent, perhaps a further reason for consumers' preference for this housing model ( 38 ). However, freedom can have its costs. At 18 months, supported housing tenants in the group deemed by the system to be moderately ready for supported housing (propensity stratum 2) reported greater feelings of isolation than their counterparts in community residences, a concern other commentators have voiced ( 11 , 15 , 16 , 39 ). The service and support functions of community residences may play a positive role, because tenants cannot remain isolated in their rooms, whereas in supported housing there is no requirement for engagement. Supported housing tenants in stratum 2 were more likely to have a diagnosis of major depression than of schizophrenia. More targeted efforts may be needed to facilitate socialization for this group.
The supported housing sites on average were half as costly to operate as the community residences. On the basis of the effectiveness measure chosen to assess cost-effectiveness, supported housing would appear either more cost-effective or at least less costly. However, tenants in both housing models used a broad spectrum of resources, which may indicate the successful influence of both housing models on their behavior. For a full assessment of housing costs, the cost of disparate resources must be integrated into a cost analysis, particularly if cost-effectiveness is to be judged. We are in the process of more fully specifying a cost-effectiveness model that expands the costs to include other social cost dimensions.
The strongest modifier of multiple outcomes was self-reported depression-anxiety at baseline. This clinical factor was correlated at many time points with housing dissatisfaction and other measures indicating poor outcome related to community living. We found poorer outcomes on several measures for those with a previous history of poly-substance abuse than for those who abused alcohol only. A link between poor outcomes, polysubstance abuse, and depression warrants further exploration.
Some limitations should be noted. A randomized design, which is preferable for causal inference, could not be employed, because of entry into the housing models from multiple portals. We addressed this limitation by using state-of-the-art statistical methods to allow appropriate hypothesis tests to be performed. Power considerations were influenced by the modest sample size. The size of the sample was constrained by the enrollment criterion that study participants be new entrants into the housing during the one-year study enrollment period, and turnover rates in the housing were low. The SAMHSA multisite study measured many outcomes by using instruments and systematic approaches to data collection developed during the closely monitored initiative ( 40 ). Its logic model posited many hypotheses. Although the study had sufficient power to detect differences for housing stability, an extremely small p value would have been required to statistically adjust for the multiple comparisons that were made. Because we did not protect for the familywise error rate, the findings should be viewed as providing directions for future targeted study.
Issues of generalizability also require discussion. Because sites were not randomly selected to be representative of the models, generalizations to other housing sites that use these models should be made with caution. Furthermore, our study examined two models of supported housing. Because the providers requested anonymity, it is not known whether the findings for supported housing would more aptly apply to only one or both of the models. In addition, some agencies may have experienced temporal changes in operation that could have affected the delivery of supports and services and hence outcomes. Furthermore, neighborhood features for the housing sites ( 41 , 42 ) and various characteristics of the housing itself, such as the role of case management or tenancy rights, were not included in the analyses of housing outcomes.
Conclusions
The study provides evidence that two particular models of supported housing were viable portals of entry into the community for persons with severe mental illness who were homelessness or newly released from the hospital. Even persons in supported housing who were more likely—or equally likely—to be referred to community residences remained stably housed in supported housing. However, our findings were similar to those of others: some persons in supported housing may benefit from socialization assistance to alleviate feelings of isolation. Of particular concern is that symptoms of depression and anxiety at baseline increased the risk of poor outcome independent of housing situation. This finding suggests a need for early screening and attentive clinical monitoring.
Acknowledgments
A research team of providers and consumers from participating housing and support agencies, researchers, and housing specialists is gratefully acknowledged for making this study possible and for input into design, analysis, and interpretation. Team members include Susan Barrow, Ph.D., New York State Psychiatric Institute; Peter Beitchman, D.S.W., The Bridge, Inc.; Steven Coe, B.A., Community Access, Inc.; Sabra Goldman, M.A., Association for Rehabilitative Case Management and Housing; Tony Hannigan, M.S.W, Center for Urban Community Services; Rosanne Haggerty, M.A., Common Ground Community H.D.F.C., Inc.; Lucy Kim, B.A., Center for Urban Community Services; Frank Lipton, M.D., New York City Human Resources Administration; Muzzy Rosenblatt, M.P.A., Bowery Residents' Committee, Inc.; Jody Silver, B.A., Community Access Inc.; and Sam Tsemberis, Ph.D., Pathways to Housing. The authors also thank Terry Hay for leadership in field work and Debra Rog, Ph.D., and Scott Holupka, M.S., Vanderbilt University, from the Substance Abuse and Mental Health Services Administration's cross-site leadership team for facilitation of this study.
1. Carling PJ: Access to housing: cornerstone of the American dream. Journal of Rehabilitation 55(5):6-8, 1989Google Scholar
2. Carling PJ: Housing, community support, and homelessness: emerging policy in mental health systems. New England Journal of Public Policy 8:281-295, 1992Google Scholar
3. Carling PJ: Housing and supports for persons with mental illness: emerging approaches to research and practice. Hospital and Community Psychiatry 44:439-449, 1993Google Scholar
4. Blanch AK, Carling P, Ridgeway P: Normal housing with specialized supports: a psychiatric rehabilitation approach to living in the community. Rehabilitation Psychology 33:47-55,1988Google Scholar
5. Ridgway P, Zipple AM: The paradigm shift in residential services: from linear continuum to supported housing approaches. Psychosocial Rehabilitation Journal, 13(4):11-32, 1990Google Scholar
6. Goering P, Paduchak D, Durbin J: Housing homeless women: a consumer preference study. Hospital and Community Psychiatry 41:790-794, 1990Google Scholar
7. Tanzman B: An overview of surveys of mental health consumers' preferences for housing and support services. Hospital and Community Psychiatry 44:450-455, 1993Google Scholar
8. Owen C, Rutherford V, Jones M, et al: Housing accommodation preferences of people with psychiatric disabilities. Psychiatric Services 47:628-632, 1996Google Scholar
9. Goldfinger SM, Schutt RK: Comparison of clinicians' housing recommendations and preferences of homeless mentally ill persons. Psychiatric Services 47:413-415, 1996Google Scholar
10. Bebout RR, Harris M: In search of pumpkin shells: residential programming for the homeless mentally ill, in Treating the Homeless Mentally Ill: A Task Force Report. Edited by Lamb HR, Bachrach LL, Kass FI. Washington, DC, American Psychiatric Association, 1992Google Scholar
11. Rosenson MK: Supported housing (letter). Hospital and Community Psychiatry 44:891, 1993Google Scholar
12. Lamb HR, Lamb DM: Factors contributing to homelessness among the chronically and severely mentally ill. Hospital and Community Psychiatry 41:301-305, 1990Google Scholar
13. Hatfield AB: A family perspective on supported housing. Housing and Community Psychiatry 44:496-497, 1993Google Scholar
14. Adler DA, Drake RE, Stern R: Viewing chronic mental illness: a conceptual framework. Comprehensive Psychiatry 24:192-207, 1984Google Scholar
15. Srebnik D, Livingston J, Gordon L, et al: Housing choice and community success for individuals with serious and persistent mental illness. Community Mental Health Journal 31:139-152, 1995Google Scholar
16. Dixon L, Krauss N, Myer, P, Lehman A: Clinical and treatment correlates of access to Section 8 certificates for homeless mentally ill persons. Hospital and Community Psychiatry 45:1196-1200, 1994Google Scholar
17. Pepper B. Where (and how) should young adult chronic patients live? The concept of a residential spectrum. TIE Lines 2:1-6, 1985Google Scholar
18. Fields S: The relationship between residential treatment and supported housing in a community system of services. Psychosocial Rehabilitation Journal 13(4):105-113, 1990Google Scholar
19. Rog DJ: The evidence on supportive housing. Psychiatric Rehabilitation Journal 27:334-344, 2004Google Scholar
20. Lipton FR, Siegel C, Hannigan A, et al. Tenure in supportive housing for homeless persons with severe mental illness. Psychiatric Services 51:479-486, 2000Google Scholar
21. Dickey B, Latimer E, Powers K, Gonzalez O, et al: Housing costs for adults who are mentally ill and formerly homeless. Journal of Mental Health Administration 24:291-305, 1997Google Scholar
22. Culhane DP, Metraux S, Hadley T: Public service reductions associated with placement of homeless persons with severe mental illness in supportive housing. Housing Policy Debate 13:107-163, 2002Google Scholar
23. Hurlburt MS, Wood PA, Hough RL: Providing independent housing for the homeless mentally ill: a novel approach to evaluating long-term longitudinal housing patterns. Journal of Community Psychology 24:291-310, 1996Google Scholar
24. Goldfinger SM, Schutt RK: Comparison of clinicians' housing recommendations and preferences of homeless mentally ill persons. Psychiatric Services 47:413-415, 1996Google Scholar
25. Hopper K, Barrow SM: Two genealogies of supported housing and their implications for outcome assessment. Psychiatric Services 54:50-54, 2003Google Scholar
26. Tsemberis S, Gulcur L, Nakae M: Housing first, consumer choice, and harm reduction for individuals who are homeless with dual diagnoses: a 24 month clinical trial. American Journal of Public Health 94:651-656, 2004Google Scholar
27. Jones K: CMHS Cross-Site Initiative Cost Analysis for the NYC Project Site. Orangeburg, NY, Nathan Kline Institute, 2001Google Scholar
28. Residential Follow-Back Calendar. Lebanon, NH, New Hampshire-Dartmouth Psychiatric Research Center, 1995Google Scholar
29. Tsemberis S, Rogers SE, Rodis E, et al: Housing satisfaction for persons with psychiatric disabilities. Journal of Community Psychology 31:581-590, 2003Google Scholar
30. Eisen SV, Dill DL, Grob MC: Reliability and validity of a brief patient-report instrument for outcome evaluation. Hospital and Community Psychiatry 45:242-247, 1994Google Scholar
31. Segal SP, Aviram U: The Mentally Ill in Community-Based Sheltered care. New York, Wiley, 1978Google Scholar
32. Russell D, Cutrona CE: UCLA Loneliness Scale Version 3, in Measures of Personality and Social Psychological Attitudes. Edited by Robinson JP, Shaver PR, Wrightsman LS. San Diego, Academic Press, 1991Google Scholar
33. Rogers ES, Chamberlin J , Ellison ML, et al: A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatric Services 48:1041-1047, 1997Google Scholar
34. Lehman AF: A quality of life interview for the chronically mentally ill. Evaluation and Program Planning 11:51-62, 1998Google Scholar
35. D'Agostino RB Jr: Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Statistics in Medicine 17:2265-2281, 1998Google Scholar
36. Rosenbaum PR, Rubin DB: The central role of the propensity score in observational studies for causal effects. Biometrika 70:41-55, 1983Google Scholar
37. Little RJ, Rubin DB: Causal effects in clinical and epidemiological studies via potential outcomes: concepts and analytical approaches. Annual Review of Public Health 21:121-145, 2000Google Scholar
38. Tsemberis S, Eisenberg RF: Pathways to housing: supported housing for streetdwelling homeless individuals with psychiatric disabilities. Psychiatric Services 51:487-493, 2000Google Scholar
39. Carling P: Return to Community, New York, Guilford, 1994Google Scholar
40. Rog DJ, Randolph FL: A multisite evaluation of supported housing: lessons learned from cross-site collaboration, in New Directions for Evaluation, 94: Conducting Multiple Site Evaluations in Real-World Settings. Edited by Herrell JM, Straw RB. San Francisco, Jossey-Bass, 2002Google Scholar
41. Saegert S, Evans GW: Poverty housing niches and health in the United States. Journal of Social Issues 59:569-589, 2003Google Scholar
42. Harkness J, Newman SJ, Salkever D: The cost-effectiveness of independent housing for the chronically mentally ill: do housing and neighborhood features matter? Health Services Research 39:1341-1360, 2004Google Scholar



