Medicaid Enrollment and Mental Health Service Use Following Release of Jail Detainees With Severe Mental Illness
The issue addressed here is whether being enrolled in Medicaid leads to an advantage in access to and receipt of services for persons with severe mental illness after their release from jail. Jails now process approximately 12.5 million bookings each year (Karberg J, personal communication, 2004), and best estimates suggest that approximately 8 percent (gender adjusted), or one million, of these bookings involve persons who have severe mental illness ( 1 , 2 , 3 ). These individuals are among the most vulnerable and needy persons in the public mental health system. However, no national data are currently available that describe their characteristics and experiences.
Jails detain many persons who have co-occurring mental illness and substance use disorders, a history of irregular contacts with community mental health agencies, and revolving-door detentions. Usually, jail stays are brief, with most persons released within 48 hours. However, in some jurisdictions, detainees with severe mental illness tend to stay four to six times longer than the average detainee ( 4 ). Often, their mental illness is a contributing factor to their offense, so timely access to appropriate mental health services after release may be crucial if they are to stabilize their psychiatric and functional conditions and avoid repeated revolving-door detentions in jail.
Research clearly shows that rates of access to health care for Medicaid beneficiaries are comparable to those for the privately insured population and much greater than those for the uninsured ( 5 , 6 ). But much less is known about the effects of Medicaid on access to and use of services by persons with severe mental illness ( 7 , 8 , 9 , 10 , 11 ), especially for the many thousands each year who are arrested and detained in jails throughout the United States.
Medicaid is the principal insurance program and payer of mental health services for persons with severe mental illness ( 12 ), now amounting to more than half of the public mental health services administered by the states ( 13 , 14 ). In a recent national study of adults, Wells and colleagues ( 15 ) reported that the likelihood of using services for alcohol abuse, drug abuse, and mental health care was highest for Medicaid beneficiaries and lowest for the uninsured.
Current research is unclear as to whether the advantage gained by the general Medicaid population in access to and use of services extends to persons with severe mental illness coming out of jail. It may well be—as reported for other vulnerable groups, such as children ( 16 ) and homeless persons ( 17 , 18 )—that among persons with severe mental illness, Medicaid offers no particular advantage in obtaining mental health services upon release from jail. The possible Medicaid advantage accrues from the basic value of any insurance program—that is, it provides a way to pay for treatment services received, thus making the recipient more attractive to service providers. Even though the social safety net for uninsured persons has been eroding throughout the United States in recent years, mental health block grant funding from the federal government to the states for local outpatient providers and the bad-debt and charity subsidies for general hospitals are ways that uninsured persons can receive free mental health care. But no reports have been published as to which of these scenarios applies for persons with severe mental illness after release from jail.
Here, we report findings that focus directly on the possible advantages of Medicaid enrollment for this population. Three hypotheses were tested. We hypothesized that compared with persons who were not enrolled in Medicaid at the time that they were released from jail, those who were enrolled at the time of release would have a higher probability of receiving community-based mental health services, having shorter lengths of time to first service contact in the community, and having more service utilization in the 90 days after release.
Methods
This study employed a prospective cohort design that used administrative data from two large urban counties over two years to examine the access to and use of community mental health services after the release from jail for persons with severe mental illness, by Medicaid status at the time of release.
Study sites
The study was carried out in Pinellas County, Florida, and King County, Washington. These two sites were selected because of the availability of administrative data that could be linked on a person-specific basis across multiple agencies.
In 2000 King County had about twice as large a population as Pinellas County and a 43 percent higher median income ( Table 1 ). In Pinellas, the population is concentrated in two midsize cities (St. Petersburg and Clearwater); in King County, the population is concentrated in one principal city (Seattle), but about two-thirds of the population is spread across a number of smaller cities and unincorporated areas. Both counties are largely white; compared with King County, Pinellas County has a somewhat larger percentage of blacks, a smaller percentage of Asians, and about the same percentage of Hispanics or Latinos.
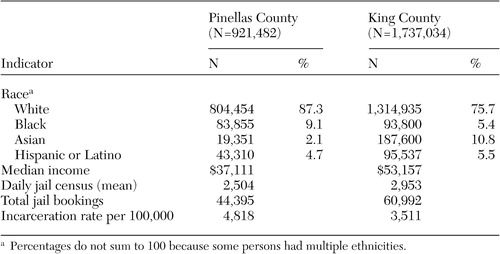 |
According to Bureau of Justice Statistics reports ( 19 ), in 2000 the Pinellas County jail ranked 33rd and the King County jail ranked 34th on the list of largest jail jurisdictions in the United States. The average daily jail census was about 18 percent larger and the total number of jail bookings was about 37 percent larger in King County than in Pinellas County. However, the incarceration rate per 100,000 was greater in Pinellas County.
Sample description
For each county, administrative data were used to identify all persons with severe mental illness who were enrolled in Medicaid and had at least one jail detention within a 24-month study interval. In King County the interval was October 1996 through September 1998 and in Pinellas County it was October 1998 through September 2000.
In Pinellas County, data on jail detentions, Medicaid enrollment, and psychiatric diagnoses were obtained through the Pinellas County Data Collaborative, an interagency data repository managed by staff at the Louis de la Parte Florida Mental Health Institute, University of South Florida. All data were used pursuant to the process established by an inter-local agreement designed to allow cross-system comparisons, while ensuring data security and individual confidentiality. In King County, these same data elements were assembled by the research team as part of an ongoing study ( 20 ). The study protocol was reviewed for human subjects' protection by institutional review boards at the home institutions of the investigators.
A common logic of sample enumeration was followed at each site, but data sources and linkage varied somewhat. For Pinellas County, the sample was limited to Medicaid enrollees who participated in MediPass (primary care case management program) to avoid the problem of missing claims data that has been found for health maintenance organizations and other capitated providers ( 21 ). A person-specific data file identifying beneficiaries with severe mental illness and Medicaid enrollment during the study interval was obtained from the state of Florida's Medicaid claims files (through the Pinellas Data Collaborative) and then linked with an incarceration file for jail stays during the study interval. The incarceration file was obtained from the Pinellas County Criminal Justice Information System.
For King County, Medicaid enrollment data were available to the research team, but individual claims data were not. Consequently, severe mental illness status was determined from county outpatient mental health records. A person-specific file identifying persons with severe mental illness who had at least one contact in these county service records during the study interval was first run against the Medicaid files to identify enrollment status and then run with an incarceration file from the King County jail to identify the final sample.
The data were grouped into two cohorts within each county: detentions for persons with severe mental illness who were enrolled in Medicaid on the day that they were released from jail and detentions for persons with severe mental illness who were not enrolled in Medicaid on the day that they were released from jail.
It is important to note that all persons in both cohorts were enrolled in Medicaid at some time during the two-year study interval. Persons can lose Medicaid benefits for a variety of reasons, so that on a subsequent arrest they might either be enrolled or not enrolled in Medicaid. Here, the persons in the non-Medicaid cohort were those who either lost enrollment or had not yet been enrolled on the date of their jail release. This sampling design attempted to control for Medicaid eligibility and to ensure that the two cohorts within each county were roughly comparable on disability status and financial need. Indeed, further checking revealed that in our sample, 1,581 (87 percent) persons in King County and 955 (79 percent) in Pinellas County were on Supplemental Security Income or Social Security Disability Insurance.
The following DSM-IV codes were used to define severe mental illness: schizophrenia (295), affective disorders (296, excluding 296.2 for single-episode depression), delusional disorder (297.10), and psychotic disorder not otherwise specified (298.9). Individuals who had diagnoses of severe mental illness at any point in the study, irrespective of when those diagnoses occurred, were treated as having severe mental illness for the entire study period. Thus some individuals may have been given a diagnosis after their incarcerations; however, an assumption was made that severe mental illness was a fixed condition for the individuals in this study. The rationale behind this assumption was that severe mental illness is a recurring and often persistent condition that manifests itself before and certainly after a formal diagnosis.
Measures of service access and use
In Pinellas County, data on service contacts were available through Medicaid claims as well as through the Florida Department of Children and Families' Information Data System Data Warehouse (IDSDW). Providers who have contracts with the department to provide mental health and substance abuse services are required to report service utilization through the IDSDW system. To capture the full range of postjail service contacts for persons in our sample, we accessed data from Medicaid claims and from IDSDW records. In King County, we did not have access to Medicaid claims, so service contacts for persons in the Medicaid and non-Medicaid cohorts were identified through the county mental health and statewide substance abuse information systems (Treatment and Assessment Report Generation Tool, or TARGET). Contract providers in King County and the state of Washington are required to report service utilization data through these information systems.
The analyses focus on the first 90-days after jail release as a critical period for receipt of services in the community. Access was measured as any service contact within the 90-day window. A service contact was defined as any recorded event, whether it was for a 15-minute clinic visit or a day-long treatment program. For Pinellas County, the number of services received was created by a count of units of service in Medicaid claims and utilization reports from the IDSDW; for King County, the count was units of service reported in the county mental health and TARGET substance abuse reporting systems. Days to first service was measured as the number of days between date of jail release and date of first service contact. Rate of service was computed by dividing the number of services received by available "exposure" days—90 days minus the number of days each person was incarcerated or hospitalized within this period.
Analyses
All analyses presented below are based on detentions, rather than unique persons. Thus any one person may have had several detentions. Analyzing the data in this way enabled us to determine the impact of Medicaid enrollment on service receipt after each jail release. To address the potential for dependence among observations, in each statistical model standard errors were adjusted for repeated observations at the individual level.
A series of regression models were run with the four dependent variables (probability of use, days to first service, number of service days, and rate of service use) separately for each county, with Medicaid enrollment status as the explanatory variable. Next, the coefficients from each regression model were used to adjust their respective point estimates for each county for each of the four dependent variables and to test for differences among these variables between Medicaid and non-Medicaid cohorts within each county. These adjustments were made for race, gender, age, diagnosis, length of incarceration, and prior substance abuse treatment.
Probability of service use was estimated with a logistic regression model based on receipt of services within 90 days (yes or no) for the total sample. Days to first service was estimated with an ordinary least-squares regression model for the subgroup that had accessed services within 90-days. Amount of service use was examined with a negative binominal regression model both for the total sample and for the subsample of persons who used services. Rate of service use was estimated with an ordinary least-squares regression model for the total sample and for the subsample of persons who used services. All statistical models were implemented by using SAS software.
Results
A total of 1,210 persons who had 2,878 detentions were identified in Pinellas County: 2,215 of these detentions represented persons enrolled in Medicaid and 663 represented those without Medicaid. For King County, the corresponding numbers were 1,816 persons and 4,482 detentions: 2,752 of these detentions represented persons enrolled in Medicaid and 1,730 represented those without Medicaid.
Table 2 presents the characteristics of the two cohorts (enrolled or not enrolled in Medicaid) at each site. Overall, the Medicaid and non-Medicaid groups were fairly homogeneous on these indices within the county, but there were some between-county sample differences. The King County sample has about 8 to 9 percent more men and 10 percent more blacks than the Pinellas County sample. The average age at the time of release from jail was approximately the same across groups and counties.
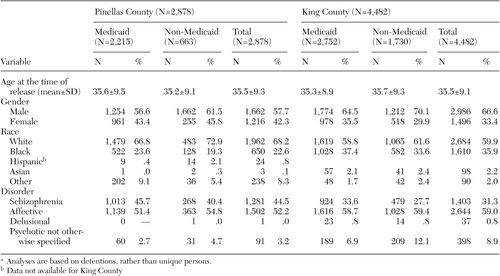 |
a Analyses are based on detentions, rather than unique persons.
Schizophrenia and affective disorders accounted for at least 90 percent of the sample in both counties ( Table 2 ). However, there are some compositional differences between the two counties. Although the predominant diagnosis in both counties was affective disorders, more individuals in the King County sample had this diagnosis (59 percent compared with 52 percent). Schizophrenia diagnoses occurred more frequently in the Pinellas County sample than in the King County sample (45 percent compared with 31 percent). This difference was offset somewhat by the greater frequency of psychotic disorders not otherwise specified in the King County sample (9 percent compared with 3 percent).
As shown in Table 3 , the probabilities of any service use for persons with and without Medicaid in the 90 days after release from jail were consistent with the first study hypothesis. In both counties, participants with Medicaid were much more likely to access services (p<.001). The relative advantage was similar in both counties; in Pinellas County, the Medicaid group was 1.6 times as likely as the non-Medicaid group to access services (59 percent of sample that used any service compared with 37 percent) and in King County, the Medicaid group was 1.25 times as likely to access services (70 percent of sample that used any service compared with 56 percent).
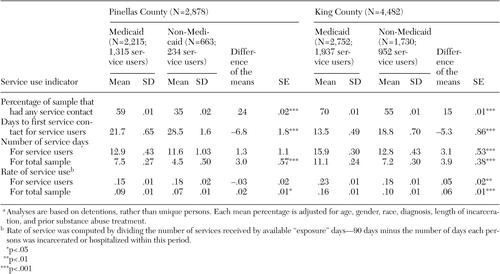 |
a Analyses are based on detentions, rather than unique persons. Each mean percentage is adjusted for age, gender, race, diagnosis, length of incarceration, and prior substance abuse treatment.
Consistent with the second study hypothesis, participants enrolled in Medicaid had a shorter length of time to first service in the community ( Table 3 ). In Pinellas County, the average lag time to first service contact was about three weeks (21.7 days) for the Medicaid group and four weeks (28.5 days) for the non-Medicaid group, yielding a 6.8-day advantage for the Medicaid group (p<.001). In King County, the corresponding figures were 13.5 and 18.8 days, for a 5.3-day advantage (p<.001).
However, the time to first service was somewhat positively skewed for each county. In King County, 50 percent of participants who received a service did so within four to six days of release, with the remainder spread across the subsequent seven to 90 days. In Pinellas County, the corresponding figures were 50 percent within ten to 17 days of release, and the remainder was spread over the subsequent 18 to 90 days. In both counties, a sizeable percentage did not receive any services at all within the 90-day period (36 percent in King County and 46 percent in Pinellas County).
Given that the distribution of the time to first service is right-censored, we next ran a Cox proportional hazards regression model for the total sample, allowing for the possibility of multiple detentions for persons ( 22 ). The relative risks obtained from the Cox model indicated that in the King County jail, detainees released with Medicaid received their first service contact 62 percent more quickly than those released without Medicaid, whereas in Pinellas County detainees received a service 39 percent more quickly if they were released with Medicaid.
Finally, the results for days of service and rate of service use ( Table 3 ) are displayed both for the total sample and for the subgroup that actually used services. When the total sample is the focus, the results are consistent with the third hypothesis—in both counties, participants with Medicaid received significantly more days of service compared with those without Medicaid (7.5 days compared with 4.5 days in Pinellas County and 11 days compared with seven days in King County, p<.001) and at higher rates of service use (.09 compared with .07 in Pinellas, p<.05; .16 compared with .10 in King County, p<.001). When we focused on only the subgroup that used services, the results were the same for King County, but for Pinellas County the differences between the Medicaid and non-Medicaid groups were not significant.
Discussion
The findings of this study confirm that in both counties, persons with severe mental illness who are enrolled in Medicaid at the time of their release from jail are more likely to access community services, to receive services more quickly, and to receive more days of service than those without Medicaid in the 90 days after their release from jail. The policy implications of these findings for jail administrators, Medicaid directors, and mental health authorities are clear—efforts to avoid interruptions in Medicaid enrollment for persons with severe mental illness who are detained in jail will likely help them obtain needed community treatment services after release.
Our companion article ( 23 ) in this issue of Psychiatric Services indicates that short jail stays allowed jail detainees to retain their Medicaid benefits while incarcerated. In combination with the findings reported here, this suggests that in-jail interventions designed to enroll or keep people on Medicaid might be more effectively used by focusing on high risk persons before the point of arrest and jail detention. Either way, the results here make it clear that having Medicaid is an advantage for persons with severe mental illness in receiving timely services following release from jail.
The Medicaid advantage was not uniform in each county, however. On average, both Medicaid and non-Medicaid groups released from jail in King County were more likely to receive services, to receive them faster, and to obtain more days of service than their counterparts released from jail in Pinellas County.
These differences could be due to discrepancies in the data sources used in each county. In Pinellas County, Medicaid claims and a state-operated service contact reporting system were linked to obtain information on Medicaid and non-Medicaid service users, whereas in King County, claims data were not available to us, so all service contact information came from county mental health, state hospital, and substance abuse service reporting systems. Any biases resulting from missing data that might exist in these record systems would likely be constant within county but variable between counties; therefore, the between-county differences could be artifacts of underreporting.
An alternative interpretation for these differences is that there was a broader and more encompassing social safety net in King County in the late 1990s, compared with Pinellas County. This interpretation is supported by our other research focusing on managed mental health care and use of jails by persons with mental illness in King County ( 20 ). When King County introduced its Prepaid Health Plan in April 1995 as part of its behavioral health Medicaid carve-out, it established a case-rate payment system that attempted to achieve a seamless service system, so providers would serve Medicaid and non-Medicaid clients alike—that is, according to their needs irrespective of their insurance status or ability to pay. The state Medical Assistance Administration (Medicaid) allowed savings from managed care to be re-allocated to serving non-Medicaid, uninsured consumers ( 24 ). The fee-for-service Medicaid system in Pinellas County did not contain such provisions. So the differences in probability and intensity of service use reported here might reflect these differences in the way Medicaid was managed in the two counties.
In the aftermath of the September 11, 2001, terrorist attacks and the declining national economy, the fiscal status of state and county governments throughout the United States has been threatened and many health and welfare services have been trimmed. In the late 1990s, for example, King County began reducing the proportion of uninsured persons that could be carried by community providers, and in 2002 all non-Medicaid enrollments in Pre-Paid Health Plan were closed in King County. It is unclear whether the robustness of the social safety net in King County described here has survived these reductions. Because it is possible that these reductions have affected the uninsured more directly than persons enrolled in Medicaid, the large advantage for the non-Medicaid group in King County, compared with Pinellas County, is likely to have diminished.
Other limitations of this research should be acknowledged. It was an observational study in two counties. The absence of randomization precludes a clear inference that Medicaid per se accounts for the positive effects observed on timely access to and use of services. People currently enrolled in Medicaid could be sicker or more persistently sick, or they could be more likely to have existing providers. Either having greater levels of sickness on unmeasured variables or having an established provider relationship, rather than Medicaid per se, could account for some or all of the results. Also, the demographic characteristics of these two counties and jails do not mirror the national populations. On the other hand, the study followed two large cohorts prospectively for two years. Furthermore, these are the best data now available to answer important questions about a pressing national policy issue.
Another caveat should be noted—these data refer to jails, not to prisons. Prisons are long-stay institutions and virtually all prison inmates lose Medicaid and other Social Security benefits during their incarceration. Because of this regulation, special efforts are required to help inmates reacquire Medicaid before their release ( 25 , 26 ). It is reasonable to infer that Medicaid would have the same service use advantages for released prisoners with severe mental illness as those described here for released jail detainees, but confirmation of this advantage for prisoners awaits further follow-up research on prisoners released to the community.
Conclusions
Among persons with severe mental illness, those who have Medicaid upon jail release will make more timely and more extensive use of community-based services than those without Medicaid benefits. On this basis, it does not make good public policy sense to disenroll persons with severe mental illness from Medicaid when they are in jail. Whether engagement in services after jail release protects persons with severe mental illness from future arrests and jail detentions is another important question, but one that cannot be answered from the data reported here. That question will be the subject of a future report. For now, we can clearly say that the advantages of Medicaid for general health care service use that have been reported in other studies do carry over to persons with severe mental illness who are released from jail.
Acknowledgments
This research was supported by grant funding from the John D. and Catherine T. MacArthur Foundation's Mental Health Policy Research Network and from grant MH-63883 from the National Institute of Mental Health. For assistance in assembling the administrative data for this study, the authors thank the Pinellas County Data Collaborative; the Pinellas County Mental Health and Substance Abuse Leadership Group; the King County Mental Health, Chemical Abuse, and Dependency Services Division; the King County Department of Adult and Juvenile Detention; the King County Department of Public Health; the Washington State Department of Social and Health Services Divisions of Mental Health, Alcohol and Substance Abuse and Medical Assistance Administration; and the Washington State Department of Health's Center for Health Statistics. The helpful comments of Richard Frank, Ph.D., and Sherry Glied, Ph.D., on an earlier draft of this article are also gratefully acknowledged.
1. Teplin LA: The prevalence of severe mental disorder among urban male detainees: comparison with the Epidemiologic Catchment Area program. American Journal of Public Health 8:663-669, 1990Google Scholar
2. Teplin LA, Abram KM, McClelland GM: The prevalence of psychiatric disorder among incarcerated women: pretrial jail detainees. Archives of General Psychiatry 53:505-512, 1996Google Scholar
3. The Prevalence of Co-occurring Mental Illness and Substance Use Disorders in Jails. Delmar, NY, National GAINS Center for People With Co-occurring Disorders in the Justice System, 2002. Available at http://gainscenter.samhsa.gov/pdfs/disorders/gainsjailprev.pdfGoogle Scholar
4. Axelson G, Wahl O: Psychotic versus non-psychotic misdemeanants in a large county jail: an analysis of pretrial treatment by the legal system. International Journal of Law and Psychiatry 15:379-386, 1992Google Scholar
5. Davis K, Schoen C: Health and the War on Poverty: A Ten-Year Appraisal. Washington, DC, Brookings Institution, 1978Google Scholar
6. Marquis M, Long S: Reconsidering the effect of Medicaid on health care service use. Health Services Research 30:791-808, 1996Google Scholar
7. Horgan C: The demand for ambulatory mental health services from specialty providers. Health Services Research 21:291-319, 1986Google Scholar
8. Taube C, Rupp A: The effect of Medicaid on access to ambulatory mental health care for the poor and near-poor under 65. Medical Care 24:677-686, 1986Google Scholar
9. Weinick R, Zuvekas S, Drilea S: Access to Health Care: Sources and Barriers, MEPS Research Findings No 3. Rockville, Md, Agency for Health Care Policy and Research, 1997Google Scholar
10. Zuvekas S: Health insurance, health reform, and outpatient mental health treatment: who benefits? Inquiry 36:127-146, 1999Google Scholar
11. McAlpine D, Mechanic D: Utilization of specialty mental health care among persons with severe mental illness: the roles of demographics, need, insurance, and risk. Health Services Research 35:277-292, 2000Google Scholar
12. Frank RG, Goldman HH, Hogan M: Medicaid and mental health: be careful what you ask for. Health Affairs 22(1):101-113, 2002Google Scholar
13. Smith V: Making Medicaid better: options that would bring the program up to date in today's health care marketplace and allow states to continue to participate. Prepared for the National Governors' Association. Lansing, Mich, Health Management Associates, 2002. Available at www.nga.org/cda/files/makingmedicaidbetter.pdfGoogle Scholar
14. Buck J: Medicaid, health care financing trends, and the future of state-based public mental health services. Psychiatric Services 54:969-975, 2003Google Scholar
15. Wells K, Sherbourne C, Sturm R, et al: Alcohol, drug abuse, and mental health care for uninsured and insured adults. Health Services Research 37:1055-1066, 2002Google Scholar
16. Feinberg E, Swartz K, Zaslavsky A, et al: Family income and the impact of a children's health insurance program on reported need for health services and unmet health need. Pediatrics 109:1-10, 2002Google Scholar
17. Glied S, Hoven C, Moore R, et al: Medicaid and service use among homeless adults. Inquiry 35:380-388, 1998Google Scholar
18. Burt M, Sharkey P: The Role of Medicaid in Improving Access to Care for Homeless People. Washington, DC, Urban Institute, 2002Google Scholar
19. Beck A, Karberg J: Prison and Jail Inmates at Midyear 2000, in Bureau of Justice Statistics Bulletin. NCJ 185989. Washington, DC, US Department of Justice, 2001Google Scholar
20. Domino M, Norton E, Morrissey J, et al: Cost shifting to jails after a change to managed mental health care. Health Services Research 39:1379-1401, 2004Google Scholar
21. Wooldridge J, Hoag S: Challenges to Developing and Using Encounter DATA in Five Medicaid Managed Care Programs. Report submitted to Health Care Financing Administration, Baltimore, Md, contract no 500 94 0047, ref no 8240-908. Princeton, NJ, Mathematica Policy Research, 2001Google Scholar
22. Wei LJ, Lin DY, Weissfeld L: Regression analysis of multivariate incomplete failure time data by modeling marginal distributions. Journal of the American Statistical Association 84:1065-1073, 1989Google Scholar
23. Morrissey JP, Dalton KM, Steadman HJ, et al: Assessing gaps between policy and practice in Medicaid disenrollment of jail detainees with severe mental illness. Psychiatric Services 57:803-808, 2006Google Scholar
24. Jarvis D, Mauer B: White Paper: Potential Impact of the Final Rules for Medicaid Managed Care on the Washington Public Mental Health System. Seattle, MCPP Healthcare Consulting, 2003Google Scholar
25. Re-entry Policy Council: Charting the Safe Return of Prisoners to the Community. Lexington, Ky, Council of State Governments, 2005. Available at http://www.reentrypolicy.org/rp/main.aspxGoogle Scholar
26. Arrested? What Happens to Your Benefits If You Go to Jail or Prison? A Guide to Federal Rules on SSI, SSDI, Medicaid, Medicare and Veterans Benefits for Adults With Disabilities. Washington, DC, Bazelon Center for Mental Health Law, 2004. Available at www.bazelon.org/issues/criminalization/publications/arrested/index.htmlGoogle Scholar



