Effect of Maternal Mental Health Problems on Child Treatment Response in Community-Based Services
A large body of evidence indicates that children of mothers with mental health disorders are at increased risk for emotional and behavioral problems ( 1 ) that could severely impair their functioning and development ( 2 ). Although clinical treatment has proven effective for children with mental health problems ( 3 ), little is known about the impact of maternal mental health problems on children's response to treatment in a community setting.
Our previous research has shown that mothers bringing children to community clinics for mental health services have very high need for mental health services themselves ( 4 ). This research also demonstrated that children of mothers with mental health problems were significantly more impaired than children of mentally healthy mothers at time of treatment presentation and follow-up. In addition, these children improved at a slower rate than children of mentally healthy mothers; however, this difference did not reach a level of statistical significance ( 5 ).
A critical issue in community research is generalizability of findings. This study extends our prior work to a new, larger, and demographically diverse sample of clients from different community mental health clinics to further examine the impact of maternal mental health status on child treatment response. Both studies used structured survey measures to compare the rate of improvement in community treatment between children of mothers with and without mental health problems. By extending our prior work we can be better assured that the results are generalizable to other community clinic populations.
Methods
Mothers were recruited when their child came in for treatment at one of three community mental health centers. One of these three centers included a subsite with a low volume of clients. Requirements for eligibility for the study included being the biological or adoptive mother of the child, residing with the child, and cognitive status that enabled both mothers and children to complete the research protocol. Two of the centers were located in urban areas, and one was in a semirural community. The centers offer a wide range of services to communities with high rates of poverty and unemployment. The recruitment period was June 2001 through July 2004. Of the mothers approached during this period, 345 (54 percent) were recruited into the study. The baseline assessment process was completed by 345 mother-child pairs. Of these, 272 mother-child pairs were still available for a three-month follow-up, with each site contributing 149 pairs, 86 pairs (of these, the subsite contributed 13), and 37 pairs for this study. All procedures were approved by the university's institutional review board.
Demographic characteristics were self-reported by participants. A slight majority of children (148 children, or 54 percent) were male. Children ranged in age from four to 18 years, with a mean±SD age of 11.3±3.5. Mothers ranged in age from 21 to 62 years, with a mean age of 38.7±8.8. Most participants (199 mothers, or 73 percent) identified themselves as white, 66 women (24 percent) identified themselves as African American, one as Asian, two as Hispanic, two as American Indian, and two as "other." A majority of mothers (152, or 56 percent) reported a household income of $20,000 a year or less.
The sample recruited for the study reported herein differs from the one we used previously to examine the rate of improvement in community treatment between children of mothers with and without mental health problems ( 5 ). The 180 mother-child pairs in the previous study were all recruited from one community mental health clinic. In contrast, the sample used in this study was larger (272 mother-child pairs compared with 180), more racially diverse (24 percent African American compared with 11 percent), and more urban than the sample recruited for the first study (45 percent urban compared with 100 percent rural) ( 5 ). In addition, the clinic sites used in the current study were in no way affiliated with the one site examined in the previous study and were likely to have mechanisms of service delivery that differ from each other and from the site in the previous study. This additional demographic and treatment diversity is important in generalizing the findings.
Children's emotional and behavioral problems were assessed when they first came in for treatment and again three months later with the Child Behavior Checklist (CBCL), which the mothers completed ( 6 ). The CBCL includes 118 problem behavior items that create a total problems score and two broadband scores of internalizing and externalizing behavior. Scores on the scales are reported as T scores standardized to have a mean of 50 and a standard deviation of 10, with higher scores indicating greater problem behaviors. Our previous work demonstrates that mothers' CBCL ratings of their children are valid when compared with clinicians' assessments via structured interviews ( 5 , 7 ). Maternal mental health status was assessed at baseline with the Patient Health Questionnaire ( 8 ), a self-report measure designed to facilitate the recognition and diagnosis of the most common mental health disorders of primary care patients: depression, anxiety, eating disorders, and alcohol abuse. Each subscale score indicates the presence or absence of a particular disorder (such as panic disorder or major depressive disorder).
A substantial proportion of mothers (155, or 57 percent) met criteria for one or more mental health disorders according to the baseline Patient Health Questionnaire scores. Depression and anxiety disorders were the most common, with 113 (42 percent) mothers meeting criteria for depression and 109 (40 percent) meeting criteria for an anxiety disorder. Twenty-eight mothers (10 percent) met criteria for alcohol abuse, and 18 (7 percent) met criteria for an eating disorder. This high percentage of mothers with mental health problems is consistent with our previous work ( 4 ) showing that this population of mothers has a high need for mental health services.
The 73 mother-child pairs who dropped out of the study were compared with the 272 pairs who completed both assessments. The results of this analysis indicate no statistically significant differences in demographic characteristics of the two groups. However, mother-child pairs who dropped out of the study were less symptomatic at baseline than those who remained in the study.
An analysis of variance (ANOVA) was conducted for the child outcomes on the basis of total, externalizing, and internalizing CBCL scores. The ANOVA model included effects for maternal mental health status, time, and the interaction of the two variables. Maternal mental health status was determined by the presence or absence of any of the mental health disorders assessed by the Patient Health Questionnaire. The beta coefficient for the interaction of time with maternal diagnostic status represents the difference in slopes between baseline and follow-up for children of mothers with or without a mental health disorder—that is, the average change in CBCL score over time that is attributable to maternal mental health status.
Results
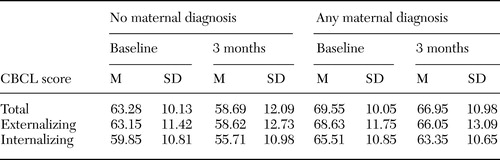
Children brought to the community clinics had a clear need for mental health treatment. The mean CBCL total score for children at baseline was 66.9±10.5, with a mean externalizing score of 66.3±11.9 and a mean internalizing score of 63.0±11.2. These scores are similar to those seen in other clinical populations ( 9 ) and are considered to be in the borderline to at-risk range ( 6 ).
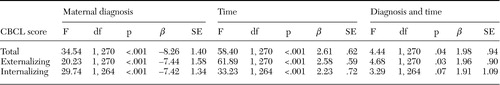
The unadjusted mean scores in Table 1 show that treatment was associated with a reduction in children's mental health symptoms and that children of mothers with mental health problems had significantly greater total behavior problems, externalizing behavior problems, and internalizing behavior problems at both baseline and follow-up. The results of the ANOVA models ( see Table 2 ) indicate significant main effects of both time and maternal mental health status. Moreover, the interaction between time and maternal mental health status was statistically significant for the total CBCL score, indicating that children of healthy mothers improved, on average, an additional 2 total CBCL points between baseline and follow-up compared with children of mothers with mental health disorders. The ANOVA interaction term was also statistically significant for externalizing CBCL scores and was marginally significant for internalizing CBCL scores. The magnitude of the interaction coefficients was about two points for these outcomes as well. The relationships between maternal mental health status and child treatment response were not significantly changed by including potential control variables, including child age and gender, maternal age and marital status, and recruitment site (data not shown).
 |
 |
Discussion
This study examined the impact of maternal mental health status on child treatment response in a community mental health setting by comparing children of mothers with and without mental health problems. The study replicates and extends our previous work into a larger, more demographically and clinically diverse population, further supporting earlier findings that children of mothers with mental health problems demonstrate significantly more behavior problems at both baseline and follow-up than children of mentally healthy mothers ( 5 ). The larger sample size in this study provides statistical support for the finding that children of mothers with mental health problems improved at a slower rate throughout treatment than children of mentally healthy mothers.
This finding is even more powerful given that the internal validity threat of regression toward the mean suggests that children beginning the study with more extreme scores (greater behavior problems) would likely show a steeper rate of improvement than would children beginning the study with less extreme scores. Our results indicate the opposite: children with more extreme scores at the beginning of treatment—that is, the children of mothers with mental health problems—demonstrated less improvement than children with less extreme scores at baseline—the children of mentally healthy mothers.
Examining the beta coefficients of the interactions of time and maternal diagnostic status ( Table 2 ) between this study and the previous one ( 5 ) allows us to compare the magnitude of the effect of maternal mental health problems on child treatment response, regardless of whether the effect reached the level of statistical significance. By comparing these coefficients, we found that the beta for the CBCL total problems scale, at 2.37 in the previous study, was actually slightly larger than the one found in the study reported herein (β=1.98), even though the effect did not reach the level of statistical significance in the earlier work. A similar phenomenon occurred for child improvement on the basis of the CBCL internalizing scale, as seen by a beta coefficient of 2.89 in the earlier study and 1.91 in the current study. However, the effect of maternal mental health status on change in children's externalizing scores was slightly stronger in this study, as seen by a beta coefficient of 1.96, compared with 1.32 in the earlier study. These comparisons demonstrate that the larger sample size (272 compared with 180) likely provided the additional power needed to detect statistical significance even though the magnitude of the effect was similar in the two studies.
Our ongoing work focusing on the mental health needs of low-income mothers who bring in their children for community mental health services indicates that mothers believe their own mental health symptoms will improve if their children, who are struggling with emotional and behavior problems, improve ( 10 ). This study, along with numerous others ( 11 , 12 ), suggests that the mental health of mothers and children is closely linked. Approaches that address mothers' as well as children's needs may be helpful and appropriate for these families. Structural family therapy, developed by Minuchin and colleagues ( 13 , 14 ), was intended to specifically address the needs of low-income families treated in community mental health settings. Despite enthusiasm for this model among practitioners, formal research documenting the effectiveness of the model has been limited and has mostly addressed adolescent drug use among Hispanic youths ( 15 ). Although the efficacy and effectiveness of family therapies are underresearched, these approaches have great promise for families whose children are experiencing mental health problems. At the very least, family approaches in community mental health provide an opportunity to identify mothers in need of treatment and provide them, as well as their children, with services.
Conclusions
Children of mothers with mental health problems had significantly greater behavior problems than children of mentally healthy mothers at both the time of treatment initiation and at the three-month follow-up. Moreover, these children demonstrated less improvement over time than did children of mentally healthy mothers. This finding suggests that treating the mental health needs of mothers, perhaps in conjunction with those of their children, may improve children's treatment response in community mental health settings.
Acknowledgments
This research was supported by National Institute of Mental Health grants R24-MH-56858 and R24-MH-61712.
1. Downey G, Coyne JC: Children of depressed parents: an integrative review. Psychological Bulletin 108:50-76, 1990Google Scholar
2. Mental Health: A Report of the Surgeon General. Washington, DC, US Department of Health and Human Services, 1999Google Scholar
3. Weisz JR, Weiss B, Han SS, et al: Effects of psychotherapy with children and adolescents revisited: a meta-analysis of treatment outcome studies. Psychological Bulletin 117:450-468, 1995Google Scholar
4. Swartz H, Shear MK, Wren FJ, et al: Depression and anxiety among mothers bringing their children to a pediatric mental health clinic. Psychiatric Services 56:1077-1083, 2005Google Scholar
5. Rishel CW, Greeno CG, Marcus SC, et al: Impact of maternal mental health status on child mental health treatment outcome. Community Mental Health Journal, in pressGoogle Scholar
6. Achenbach TM, Edelbrock CS: Manual for the Child Behavior Checklist and Revised Child Behavior Profile. Burlington, Vt, Department of Psychiatry, University of Vermont, 1983Google Scholar
7. Rishel CW, Greeno CG, Marcus SC, et al: Use of the Child Behavior Checklist as a diagnostic screening tool in community mental health. Research on Social Work Practice 15:195-203, 2005Google Scholar
8. Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 282:1737-1744, 1999Google Scholar
9. Bickman L, Andrade AR, Lambert EW: Dose response in child and adolescent mental health services. Mental Health Services Research 4:57-69, 2002Google Scholar
10. Anderson CM, Robins C, Greeno CG, et al: Why low-income mothers do not engage with the formal mental health care system: a qualitative study of perceptual barriers to care. Qualitative Health Research, in pressGoogle Scholar
11. Lieb R, Isensee B, Hofler M, et al: Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Archives of General Psychiatry 59:365-374, 2002Google Scholar
12. Weissman MM, Warner V, Wickramaratne P, et al: Offspring of depressed parents: 10 years later. Archives of General Psychiatry 54:932-940, 1997Google Scholar
13. Minuchin S: Families and Family Therapy. Cambridge, Mass, Harvard University Press, 1974Google Scholar
14. Minuchin S, Montalvo B, Guerney B, et al: Families of the Slums. New York, Basic Books, 1967Google Scholar
15. Szapocznik J, Williams RA: Brief strategic family therapy: twenty-five years of interplay among theory, research, and practice in adolescent behavior problems and drug abuse. Clinical Child and Family Psychology Review 3:117-134, 2000Google Scholar



