Mortality and Medical Comorbidity Among Patients With Serious Mental Illness
Numerous studies have documented the impact of excess mortality among patients with serious mental illness. In 1985 Black and associates ( 1 ) found that death rates were higher than expected among psychiatric patients, primarily as a result of suicides and accidents. After extensively reviewing the literature a decade later, Felker and colleagues ( 2 ) found that standardized mortality ratios for both natural and unnatural causes of death among psychiatric patients were more than twice those of the general population. This literature review covered 20 studies and more than 8,000 psychiatric patients and concluded that 50 percent of psychiatric patients had known medical comorbidities, 35 percent harbored undiagnosed medical disorders, and an additional 20 percent had medical problems that may actually have caused or exasperated their psychiatric condition ( 2 ).
Dembling and associates ( 3 ) found that adult patients served by the Massachusetts Department of Mental Health (MDMH) between 1985 and 1994 had a significantly higher frequency of deaths from accidental and intentional injuries. Reduced life expectancies across all disease and injury conditions within this population were also noted. The average years of potential life lost (YPLL) was 8.8 years higher for MDMH decedents compared with decedents in the general population ( 3 ). An unpublished 2001 MDMH mortality report by Sudders (Commonwealth of Massachusetts Executive Office of Health and Human Services Department of Mental Health, unpublished data, May 2001) found that age-specific mortality from cardiovascular disease for individuals aged 25 to 44 years was more than six times as high among MDMH clients as in the general Massachusetts population.
In one of the few studies to consider a cohort of patients with serious mental illness served in a community setting, Berren and associates ( 4 ) reported an overall standardized mortality ratio of 2.4, compared with the general population. Dickey and colleagues ( 5 ) found that for males and females combined the standardized mortality ratio for unnatural causes of death (4.4) was greater than that for natural causes (1.7); however, the highest cause-specific standardized mortality ratios were from HIV (6.1), suicides (5.8), and cerebrovascular disease (4.4). Furthermore, this study documented that Medicaid beneficiaries treated for serious mental illness experienced a significantly higher age- and gender-adjusted risk of having one of eight medical disorders compared with a similar group of Medicaid patients without serious mental illness ( 5 ).
Recently, there has been a renewed interest in better managing the complex relationships that exist between mental and physical illness. This is exemplified by the first goal stated in the report of the President's New Freedom Commission on Mental Health, Achieving the Promise: Transforming Mental Health Care in America: "Americans understand that mental health is essential to overall health" ( 6 ). An internal Ohio Department of Mental Health (ODMH) mortality and morbidity review in 2004 by the Medical Director's Office (Ohio Department of Mental Health, unpublished data, 2004) that examined deaths from 1998 to 2003 during hospitalization or within 30 days postdischarge found that heart disease was the leading cause of death. As a result of these findings, the ODMH required that Ohio's public mental health hospitals review and implement, where appropriate, tools for reducing heart disease developed by the American Heart Association. In November 2004 the Medical Directors Council of the National Association of State Mental Health Program Directors released a technical report that emphasized the need to develop a system of care that bridges existing gaps between the mental and general health communities ( 7 ).
In order to gain an improved understanding and awareness of mortality and medical comorbidity among patients in Ohio with serious mental illness, the purpose of this retrospective record linkage study was to investigate the leading causes of death and medical comorbidity, YPLL, and standardized mortality ratios for patients experiencing at least one inpatient hospitalization in Ohio's public mental health system between 1998 and 2002.
Methods
Data sources and records linkage
This study defined patients with serious mental illness as individuals requiring at least one inpatient psychiatric hospitalization within Ohio's public mental health system. By utilizing the ODMH Patient Care System (PCS) database, data were obtained retrospectively in July 2004 from 31,681 records of adult inpatient admissions between 1998 and 2002. These records consisted of 30,477 admissions during the five-year study period plus an additional 1,204 patients admitted before 1998 who were still hospitalized as of January 1, 1998. Because of multiple admissions, the 31,681 records corresponded to 20,020 unduplicated patients. Two patients were not included in the sample—one with unknown gender and one with unknown date of birth. For patients with multiple admissions, the earliest admission was used for all subsequent date-dependent calculations.
Death records from the Ohio Department of Health (ODH) were then obtained for the same years. Patients from ODMH and ODH files were matched on the basis of name and date of birth, followed by manual inspection of the results to eliminate false positives. This identified 608 ODMH patients who died during the study period. Hospital deaths were included in this total.
Access to ODMH patient records was authorized by the department's medical director for matching purposes only. All personal identifying data were removed from the resulting analytic files. Institutional review board approval was sought through the Ohio Department of Health, and the study was granted exempt status.
Period at risk
Because patients were admitted over varying timelines between 1998 and 2002, the length of time that they were in our sample, and thus, the length of time that their death records would have been searched for, was unequal and the observations were right censored. This was addressed by defining the ODMH population for each year of the study to account for both new patient admissions and deaths. The 1998 ODMH population consisted of 4,392 admissions in 1998, plus an additional 1,204 patients admitted before 1998 who were still hospitalized as of January 1, 1998. The 1999 ODMH population consisted of the 5,596 patients in the 1998 population, plus 3,864 patients admitted in 1999, minus the 37 deaths in 1998. The 2000, 2001, and 2002 ODMH populations were determined similarly. Thus the size of the ODMH population increased annually, as patients were at risk of death from the time of admission until the end of the study period.
Data on leading causes of mortality in the United States for each year of the study were obtained from annual mortality reports from the National Center for Health Statistics (NCHS) ( 8 , 9 , 10 , 11 , 12 ).
Cause of death and ICD coding
For the 608 ODMH decedents, all mortality calculations were based on the underlying cause of death—that is, the condition determined to have initiated the sequence of morbid events culminating in death—as documented in ODH records. In 1999 the ODH changed coding from ICD-9 to ICD-10 . In order to address this change, comparable category codes between ICD-9 and ICD-10 were used as presented in a 1999 NCHS mortality report ( 9 ). This facilitated the inclusion of data from 1998 with the other years of the study.
Life expectancy
YPLL is a measure of premature mortality based on the current mean survival age for a living cohort by age and by gender ( 3 ). YPLL was determined for each ODMH decedent on the basis of U.S. life expectancy in the year of death ( 8 , 9 , 10 , 11 , 12 ). Because life expectancies were given by five-year age groups, these values were linearly interpolated within age groups to estimate life expectancy for each year of age. For all years of the study combined, the mean YPLL was calculated for leading causes as well as all causes of death.
Standardized mortality ratios
Standardized mortality ratios measure the degree to which observed mortality differs from expected mortality in a cohort based on a standard reference population. The U.S. general population from 1998 to 2002 was used as the standard reference population in this study. Specifically, the expected number of ODMH deaths from a given cause was calculated by using age-specific U.S. mortality rates from NCHS annual mortality reports ( 8 , 9 , 10 , 11 , 12 ). For each cause of death, a weighted average of annual standardized mortality ratios was then taken to calculate aggregated standardized mortality ratios for all years of the study combined.
Medical comorbidity
Information on the medical comorbidities of the 608 ODMH decedents was directly obtained from axis III diagnoses in the PCS database. Height and weight data, also available in the PCS database, were used to calculate body mass indices (BMIs).
Statistical analysis
Ninety-five percent, 99 percent, and 99.9 percent confidence intervals were constructed for all standardized mortality ratios by using a simplified method based on the chi square distribution ( 13 ). For confidence intervals that excluded 1.0, the standardized mortality ratio was considered statistically significant.
Results
Population and patient characteristics
Table 1 shows characteristics of the 608 ODMH decedents. The mean±SD and median ages at death for ODMH decedents were 47.7±15.3 and 46 years, respectively. Among ODMH decedents, the most prevalent axis I diagnoses other than substance use disorders were schizophrenia (134 persons, or 22 percent), schizoaffective disorder (128 persons, or 21 percent), bipolar I disorder (87 persons, or 14 percent), and major depressive disorder (80 persons, or 13 percent). Although having a primary substance use disorder was not a criterion for inpatient admission, these axis I diagnoses were well documented in our patient population ( Table 1 ).
 |
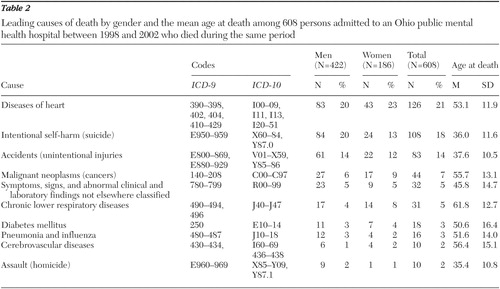
Leading causes of death
As listed in Table 2 , the leading causes of death among the 608 ODMH decedents were heart disease (126 persons, or 21 percent), suicides (108 persons, or 18 percent), accidents (83 persons, or 14 percent), and malignant neoplasms (44 persons, or 7 percent). The top ten causes represented 79 percent (478 cases) of all deaths. Heart disease (43 persons, or 23 percent) and suicides (24 persons, or 13 percent) were the leading causes of death among female ODMH decedents. By contrast, suicides (84 persons, or 20 percent) replaced heart disease (83 persons, or 20 percent) as the leading cause of death among male ODMH decedents. The youngest mean age at death was from homicide (35.4±10.8 years). On average, deaths from unnatural causes (that is, suicides, homicides, and accidents) occurred at earlier ages than deaths from natural causes.
 |
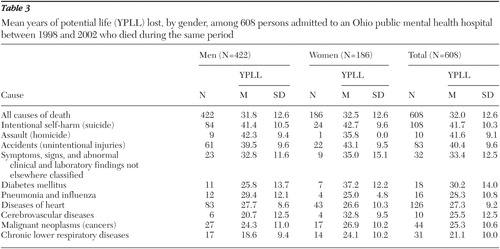
Life expectancy
The mean YPLL for leading causes as well as for all causes of death is shown in Table 3 . The mean YPLL for all causes of death for ODMH decedents was 32.0±12.6 years—31.8±12.6 years for men and 32.5±12.6 years for women. The highest cause-specific mean YPLL was for suicides (41.7±10.3 years). Deaths from unnatural causes had higher mean YPLL than deaths from any other causes. Cause-specific mean YPLL were higher for women than for men, except for homicides, pneumonia and influenza, and heart disease.
 |
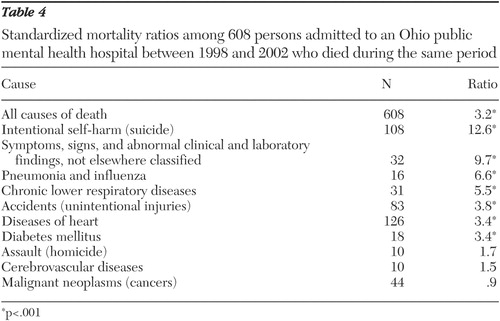
Standardized mortality ratios
Table 4 presents the aggregated standardized mortality ratios for all years of the study combined for leading causes as well as all causes of death. The standardized mortality ratio for all causes of death was 3.2, corresponding to 417 excess deaths (p<.001). The standardized mortality ratio for men (3.2) was equal to that for women (3.2). Suicides had the highest cause-specific standardized mortality ratio (12.6). The only cause-specific standardized mortality ratio less than 1.0 was for malignant neoplasms (.9), indicating fewer than expected cancer deaths among ODMH decedents. Cause-specific standardized mortality ratios were statistically significant (p<.001) for all leading causes except assaults, cerebrovascular diseases, and malignant neoplasms.
 |
Medical comorbidity
For the 608 ODMH decedents, the ODMH PCS database contained axis III diagnoses for 451 (74 percent) and height and weight data for 581 (96 percent). The ten most prevalent medical comorbidities are listed in Table 5 . These included obesity (BMI≥30.0; 144 persons, or 24 percent), hypertension (136 persons, or 22 percent), diabetes mellitus (70 persons, or 12 percent), chronic obstructive pulmonary disease (COPD) (62 persons, or 10 percent), and injuries (39 persons, or 6 percent).
 |
Axis III data were further examined among the 126 ODMH decedents for whom the underlying cause of death was coded as "diseases of heart." Among these patients, leading medical comorbidities were hypertension (46 persons, or 37 percent), obesity (43 persons, or 34 percent), diabetes mellitus (24 persons, or 19 percent), COPD (13 persons, or 10 percent), and disorders of lipid metabolism (11 persons, or 9 percent).
Discussion
Beyond strengthening previously cited mortality statistics, this retrospective record linkage study estimated the prevalence of medical comorbidities and was the first report, to our knowledge, to standardize the classification of causes of death in a decedent population with serious mental illness by using the same ICD codes as mortality reports by the Centers for Disease Control and Prevention. Our findings support the evidence that among patients with serious mental illness, standardized mortality ratios and YPLL are substantially increased for both males and females. Our study also substantiated earlier findings that heart disease, accidents, and suicides were among the leading causes of death in this population. Furthermore, obesity, hypertension, diabetes mellitus, and COPD were the most prevalent medical comorbidities, a finding that is consistent with known risk factors for the observed natural leading causes of death. The prevalence estimates of these conditions are inherently conservative, as there may have been patients for whom axis III data were incompletely recorded.
Many reasons have been postulated as to the etiology of these results. For instance, medication-induced weight gain, poor personal hygiene, reduced physical activity, the increased prevalence of smoking, increased substance use, and inadequate social support systems all are likely to contribute to the development of hypertension, diabetes mellitus, infections, COPD, heart disease, and injuries. Although comorbid substance use—particularly alcohol, marijuana, and cocaine—was well documented ( Table 1 ), notably missing from this list was smoking. Although nicotine dependence is known to be prevalent among patients with serious mental illness, our medical records did not typically include this diagnosis during the years of our study.
Additionally, we observed that a significant number of patients who died did so within relatively short time frames after their last hospitalization. A plurality of patients (211 persons, or 35 percent) died between one and 12 months after discharge, and a majority of the deaths (360 deaths, or 59 percent) were recorded by the end of the second year of community stay. Although the meaning of these data is not clear, they may suggest that hospitalization for serious mental illness is associated with serious physical illnesses. For instance, is this pattern of mortality different for such well-known chronic illnesses as heart failure or COPD?
These issues raise the question of how stakeholders might reorganize to ensure better delivery of a more comprehensive array of appropriate and timely services. Ensuring the continuity of care between the mental and physical health communities is essential for reducing excess mortality and mitigating the effect of medical comorbidities. The relationships between these factors are complex and multifaceted. Solutions will consist of combinations and permutations of local, state, and national resources. As discussed by Dickey and colleagues ( 5 ), the long-standing separation of treatment for medical and mental illnesses may need to be reconsidered. A 2004 Bazelon report examined model programs for improving integration and coordination of behavioral and primary health services ( 14 ). This report states, "physical health care is as central to an individual's service plan as housing, job training, or education." Our study underscores the need for further collaboration among all stakeholders to develop targeted interventions for this population that improve quality-of-life outcomes. Such interventions might include implementing guidelines for reducing heart disease, smoking cessation programs, and pneumonia and influenza vaccination programs.
A current concern, which was not a focus of our study but was consistent with our findings, is the metabolic side effects of second-generation antipsychotic medications. A 2004 Consensus Statement by the American Diabetes Association, the American Psychiatric Association, and others concerning second-generation antipsychotic use and obesity, diabetes, and high cholesterol prompted guidance to physicians to carefully screen and monitor patients taking these medications ( 15 ). Recent mortality warnings from the Food and Drug Administration on the off-label use of second-generation antipsychotics also heightens concern and supports the need for further study of medication-induced side effects.
Although data for a large number of patients in a state hospital were analyzed and matched against more than 500,000 ODH death records, care must be taken in trying to extend these results to a larger population with serious mental illness. Although differences in age and gender were taken into consideration, there are many other factors—axis I diagnoses, medication history, and health and socioeconomic and demographic characteristics—that are difficult to adequately and accurately control for. Our population was largely male, white, and unmarried. In addition, deaths occurring outside of Ohio would not have been tabulated. Errors in death certificate coding and patient matching likewise are difficult to properly quantify.
Conclusions
Observed deaths in our patient population were more than three times as high as expected, compared with the U.S. general population. The mean age at death for ODMH decedents was 47.7±15.3 years, corresponding to an average of 32.0±12.6 years of potential life lost per patient. Heart disease was the leading cause of death. Medical comorbidities were consistent with the known risk factors for the identified natural leading causes of death. Much like the findings of most studies that have examined these issues, our findings showed that serious health care gaps exist for this vulnerable population. The implications of our findings highlight the need to integrate the delivery of currently segmented mental and physical health services. This study underscores a need for improved collaboration between all stakeholders to target interventions that improve quality-of-life outcomes for this population.
Acknowledgment
The authors thank Kelly Miller, M.S., for data analysis assistance.
1. Black DW, Warrack G, Winokur G: The Iowa Record-Linkage Study: I. suicides and accidental deaths among psychiatric patients. Archives of General Psychiatry 42:71-75, 1985Google Scholar
2. Felker B, Yazel JJ, Short D: Mortality and medical comorbidity among psychiatric patients: a review. Psychiatric Services 47:1356-1363, 1996Google Scholar
3. Dembling BP, Chen DT, Vachon L: Life expectancy and causes of death in a population treated for serious mental illness. Psychiatric Services 50:1036-1042, 1999Google Scholar
4. Berren MR, Hill KR, Merikle E, et al: Serious mental illness and mortality rates. Hospital and Community Psychiatry 45:604-605, 1994Google Scholar
5. Dickey B, Normand SLT, Weiss RD, et al: Medical morbidity, mental illness, and substance use disorders. Psychiatric Services 53:861-867, 2002Google Scholar
6. Achieving the Promise: Transforming Mental Health Care in America. Pub no SMA-03-3832. Rockville, Md, Department of Health and Human Services, President's New Freedom Commission on Mental Health, 2003Google Scholar
7. Parks J, Pollack D, Mauer B: Integrating Behavioral Health and Primary Care Services: Opportunities and Challenges for State Mental Health Authorities. Alexandria, Va, National Association of State Mental Health Program Directors, 2004Google Scholar
8. Murphy SL: Deaths: Final Data for 1998. National Vital Statistics Reports: Vol 48, No 11. Hyattsville, Md, National Center for Health Statistics, 2000Google Scholar
9. Hoyer DL, Arias E, Smith BL, et al: Deaths: Final Data for 1999. National Vital Statistics Reports: Vol 49, No 8. Hyattsville, Md, National Center for Health Statistics, 2001Google Scholar
10. Miniño A, Arias E, Kochanek KD, et al: Deaths: Final Data for 2000. National Vital Statistics Reports: Vol 50, No 15. Hyattsville, Md, National Center for Health Statistics, 2002Google Scholar
11. Arias E, Anderson RN, Hsiang-Ching K, et al: Deaths: Final Data for 2001. National Vital Statistics Reports: Vol 52, No 3. Hyattsville, Md, National Center for Health Statistics, 2003Google Scholar
12. Kochanek KD, Murphy SL, Anderson RN, et al: Deaths: Final Data for 2002. National Vital Statistics Reports: Vol 53, No 5. Hyattsville, Md, National Center for Health Statistics, 2004Google Scholar
13. Ulm K: A simple method to calculate the confidence interval of a standardized mortality ratio. American Journal of Epidemiology 131:373-375, 1990Google Scholar
14. Koyanagi C: Get It Together: How to Integrate Physical and Mental Health Care for People With Serious Mental Disorders. Washington, DC, Bazelon Center for Mental Health Law, 2004Google Scholar
15. Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care 27:596-601, 2004Google Scholar



