Awareness of Illness and Nonadherence to Antipsychotic Medications Among Persons With Schizophrenia
Abstract
OBJECTIVE: The purpose of this study was to assess the effects of patients' awareness of their illness on the clinical presentation, management, and course of nonadherence to antipsychotic medications among patients with schizophrenia. METHODS: A national survey was conducted of psychiatrists who were treating patients with schizophrenia. The survey was sent to 771 psychiatrists, of whom 534 responded, for a response rate of 69 percent. The psychiatrists were asked to report on presentation, management, and course for one adult patient with schizophrenia who had been under their care for at least one year and who had been nonadherent to oral antipsychotics at some point in the past year. Patients who were aware that they had a mental illness were compared with those who were not aware. RESULTS: Of the 534 respondent psychiatrists, 310 reported on an eligible patient, and 300 of these patients were classified by illness awareness. Ninety-seven patients, or 32 percent, were not aware that they had a mental illness. These patients who lacked awareness had significantly longer episodes of antipsychotic nonadherence, were more likely to completely cease taking the antipsychotic medication, were more likely to have severe positive symptoms, and were more likely to be psychiatrically hospitalized after nonadherence than those who were aware of their illness. Psychological interventions and several types of family interventions were significantly less effective among patients who lacked awareness. CONCLUSIONS: A lack of awareness of mental illness is common among patients with schizophrenia who are nonadherent to antipsychotics. Such nonadherence tends to be especially disruptive and unresponsive to simple commonly used psychological interventions.
Nonadherence to antipsychotic medication regimens is a grave and pervasive problem in the clinical management of schizophrenia. Compared with patients who are adherent, patients who are not adherent have a greater risk of symptom exacerbation (1), psychiatric hospitalization (2), housing instability (3,4), and violence (5).
Lack of insight or awareness of having a mental illness is commonly cited as a primary reason for nonadherence to antipsychotic medications (6,7). Psychotic patients who lack such insight are at significantly increased risk of nonadherence and hospitalization (8,9,10,11,12). In addition, a perception of invulnerability to rehospitalization (13,14) and a belief that antipsychotic medications do not prevent relapse (15,16) have been associated with nonadherence to medications.
Limited progress has been made in developing effective interventions to manage insight deficits and nonadherence among psychotic patients. In one controlled trial, a brief cognitive-behavioral intervention was associated with significantly improved insight into illness and reduced symptom severity compared with usual care for patients with schizophrenia (17). A type of cognitive-behavioral therapy that focused specifically on improving antipsychotic adherence also proved to be effective (18) and durable (19) in a mixed sample of psychotic patients. However, a replication of the study in a sample that was limited to patients with schizophrenia did not show a significant improvement in adherence (20). Psychoeducational interventions for schizophrenia have tended to demonstrate little effect on insight (21) or adherence (22).
Little is known about the routine psychiatric management of nonadherence to antipsychotic medications among patients with schizophrenia who lack awareness of their illness. Information is sparse regarding how psychiatrists manage these patients and whether and to what extent commonly provided clinical interventions improve adherence among patients who lack insight into their illness. By examining the effects of patients' insight into their illness on the clinical presentation and management of nonadherence as well as the treatment response among patients with schizophrenia, we hope to inform efforts to improve the clinical management of nonadherence to antipsychotics among patients who are not aware that they have a mental illness.
Methods
A nationally representative sample of psychiatrists was surveyed by mail to assess their management of patients with schizophrenia who had been nonadherent to antipsychotic medication regimens. The study was approved by the institutional review boards of New York State Psychiatric Institute and the American Psychiatric Institute for Research and Education. Primary data collection was conducted from September 2003 to January 2004.
A random sample of psychiatrists was selected from the American Medical Association's Masterfile of Physicians. Psychiatrists who were in psychiatric residency training, living outside the United States, over the age of 75 years, and not involved in direct patient care were excluded. Selected psychiatrists (N=1,150) were sent a prescreening postcard to determine whether they had treated at least four patients with schizophrenia in the past typical work month. Analysis of the National Survey of Psychiatric Practice (23,24) indicated that more than 90 percent of patients with schizophrenia who were receiving psychiatric care were being treated by psychiatrists who treated four or more patients with schizophrenia per month.
When the psychiatrists who reported treating fewer than four patients with schizophrenia per month were excluded, the sample was reduced from 1,150 to 880. An additional ten psychiatrists were excluded from the sample because the screening postcards were returned with "addressee unknown" indicated and a follow-up telephone inquiry revealed no forwarding contact information. These exclusions resulted in a final sample of 771 psychiatrists who met eligibility criteria and had a serviceable mailing address.
In this sample, 534 psychiatrists responded to the survey, for a response rate of 69 percent. Of these 534 psychiatrists, 310 reported on an eligible patient who met the study criteria of being older than 18 years; being under the psychiatrist's care for at least one year; being nonadherent to oral antipsychotics at some point in the past year, defined as taking less than half of the prescribed medication for at least two consecutive weeks; not receiving an injection of depot antipsychotic medication during the two months before nonadherence to oral antipsychotics; and being the last patient the psychiatrist saw who had these characteristics. The other participating psychiatrists (N=224) provided general information about their management of medication nonadherence among patients with schizophrenia, but not individual patient-level information. This information was not analyzed for this study.
Psychiatrists were asked, in characterizing the selected patients, to determine whether the patient generally believed he or she had a mental illness. This item was used to define the two study groups: patients who were aware that they had a mental illness and those who were not. Data were missing for ten patients for this variable.
Psychiatrists' assessments of patients who were and were not aware of their illness were compared in terms of basic sociodemographic and clinical characteristics, including selected lifetime mental disorders and prescribed psychotropic medications. The study groups were also compared in terms of the perceived primary cause of the patient's last episode of medication nonadherence: denial of illness, paranoia, grandiosity, cognitive disorganization (difficulty following a medication regimen), motivation deficits (indifference, apathy), intolerable side effects, nonresponse of symptoms to medications, patient's belief that his or her symptoms did not respond to medications, stigma associated with taking medications, lack of family support for medications, lack of support in the patient's living environment for medications, substance use problems, problems with the therapeutic alliance, and cost of medications.
The groups were compared on the frequency and perceived effectiveness of several pharmacologic, psychological, behavioral, and family interventions that were used to manage the most recent episode of nonadherence. For these items, the psychiatrists were asked to indicate whether they used each intervention, and, among those they used, to assess the effectiveness of each on a 5-point scale from 1, ineffective in maintaining adherence, to 5, extremely effective.
Bivariate statistical comparisons were based on chi square tests for categorical variables and t tests for continuous variables. Multiple linear regression analyses examined associations between insight into illness and perceived effectiveness of the intervention, with potentially confounding sociodemographic and clinical patient characteristics controlled for. All analyses included weighting to account for nonresponse.
Results
Sociodemographic and clinical characteristics
Approximately one-third of the nonadherent patients (97 patients, or 32 percent) were reported by their psychiatrists as being unaware that they had a mental illness. Compared with the patients who were aware of their mental illness, patients who lacked awareness were significantly less likely to be working at either paid or volunteer employment (Table 1). Both patient groups were predominantly white males who were not married or employed.
Patients who were reported to be aware of having a mental illness were significantly more likely than those without such an awareness to have a lifetime history of major depression, to have a substance use disorder, and to have been homeless for at least 48 hours. By contrast, awareness of illness was not significantly related to deficits in intellectual functioning, having made a previous suicide attempt, or having intentionally physically injured someone. Immediately before the index nonadherence episode, the vast majority of both groups were managed with second-generation antipsychotic medications. Some patients in each group received adjunctive mood stabilizers, antidepressants, or anxiolytic medications.
Nonadherence episodes
The psychiatrists were asked to select, from a list of 15 possible responses, the primary factor that they believed was most important in the development of the patient's last episode of nonadherence. Denial of illness was cited for nearly three-quarters of the patients who lacked an awareness of their illness (70 patients, or 72 percent). By contrast, denial of illness was cited as the primary factor for 35 of the patients who were aware of having a mental illness (18 percent) (Table 2). Interestingly, stigma associated with taking an antipsychotic medication was not cited as the primary contributing factor for any of the patients who lacked awareness of having a mental illness.
Episodes of nonadherence tended to be more severe among patients who were assessed as being unaware of having a mental disorder than among patients who were assessed as being aware. Specifically, episodes of nonadherence among patients who were unaware of their illness were significantly longer, more commonly involved complete cessation of medication, and more often resulted in a psychiatric hospitalization. However, complete cessation of medication was common in both groups. Compared with patients who were aware of having a mental illness, patients who lacked such awareness had significantly more severe positive symptoms immediately before, during, and after the nonadherence episode and significantly more severe negative symptoms after the episode (Table 2).
Management of medication nonadherence
There was little evidence that management of nonadherence with antipsychotic medications varied across the two patient groups. The vast majority of both groups were urged by their psychiatrists to take their antipsychotic medications. In addition, psychiatrists commonly discussed the risks of medication nonadherence, main effects and side effects of the medications, the patients' reasons for nonadherence, and what taking medications meant to the patients' identity. Efforts were made to connect medication adherence to patients' personal goals. A substantially smaller proportion of patients in each group received family, behavioral, or pharmacologic interventions aimed at managing their nonadherence. In both groups, simplifying the dosage regimen was the most common pharmacologic intervention (Table 3).
Perceived effectiveness of interventions
All the psychological interventions studied were reported by the treating psychiatrists to be significantly less effective among patients who lacked awareness of having a mental illness than among patients who were aware (Table 4). These group differences remained significant after group differences in background sociodemographic and clinical characteristics were controlled.
Several, but not all, of the behavioral and family interventions were also reported to be significantly less effective among patients who were unaware of their mental illness than they were among patients who were aware. The effectiveness of teaching family members to use positive reinforcement and cueing pill taking to reminders, such as an alarm clock, did not significantly differ in perceived effectiveness between the study groups, although each approach tended to be more effective among patients who were aware that they had a mental illness (Table 4).
The perceived effectiveness of the pharmacologic interventions, with the exception of simplifying the dosage regimen, did not significantly differ between the two study groups in the adjusted models. In both groups, the most effective intervention was reported to be the initiation of a depot antipsychotic medication.
Discussion
Our findings, in line with previous research (6,8,9), indicate that patients with schizophrenia who are not adherent to antipsychotic medication regimens commonly lack an awareness of having a mental disorder. We estimate that approximately one-third of psychiatric outpatients with schizophrenia in the United States who are nonadherent are not aware that they have a mental illness.
In this study, awareness of illness was related to a history of comorbid depression. A recent meta-analysis also indicated a positive relationship between insight and depressive symptoms (25). More severe depression has been strongly associated with greater insight early in the course of illness (26) and among patients with multiple episodes (27,28,29). In one study, insight into illness was related to suicidal ideation (30). As clinical efforts are made to extend and broaden insight into illness among persons with schizophrenia, it may be important to monitor patients closely for changes in mood state and suicidal behavior (17).
Patients who were aware of having a mental illness were approximately twice as likely to be engaged in paid or volunteer employment as patients who lacked such awareness. This finding is consistent with previous research linking impairments in insight and occupational performance (31,32). In one study of adults with schizophrenia, those with poor insight into their illness had greater difficulties cooperating with coworkers, poorer work habits, and poorer quality of work than their counterparts whose insight was intact (32). Improvements in vocational rehabilitation have also been related to improved insight (33).
In this study, a history of substance abuse and homelessness was related to an awareness of illness. Longitudinal research is needed to help define the extent to which awareness of schizophrenia increases vulnerability to substance abuse or housing loss, or whether these adversities tend to lead to a greater awareness of having a mental disorder among individuals with schizophrenia.
Several investigators have reported that cognitive impairment in schizophrenia is related to deficits in insight (32,34,35,36). In our study, which involved comparisons among patients who had recently been nonadherent to medications, awareness of mental illness was not significantly related to general intellectual functioning. Because nonadherence is also significantly related to poor intellectual functioning (36), it is possible that, because the samples were limited to patients who were nonadherent, group differences in intellectual functioning were attenuated.
Denial of illness was cited as the primary cause of nonadherence for a majority of patients who lacked awareness of their illness. By contrast, paranoia was less commonly related to nonadherence among patients who lacked awareness than among those who were aware of having a mental illness. This finding, together with the lower rates of depressive disorder in the group that lacked insight, is consistent with research linking the evolution of insight to development of depression and paranoia in early-stage schizophrenia (37).
The consequences of nonadherence to antipsychotic medications may be especially serious for patients who lack awareness of having a mental disorder. Compared with patients with intact insight, patients with impaired insight have a significantly longer duration of nonadherence, are more likely to completely cease taking antipsychotic medications, have more severe positive psychotic symptoms, and are more likely to be psychiatrically hospitalized.
In routine psychiatric practice, management of nonadherence to antipsychotic medications does not appear to vary markedly with awareness of illness. No significant differences were found by illness awareness in the frequency with which patients received a wide range of pharmacologic, psychological, behavioral, and family interventions. Simple psychological interventions, such as urging the patient to maintain medication adherence or discussing the risks of nonadherence, were almost universally provided to both patient groups.
In clinical treatment research, cognitive-behavioral and motivational approaches have shown some promise in building insight (17) and improving adherence (18,19) among persons with psychotic disorders. By contrast, the common—and presumably much less intensive—psychological interventions we assessed in routine practice were perceived as relatively ineffective in managing antipsychotic nonadherence, especially among patients who lacked awareness of having a mental disorder. Differences between patient groups in perceived effectiveness tended to be less evident for several of the pharmacologic interventions.
For both patient groups, starting a depot medication (38) and observing pill taking on a daily basis were rated as the two most effective interventions. Expanding the use of these interventions might improve the management of nonadherence. At the same time, more work is needed to develop and test intensive psychological approaches to the prevention and management of nonadherence to antipsychotic medications among patients with schizophrenia.
This study had several limitations. First, the data are based exclusively on the psychiatrists' assessments. Although we limited the study to patients who had been under the psychiatrists' care for at least a year and who therefore were presumably well known to the psychiatrists, the absence of patient-reported or family-reported data imposes significant and obvious limitations. For example, patients may have a different view than their psychiatrist of the effectiveness of treatment. In addition, the exclusion of patients who were seen for less than a year is likely to have eliminated many highly nonadherent patients.
Second, the accuracy of clinicians' assessments of adherence to antipsychotic regimens has been questioned (39,40). Although a more intrusive method of adherence measurement, such as pill counts, serum levels, and electronic MEMS (Medication Event Monitoring System) caps, would likely have yielded more accurate information, the promise of improved accuracy of measurement must be weighed against substantial selection biases that are likely to have been introduced by limiting the sample to patients who were willing to submit to intrusive adherence monitoring.
Third, illness awareness was measured with a single survey item. A more extensive assessment of insight into illness (41,42,43) would have provided a more informative description. For some patients, illness awareness may fluctuate and cannot be captured by a dichotomous measure.
Fourth, salience of individual cases may have biased patient selection and produced a sample of memorable patients rather than representative patients (44). Fifth, no information was collected for patients who consistently adhered to their antipsychotic therapy. For this reason, the results do not address patients who, despite reporting that they were not ill, came to appointments and took their antipsychotic medications as prescribed. Finally, survey nonresponse may have biased the reported rates and group associations. Although we adjusted the results for nonresponse related to known characteristics of the study psychiatrists, we cannot exclude the possibility that response patterns related to unmeasured respondent characteristics biased study findings.
Conclusions
Lack of insight into mental illness is common among patients with schizophrenia who are nonadherent to antipsychotic medication regimens. For patients with schizophrenia who lack such awareness, nonadherence tends to be prolonged and especially clinically disruptive. Simple psychological approaches were often used to manage medication nonadherence in this patient sample but were reported by the treating psychiatrists as being relatively ineffective. By contrast, initiation of depot medications, daily observation of medications, and family psychoeducation were less commonly used but were reported to be more effective than the psychological interventions. Developing and testing new strategies to enhance adherence to antipsychotics among patients with schizophrenia who lack insight into their illness remains a high priority.
Acknowledgment
This research was supported by grant MH-061539 to Dr. Olfson from the National Institutes of Health.
Dr. Olfson is affiliated with the department of psychiatry of Columbia University and with New York State Psychiatric Institute, 1051 Riverside Drive, New York, New York 10032 (e-mail, [email protected]). Dr. Marcus is with the department of social work of the University of Pennsylvania in Philadelphia. Dr. Wilk and Dr. West are with the American Psychiatric Institute for Research and Education in Arlington, Virginia.
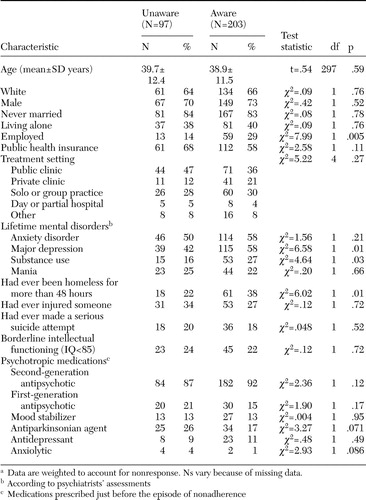 |
Table 1. Background sociodemographic and clinical characteristics of patients with schizophrenia who were nonadherent to antipsychotic medications, by whether their psychiatrist reported them as being aware of their mental illnessa
a Data are weighted to account for nonresponse. Ns vary because of missing data.
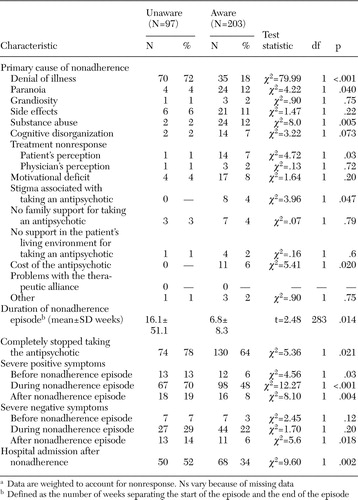 |
Table 2. Characteristics of episodes of nonadherence to antipsychotic medications among patients with schizophrenia who were aware of their mental illness and those who were not awarea
a Data are weighted to account for nonresponse. Ns vary because of missing data
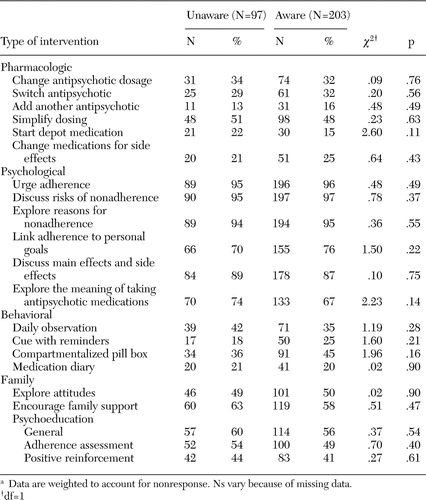 |
Table 3. Frequency of interventions used to manage episodes of nonadherence among patients with schizophrenia, by whether their psychiatrist reported them as being aware of their mental illnessa
a Data are weighted to account for nonresponse. Ns vary because of missing data.
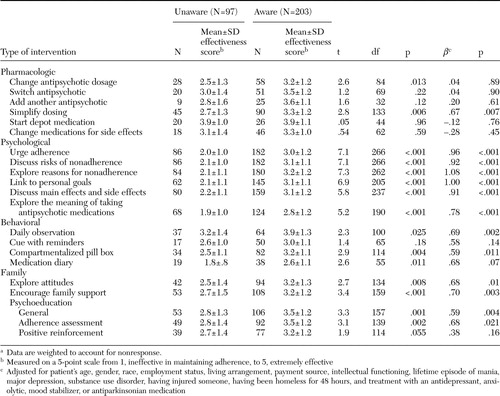 |
Table 4. Perceived effectiveness of interventions to manage episodes of nonadherence to antipsychotic medications among patients with schizophrenia, by whether their psychiatrist reported them as being aware of their mental illnessa
a Data are weighted to account for nonresponse.
1. Robinson D, Woerner MG, Alvir JM, et al: Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Archives of General Psychiatry 56:241–247,1999Crossref, Medline, Google Scholar
2. Svarstad BL, Shireman TI, Sweeney JK: Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatric Services 52:805–811,2001Link, Google Scholar
3. Drake RE, Wallach MA, Teague GB, et al: Housing instability and homelessness among rural schizophrenic patients. American Journal of Psychiatry 148:330–336,1991Link, Google Scholar
4. Opler LA, Caton CL, Shrout P, et al: Symptom profiles and homelessness in schizophrenia. Journal of Nervous and Mental Disease 182:174–178,1994Crossref, Medline, Google Scholar
5. Swanson JW, Swartz MS, Borm R, et al: Involuntary out-patient commitment and reduction of violent behavior in persons with severe mental illness. British Journal of Psychiatry 176:324–331,2000Crossref, Medline, Google Scholar
6. Loffler W, Kilian R, Touni M, et al: Schizophrenic patients' subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry 36:105–112,2003Crossref, Medline, Google Scholar
7. Smith TE, Hull JW, Goodman M, et al: The relative influences of symptoms, insight, and neurocognition on social adjustment in schizophrenia and schizoaffective disorder. Journal of Nervous and Mental Disease 187:102–108,1999Crossref, Medline, Google Scholar
8. Rittmannsberger H, Pachinger T, Keppelmuller P, et al: Medication adherence among psychotic patients before admission to inpatient treatment. Psychiatric Services 55:174–179,2004Link, Google Scholar
9. Olfson M, Mechanic D, Hansell S, et al: Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiatric Services 51:216–222,2000Link, Google Scholar
10. Cuffel BJ, Alford J, Fischer EP, et al: Awareness of illness in schizophrenia and outpatient treatment adherence. Journal of Nervous and Mental Disease 184:653–659,1996Crossref, Medline, Google Scholar
11. MacPhearson R, Jerome B, Hughes A: Relationship between insight, educational background, and cognition in schizophrenia. British Journal of Psychiatry 168:718–722,1996Crossref, Medline, Google Scholar
12. Bartko G, Herczeg I, Zaador G: Clinical symptomatology and drug compliance in schizophrenic patients. Acta Psychiatrica Scandinavica 77:74–76,1988Crossref, Medline, Google Scholar
13. Adams J, Scott J: Predicting medication adherence in severe mental disorders. Acta Psychiatrica Scandinavica 101:119–124,2000Crossref, Medline, Google Scholar
14. Kelly GR, Scott JE: Medication compliance and health education among outpatients with chronic mental disorders. Medical Care 28:1181–1197,1990Crossref, Medline, Google Scholar
15. Hogan TP, Awad AG, Eastwood R: A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychological Medicine 13:177–183,1983Crossref, Medline, Google Scholar
16. Amador XF, Strauss DH: Poor insight in schizophrenia. Psychiatric Quarterly 64:305–318,1993Crossref, Medline, Google Scholar
17. Turkington D, Kingdon D, Turner T: Insight Into Schizophrenia Research Group: effectiveness of a brief cognitive-behavioral therapy intervention in the treatment of schizophrenia. British Journal of Psychiatry 180:523–527,2002Crossref, Medline, Google Scholar
18. Kemp R, Hayward P, Applewhaite G, et al: Compliance therapy in psychotic patients: randomised controlled trial. British Medical Journal 372:345–349,1996Crossref, Google Scholar
19. Kemp R, Kirov G, Everitt B, et al: Randomized controlled trial of compliance therapy:18–month follow-up. British Journal of Psychiatry 172:413-419,1998Google Scholar
20. O'Donnell C, Donohoe G, Sharkey L, et al: Compliance therapy: a randomised controlled trial in schizophrenia. British Medical Journal 327:834,2003Crossref, Medline, Google Scholar
21. Pekkala E, Merinder L: Psychoeducation for schizophrenia. Cochrane Database of Systematic Reviews 2:CD002931, 2002Google Scholar
22. Zygmunt A, Olfson M, Boyer CA, et al: Interventions to improve medication adherence in schizophrenia. American Journal of Psychiatry 159:1653–1664,2002Link, Google Scholar
23. Scully JH, Wilk JE: Selected characteristics and data of psychiatrists in the United States, 2001-2002. Academic Psychiatry 27:2476–2251,2003Crossref, Google Scholar
24. Zarin DA, Pincus HA, Peterson BD, et al: Characterizing psychiatry with findings from the 1996 National Survey of Psychiatric Practice. American Journal of Psychiatry 155:397–404,1998Link, Google Scholar
25. Mintz AR, Dobson KS, Romney DM: Insight in schizophrenia: a meta-analysis. Schizophrenia Research 61:75–88,2003Crossref, Medline, Google Scholar
26. Drake RJ, Pickles A, Bentall RP, et al: The evolution of insight, paranoia, and depression during early schizophrenia. Psychological Medicine 34:285–292,2004Crossref, Medline, Google Scholar
27. Smith TE, Hull JW, Israel LM: Insight, symptoms, and neurocognition in schizophrenia. Schizophrenia Bulletin 26:193–200,2000Crossref, Medline, Google Scholar
28. Moore O, Cassidy E, Carr A, et al: Unawareness of illness and its relationship with depression and self-deception in schizophrenia. European Journal of Psychiatry 14:264–269,1999Crossref, Google Scholar
29. Carroll A, Fattah S, Clyde Z, et al: Correlations of insight and insight change in schizophrenia. Schizophrenia Research 35:247–253,1999Crossref, Medline, Google Scholar
30. Kim CH, Jayathilake K, Meltzer HY: Hopelessness, neurocognitive function, and insight in schizophrenia: relationship to suicidal behaviour. Schizophrenia Research 60:71–80,2003Crossref, Medline, Google Scholar
31. Lysaker PH, Bell MD, Milstein RM, et al: Insight and psychosocial treatment compliance in schizophrenia. Psychiatry 57:307–315,1994Crossref, Medline, Google Scholar
32. Lysaker PH, Bryson GJ, Bell MD: Insight and work performance in schizophrenia. Journal of Nervous and Mental Disease 190:142–146,2002Crossref, Medline, Google Scholar
33. Lysaker P, Bell M: Work rehabilitation and improvements in insight in schizophrenia. Journal of Nervous and Mental Disease 183:103–106,1995Crossref, Medline, Google Scholar
34. Laroi F, Fannemel M, Ronneberg U, et al: Unawareness of illness in chronic schizophrenia and its relationship to structural brain measures and neuropsychological tests. Psychiatry Research 100:49–58,2000Crossref, Medline, Google Scholar
35. Mohamed S, Fleming S, Penn DL, et al: Insight in schizophrenia: its relationship to measures of executive functions. Journal of Nervous and Mental Disease 187:525–531,1999Crossref, Medline, Google Scholar
36. David A, Buchanan A, Reed A, et al: The assessment of insight in psychosis. British Journal of Psychiatry 161:599–602,1992Crossref, Medline, Google Scholar
37. Drake RJ, Pickles A, Bentall RP, et al: The evolution of insight, paranoia, and depression during early schizophrenia. Psychological Medicine 34:285–292,2004Crossref, Medline, Google Scholar
38. Schooler NR: Relapse and rehospitalization: comparing oral and depot antipsychotics. Journal of Clinical Psychiatry 64:14–17,2003Crossref, Google Scholar
39. Byerly M, Fisher R, Whatley K, et al: A comparison of electronic monitoring vs clinician rating of antipsychotic adherence in outpatients with schizophrenia. Psychiatry Research 133:129–133,2005Crossref, Medline, Google Scholar
40. Cramer JA, Rosenheck R: Enhancing medication compliance for people with serious mental illness. Journal of Nervous and Mental Disease 187:53–55,1999Crossref, Medline, Google Scholar
41. Amador XF, Flaum M, Andreasen NC, et al: Awareness of illness in schizophrenia and schizoaffective and mood disorders. Archives of General Psychiatry 51:826–836,1994Crossref, Medline, Google Scholar
42. McEvoy JP, Freter S, Everett G, et al: Insight and the clinical outcome of schizophrenic patients. Journal of Nervous and Mental Disease 177:48–51,1989Crossref, Medline, Google Scholar
43. Beck AT, Baruch E, Balter JM, et al: A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophrenia Research 68:319–329,2004Crossref, Medline, Google Scholar
44. Westmacott R, Moscovitch M: The contribution of autobiographical significance to semantic memory. Memory and Cognition 31:761–774,2003Crossref, Medline, Google Scholar



