Brief Reports: Use of Psychotropic Medications by Youths With Psychiatric Diagnoses in the U.S. Mental Health System
Abstract
This study estimated the overall rate of use of psychotropic medications among youths (less than 18 years of age) in the U.S. mental health service system and compared rates of use for youths with a single diagnosis and those with co-occurring diagnoses. Results were based on nationally representative client data from the 1997 Client/Patient Sample Survey. On any given day, about one-third (32.5 percent) of the 559,769 youths in the service system received psychotropic medication. Youths with co-occurring diagnoses were significantly more likely to receive medication than youths with a single diagnosis. Future research on best practices may be most effective if the role of medication in the treatment of single and co-occurring disorders among youths is evaluated.
Use of psychotropic medications by youths who have serious emotional disturbances is increasingly common (1,2,3). Our understanding of the scope of psychotropic drug use among children and adolescents in the United States has been informed primarily by data on office-based encounters in the National Ambulatory Medical Care Survey (NAMCS) (4,5) and by records of state Medicaid or regional health maintenance organizations (1,3,6). In general, these studies have estimated the prevalence and correlates of use of psychotropic medications on the basis of a single primary diagnosis. Little is known about patterns of psychotropic use among children who have more than one psychiatric disorder. This gap in information complicates the development of safe and effective pharmacologic regimens.
The purpose of the study reported here was to estimate the use of psychotropic medications among youths (less than 18 years of age) in the U.S. mental health service system and to compare rates between youths with a specific single diagnosis and those with co-occurring diagnoses. Analyses were based on data from the nationally representative 1997 Client/Patient Sample Survey (CPSS). This study complements existing research by including a comprehensive standardized diagnostic inventory that identifies up to two diagnoses and by capturing data on youths receiving care in psychiatric inpatient, outpatient, and residential settings across the nation, regardless of payment source.
Methods
The National Institutes of Health's Center for Mental Health Services (CMHS) conducted the 1997 CPSS to collect information about persons receiving mental health care throughout the nation (7). The study, which oversampled youths, targeted two distinct populations: all persons who were admitted to or discharged from inpatient, outpatient, and residential treatment facilities during 1997 and all persons who were under care in these facilities on May 1, 1997. Service information was collected only for the sample of persons under care.
A two-stage sampling design was used. First, 1,598 facilities were randomly selected from the 1994 Inventory of Mental Health Organizations and General Hospital Mental Health Services, which includes all inpatient, outpatient, and residential care programs in the United States and excludes individual or group office-based practices. Second, administrative staff at each facility, who had been blinded to the purposes of this study, completed data collection forms based on case records for randomly selected clients. The CMHS calculated weights to generate national estimates. The study reported here is based on 3,995 youths under care, representing a weighted estimate of 559,769 youths (6.8 percent aged zero to five years, 50.3 percent aged six to 12 years, and 42.9 percent aged 13 to 17 years). A majority of the youths were male (63.5 percent) and were non-Hispanic white (61.4 percent). Close to one quarter (22.6 percent) of the youths were non-Hispanic black, 13.4 percent were Hispanic, and the rest were Asians, Pacific Islanders, or Native Americans.
The data collection instrument allowed for one psychiatric diagnosis (the "principal" diagnosis) or two diagnoses ("secondary or dual principal" diagnoses) for each client. These diagnoses were entered as DSM-IV, DSM-III-R, DSM-III, or ICD-9-CM diagnostic codes and were collapsed into 12 analytic categories: attention-deficit hyperactivity disorder, conduct disorder, adjustment disorder, mood disorder, anxiety disorder, developmental or pervasive developmental disorder, psychotic disorder, personality disorder, alcohol or other drug use disorder, V codes, other psychiatric diagnosis, and no psychiatric diagnosis or diagnosis deferred. Receipt of psychotropic medication during the "under care" episode was expressed as a dichotomous yes-or-no variable. Frequency and chi square analyses (with PROC CROSSTAB) were conducted on the weighted data with use of SAS-callable SUDAAN to account for the complex survey design (8).
The institutional review board at Rutgers University granted the study exemption status on the grounds that specific individuals were not identifiable in the data set. The survey instrument and detailed diagnostic codes are available on request.
Results
About a third of the youths (32.5 percent) in the mental health service system were treated with psychotropic medication. Rates of medication use were highest in inpatient settings (76.2 percent), followed by residential care settings (59.2 percent) and outpatient settings (29.7 percent) (χ2=63.8, df=2, p<.001). Boys had significantly higher rates of medication use than girls (34.9 percent compared with 28.3 percent; χ2=6.42, df=1, p=.01). Rates of use differed significantly by age (χ2=24.26, df=2, p<.001), primarily because of the comparatively low rate of use among youths under the age of six years (13.3 percent); the youngest recipients of medication were two years old. Estimates of medication use among six- to 12-year-olds and 13- to 17-year-olds were similar (32.8 percent and 35.1 percent, respectively).
As can be seen from Table 1, youths with only one assigned psychiatric diagnosis had a medication use rate of 28.9 percent, whereas those with two diagnoses had a significantly higher rate of 40.4 percent. Nearly 14 percent of the youths with no assigned diagnosis also were treated with medication.
The table also shows rates of medication use for specific principal diagnoses, listed in the order of the frequency of the diagnosis in the service population. Across diagnostic categories, medication use ranged from 15.5 percent (for adjustment disorder) to 65.9 percent (for psychotic disorders). The diagnostic categories were also disaggregated to determine the rate of medication use both when the principal diagnosis was the only diagnosis and when the principal diagnosis was coupled with another diagnosis. An overall pattern of higher medication use was observed among youths with two diagnoses rather than one. Notably, of the youths with a diagnosis of conduct disorder alone, 23.4 percent received medication, compared with 35.4 percent of youths whose diagnostic profile included both conduct disorder and another disorder. The medication use rate for adjustment disorder was twice as high among youths with co-occurring diagnoses (25.5 percent) as among those with a single diagnosis (12.2 percent).
Finally, we estimated medication use among youths who had specific combinations of co-occurring disorders (data not included in the table). Compared with youths who had other diagnostic profiles, youths with anxiety plus attention-deficit hyperactivity disorder were significantly more likely to receive medication (67.4 percent; χ2=10.21, df=1, p<.001), as were those who had both conduct disorder and attention-deficit hyperactivity disorder (57.3 percent; χ2=12.10, df=1, p<.001).
Discussion
These national mental health service data show that about one-third of youths under the age of 18 years received psychotropic medications while they were under care in inpatient, outpatient, or residential settings and that youths with co-occurring psychiatric diagnoses were significantly more likely to receive medications than those with a single diagnosis. Utilization studies based on other target populations have shown lower estimates (for example, 61.6 per 1,000 youths enrolled in three health care plans) (1), whereas other studies have shown higher rates (for example, 75 percent of office visits by five- to 18-year-olds with attention-deficit hyperactivity disorder) (3). Adding to the growing base of knowledge about psychotropic medications, the CPSS data represent half a million youths with private or public insurance in the U.S. mental health service system.
Our findings are consistent with the results of limited previous research that also showed higher medication use rates among clients with a second diagnosis (9). As in our study, other studies have shown a greater use of medications for attention-deficit hyperactivity disorder than for most other diagnoses (6). In addition, other research has shown that a substantial number of youths who do not have a psychiatric diagnosis receive psychotropic medications (4).
Given the increasing use of psychotropic medication among youths (1,2,3), rates of medication use reported in 1997 may be lower than current rates, which is a potential limitation of the study. However, in terms of differences between youths with single and co-occurring diagnoses, the pattern is likely to be the same.
Conclusions
This study used nationally representative client estimates across inpatient, outpatient, and residential care facilities to add to the data on the prevalence of psychotropic medication use among youths in the United States. The study is the first national services study to document differences in use between youths with one diagnosis and those with co-occurring diagnoses. Although the survey did not collect information about the classifications of psychotropic medications prescribed, the results may be useful to researchers and clinicians. A landmark study of treatment for children with attention-deficit hyperactivity disorder demonstrated the importance of attending to co-occurring psychiatric conditions in clinical trials of psychotropic agents (10). Our results strongly suggest that the validity of future clinical trials of psychotropic agents may be strengthened by systematically evaluating outcomes for youths with single and co-occurring diagnoses.
Dr. Warner and Dr. Pottick are affiliated with Rutgers University School of Social Work, 536 George Street, New Brunswick, New Jersey 08901 (e-mail, [email protected]). Dr. Pottick is also with the Institute for Health, Health Care Policy, and Aging Research of Rutgers University. Ms. Mukherjee is a student in the honors program of Rutgers College at Rutgers University.
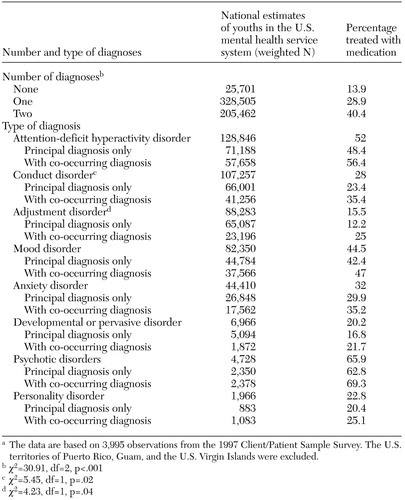 |
Table 1. Proportion of youths treated with psychotropic medication in the U.S. mentalhealth service system, by number and type of diagnoses (principal diagnosis onlyand principal with a co-occurring diagnosis)a
a The data are based on 3,995 observations from the 1997 Client/Patient Sample Survey. The U.S.territories of Puerto Rico, Guam, and the U.S. Virgin Islands were excluded.
1. Zito JM, Safer DJ, dos Reis S, et al: Psychotropic practice patterns for youth. Archives of Pediatrics and Adolescent Medicine 157:17–25, 2003Crossref, Medline, Google Scholar
2. Rushton JL, Whitmire JT: Pediatric stimulant and selective serotonin reuptake inhibitor prescription trends, 1992 to 1998. Archives of Pediatrics and Adolescent Medicine 155:560–565, 2001Crossref, Medline, Google Scholar
3. Robinson LM, Sclar DA, Skaer TL, et al: National trends in the prevalence of attention-deficit/hyperactivity disorder and the prescribing of methylphenidate among school-age children:1990–1995. Clinical Pediatrics 38:209–217, 1999Google Scholar
4. Goodwin R, Gould MS, Blanco C, et al: Prescription of psychotropic medications to youths in office-based practice. Psychiatric Services 52:1081–1087, 2001Link, Google Scholar
5. Jensen PS, Bhatara VS, Vitiello B, et al: Psychoactive medication prescribing practices for U.S. children: gaps between research and clinical practice. Journal of the American Academy of Child and Adolescent Psychiatry 38:557–565, 1999Crossref, Medline, Google Scholar
6. Shireman TI, Olson BM, Dewan NA: Patterns of antidepressant use among children and adolescents. Psychiatric Services 53:1444–1450, 2002Link, Google Scholar
7. Milazzo-Sayre LJ, Henderson MJ, Manderscheid RW, et al: Persons treated in specialty mental health care programs, United States, 1997, in Mental Health, United States, 2000. Edited by Manderscheid, RW, Henderson MJ. DHHS pub no SMA 01–3537. Rockville, Md, Center for Mental Health Services, 2001Google Scholar
8. Shah BV, Barnwell BG, Bieler GS: SUDAAN User's Manual, release 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
9. Rappley M, Eneli IU, Mullan PB, et al: Patterns of psychotropic medication use in very young children with attention-deficit hyperactivity disorder. Journal of Developmental and Behavioral Pediatrics 23:23–30, 2002Crossref, Medline, Google Scholar
10. The MTA Cooperative Group: Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder: the Multimodal Treatment Study of Children With Attention-Deficit/Hyperactivity Disorder. Archives of General Psychiatry 56:1088–1096, 1999Crossref, Medline, Google Scholar



