Criminal History as a Prognostic Indicator in the Treatment of Homeless People With Severe Mental Illness
Abstract
OBJECTIVE: This study examined the clinical problems and treatment outcomes of homeless people with severe mental illness and a history of incarceration. METHODS: Between May 1994 and June 1998, a total of 5,774 people entered assertive community treatment case management services in the Access to Community Care and Effective Services and Supports (ACCESS) demonstration program at 18 sites in nine states. This study used data from reassessments at 12 months after program entry. Analysis of variance was used to compare baseline status and 12-month outcomes for clients with a lifetime incarceration history of less than six months, of six months or more, and no incarceration history. The outcomes assessed were housing status, employment status, psychiatric problems, alcohol problems, drug problems, and criminal justice involvement. RESULTS: Two-thirds of the ACCESS clients had a history of incarceration, with about one-third having less than six months of incarceration and about one-third having six months or more of incarceration. Clients with a long-term incarceration history had higher psychiatric symptom scores, higher drug use and alcohol use scores, and higher levels of dual diagnosis than those with a short-term incarceration history or those with no history of incarceration. The same order of differences was found on measures of childhood abuse, family-of-origin stability, and childhood conduct disorder. Clients with an incarceration history of six months or more reported higher levels of long-term homelessness than the group without an incarceration history. The group with an incarceration history of less than six months showed less improvement at the 12-month follow-up evaluation than the group with no incarceration history on only one outcome measure, psychiatric problems. The group with an incarceration history of six months or more had poorer outcomes than the group with no incarceration history on only two of six outcomes, psychiatric problems and number of days in jail. CONCLUSIONS: This study found that among homeless clients with severe mental illness, clients with a history of incarceration have more serious problems and show somewhat less improvement in some community adjustment domains.
Since the 1990s epidemiologic studies of homeless people have demonstrated that about one-half of people who are sleeping on the streets or in shelters have a history of incarceration (1,2) and that rates of multiple arrests are four times higher for homeless men than for domiciled men (3). Researchers have suggested various explanations for these higher arrest and incarceration rates, ranging from laws that criminalize homeless people (1,4) to criminal activity that long predates adult homelessness (5).
Although mental health advocates are strongly supportive of outreach to homeless people with mental illness, clinicians and administrators are apprehensive about the treatment prospects of former inmates, who are viewed as treatment resistant, dangerous, serious substance abusers, and sociopaths (6,7,8,9,10,11). At present, however, information is limited on the specific types and levels of clinical problems that clients with a history of incarceration have and whether these clients are less responsive to community treatment than clients without a history of incarceration.
To examine these issues, we analyzed baseline and 12-month data from the Center for Mental Health Services' Access to Community Care and Effective Services and Supports (ACCESS) demonstration program to compare homeless clients with severe mental illness, grouped according to their incarceration history. Our hypothesis was based on a recent study of a jail outreach program (12). We expected that ACCESS clients with a history of incarceration would have higher levels of psychiatric, substance abuse, and community adjustment problems at baseline, would use various types of health and social services less frequently, and would have poorer 12-month outcomes than clients who did not have a history of incarceration.
Methods
ACCESS clients and data sources
In 1993 the Center for Mental Health Services initiated the ACCESS demonstration program, a five-year, 18-site, nine-state program designed to test whether the integration of service systems would improve outcomes for homeless persons with severe mental illness (13). The 18 sites provided 12 months of assertive community treatment case management services to four successive cohorts, each with 100 clients who were contacted in a variety of outreach locations (14,15). Clients were eligible for services if they had a severe mental illness and had lived in an emergency shelter, outdoors, or in a public or abandoned building for seven of the previous 14 days (16).
The appropriate institutional review boards approved the study protocol and informed consent procedures. At baseline, clients were evaluated with a comprehensive interview. Clients were reevaluated after three and 12 months to determine outcomes and service use. The study reported here analyzed 12-month data only. Program participants were recruited from May 1994 through June 1998.
Past involvement in the criminal justice system, as measured by reported lifetime incarceration at the baseline interview, was used to divide the sample into three groups: no incarceration history; short-term incarceration history, defined as less than six months of incarceration; and long-term incarceration history, defined as six months or more of incarceration. Categories of incarceration history were selected after consultation with criminal justice experts, who suggested that a six-month incarceration point would be an appropriate cutoff, separating clients who were incarcerated for misdemeanor offenses from clients who committed felony offenses.
Measures
Baseline data included age, sex, race, marital status, duration of recent and past homelessness, employment, and income. For the baseline evaluation, clients were assessed with standardized measures (15) that addressed childhood background measures of abuse and stability of the family of origin (17); childhood conduct disorder (18); instrumental social support (19); self-reported severe medical problems; current psychiatric, alcohol, and drug problems (20); psychiatric status, including symptoms of depression and psychosis (21,22); and legal status (20). Counselor rated psychiatric diagnoses were obtained in a baseline interview.
Service use was assessed with a series of 23 questions about the use of various types of health and social services during the 60 days before the 12-month follow-up evaluation. These questions were grouped into five subcategories: employment assistance, housing support, medical and surgical outpatient services, psychiatric and substance abuse outpatient services, and public support payments. Costs for these services were determined by using published estimates of unit costs (23,24).
Twelve-month outcomes for housing status, employment status, and criminal justice involvement were determined by self-report. Twelve-month outcomes for psychiatric, alcohol, and drug problems were measured by using the instruments cited above.
Analyses
First, bivariate analyses were used to compare baseline characteristics across the three groups by using chi square tests and analysis of variance (ANOVA). Tukey tests were employed to identify significant differences between pairs of groups. Partial eta squares provided measures of strength of association between incarceration group status and the ANOVA dependent variables (25).
Next, we assessed the relationship between baseline incarceration history and 12-month follow-up status in six domains—housing status, employment status, psychiatric problems, alcohol problems, drug problems, and criminal justice involvement—by using multiple regression to control for potentially confounding baseline characteristics. In analyzing improvements in psychiatric and substance use problems, we included only clients who had such problems at baseline, that is, who had Addiction Severity Index scores for alcohol use or drug use greater than 0 or psychiatric scores greater than 0.
In the final phase of the analysis, differences in costs between the three groups for the 60 days before the 12-month assessment were compared by using ANOVA followed by Tukey tests. The significance level for all analyses was set at .05.
Results
Sample characteristics
Although baseline data were available for 7,055 clients, only 5,774 people were successfully assessed 12 months after program entry. Clients who were interviewed at the 12-month follow-up were not significantly different in clinical and social status from clients who were interviewed only at baseline and were not more likely to have been lost to incarceration (15).
Tables 1 and 2 show sample and group baseline characteristics. A total of 33 percent of the clients in this sample had no incarceration history, 35 percent had a short-term incarceration history, and 32 percent had a long-term incarceration history. Clients with a long-term incarceration history had higher psychiatric symptom scores, higher drug use and alcohol use scores, and higher levels of dual diagnosis than those with a short-term incarceration history or those with no history of incarceration. The same order of differences was found on measures of childhood abuse, family-of-origin stability, and childhood conduct disorder. Partial eta square analyses indicated small associations (partial eta square>.05)between incarceration group and family-of-origin stability andchildhood conduct disorder. With the exception of months of incarceration (partial eta square=.33), in all ANOVA analyses in which significant group differences were found, the degree of association between incarceration group and the dependent variable was very small (partial eta square≤.05).
Baseline social adjustment measures indicated slight but significant differences in recent days of homelessness between the two groups with a history of incarceration; the long-term-incarceration group spent more days homeless than the short-term group. Long-term homelessness was more characteristic of the group with a long-term incarceration history than of the group without an incarceration history. The short-term-incarceration group had higher instrumental social support scores than the long-term-incarceration group. The group with no incarceration history had the highest percentage of clients with a one-year pattern of unemployment.
Consistent with our first hypothesis, the two groups that had a history of incarceration showed higher levels of severe problems at baseline across a range of clinical and social background and adjustment measures than those with no incarceration history.
Service use and receipt of public support payments
As shown in Table 3, the group with no incarceration history used more outpatient psychiatric services during the study period than the group with a long-term incarceration history. In addition, the group with no incarceration history and the group with a short-term incarceration history received higher levels of public support payments and used more employment services than the long-term-incarceration group. Use of substance abuse services during the 60 days before the 12-month evaluation paralleled baseline levels of substance use problems; the two groups with a history of incarceration had higher use of substance abuse services than the group with no incarceration history.
Twelve-month outcomes and health care costs
Outcomes were measured for the 60 days before the 12-month follow-up interview for number of days homeless and number of days in jail and for the 30 days before the 12-month evaluation for number of days employed. Table 4 shows that the short-term-incarceration group did not differ from the group with no incarceration history in the number of days homeless, number of days employed, alcohol use and drug use scores, or number of days in jail. However, the short-term-incarceration group did have poorer psychiatric outcomes after the analysis controlled for baseline differences.
Substance use indicators were also higher for the two incarceration groups. When current alcohol use and drug use scores at the 12-month follow-up were controlled for in the psychiatric outcome analysis, differences between all three groups disappeared, indicating that the higher levels of psychiatric symptoms were associated with higher levels of substance abuse. However, even after we adjusted for substance use scores at 12-months, the long-term-incarceration group had poorer outcomes than the group with no incarceration history for number of days in jail. The hypothesis that clients with a long-term criminal history would have poorer 12-month outcomes than clients with no history of incarceration was thus supported on only two of the six outcomes, psychiatric problems and number of days in jail.
As shown in Table 5, health care costs during the 60 days before the 12-month follow-up revealed significant differences only in residential care costs, which were higher for the group with a long-term incarceration history. No difference was seen in total costs for health care services received in the past 60 days between the incarceration groups and the group with no incarceration history. Criminal justice costs for the 60 days before the 12-month follow-up interview were highest for the long-term-incarceration group, next highest for short-term-incarceration group, and lowest for the group with no incarceration history.
Discussion and conclusions
In this study, we analyzed baseline demographic, social, and clinical characteristics and 12-month follow-up levels of community service use, costs, and outcomes to compare homeless clients who had severe mental illness, grouped according to their history of incarceration. We hypothesized that clients with a history of incarceration would have higher levels of clinical and social adjustment problems at baseline and poorer 12-month outcomes. With the exception of unemployment, we confirmed this hypothesis: at baseline clients with a history of incarceration showed higher levels of social and clinical impairment. As hypothesized, we found higher levels of outpatient psychiatric and employment service use and public support payments for the group with no incarceration history and higher use of outpatient substance abuse services for the two groups with an incarceration history. Finally, after controlling for baseline differences, we found supporting evidence for the hypothesis of poorer 12-month outcomes among both groups with a history of incarceration. These findings are consistent with those of previous studies of homeless people (1,12,26).
Previously unaddressed issues center on treatment and outcomes. First, the clients with a history of incarceration had sustained contact with the ACCESS treatment program and had treatment services available to them, as did clients without a history of incarceration. The proportions of the initial sample that were successfully interviewed at the 12-month follow-up were 49 percent for those with no incarceration history, 42 percent for those with a short-term incarceration history, and 42 percent for those with a long-term incarceration history (χ2=17.90, df=2, p=.005). These differences were small, however, suggesting that the two groups with an incarceration history were almost as likely to sustain program contact as the group with no history of incarceration.
Even though clients with a history of incarceration had greater psychiatric and medical problems than those who had never been incarcerated, they used fewer outpatient psychiatric and medical services. However, they were more frequent consumers of outpatient substance abuse services than persons who had not been incarcerated. Finally, total health care costs for the two groups with a history of incarceration, although different between the two groups, were not significantly higher than total costs for the group with no incarceration history. Thus, although there were differences between all three groups in background and health status, homeless clients with a history of incarceration were not that different from those without such a history in terms of service use and overall health costs.
As hypothesized, clients with a history of incarceration did show poorer outcomes than those with no history of incarceration. Specifically, clients with any history of incarceration had poorer psychiatric outcomes, and those with a history of long-term incarceration were more likely to reenter the criminal justice system. When we entered 12-month alcohol use and drug use scores into the regression analysis for psychiatric outcome, no differences were seen between the three groups. Thus it appears that the poorer psychiatric outcomes at follow-up were associated with higher levels of current substance abuse, although we cannot make a causal inference.
The number of domains for which we found no differences between the three groups was unanticipated and deserves attention. Findings of this study provide some degree of hope for agencies and clinicians who are apprehensive about treating past offenders. Our findings also provide partial support for assertions (6,27) that assertive community treatment case management programs can be effective for homeless people with a mental illness and a history of incarceration and that among homeless people with mental illness, overall health costs are not substantially different for those with a history of incarceration.
Although other studies of community case management for ex-inmates have addressed recidivism outcomes (7,28), the significance of this study is in its analysis of service use and costs and of community social and clinical adjustment outcomes across a large sample of homeless people with severe mental illness who completed 12 months of assertive community treatment. The results of this study suggest that although people with a history of involvement in the criminal justice system do not fare as well as nonoffenders on some measures, they show similar improvements as nonoffenders on other measures. Therefore, homeless people with severe mental illness and a history of incarceration appear to benefit from treatment.
The primary limitations of this study are the fact that clients were recruited by convenience sampling and the absence of a comparison group, without which we cannot infer that the observed improvements were the result of treatment. Because clients were not drawn randomly from the potential client population, it is not clear how representative the clients in this study were of the population of homeless people with a severe mental illness and a history of incarceration. In particular, clients with an incarceration history who enter the ACCESS program may represent a subgroup that is especially amenable to treatment. Also, we were not able to measure the role of other potentially important factors that could contribute to outcome status, such as clients' background characteristics that were not included in the analysis or clients' inability to avoid involvement in the criminal justice system. However, although sociodemographic, clinical, and community adjustment characteristics of homeless persons vary considerably, the data reported in this study are within the parameters cited in other studies of homeless people who are incarcerated or who are living in the community (6). Although our outcome findings were mixed, they provide some empirical support and encouragement for treating this challenging population.
Acknowledgments
The Access to Community Care and Effective Services and Supports study was funded under interagency agreement AM9512200A between the Department of Health and Human Services Center for Mental Health Services and the Department of Veterans Affairs Northeast Program Evaluation Center. At the time of the study, Julie Lam, Ph.D., was project director at Northeast Program Evaluation Center for the client data collection during this study. Jennifer Cahil provided data management and programming support throughout. Don Hedeker, Ph.D., and Steven Banks, Ph.D., provided invaluable statistical consultation during the study. The evaluation coordinators and research assistants at each site were responsible for the success of this data collection effort. The authors thank the following local evaluation coordinators and their staffs for their invaluable assistance in collecting the data for this project. Simeon Goodwin, Ph.D., Jacob Tebes, Ph.D., Mardi Solomon, M.A., Sue Pickett, Ph.D., Greg Meissen, Ph.D., Robert Calsyn, Ph.D., Cheryl Roberts, M.A., Coleman Poses, M.S.W., Laverne Knezek, Ph.D., Deborah Webb, Ph.D., Marilyn Biggerstaff, D.S.W., and Peter Brissing, M.S.W.
Dr. McGuire is affiliated with the Northeast Program Evaluation Center of the Department of Veterans Affairs West Los Angeles Healthcare Center, Building 500, Room 6651, 11301 Wilshire Boulevard, Los Angeles, California 90073 (e-mail, james.mcguire@ med.va.gov). He is also with the School of Public Policy and Social Research at University of California, Los Angeles. Dr. Rosenheck is with the Northeast Program Evaluation Center of the Department of Veterans Affairs in West Haven, Connecticut, and with the department of psychiatry at the Yale University School of Medicine in New Haven.
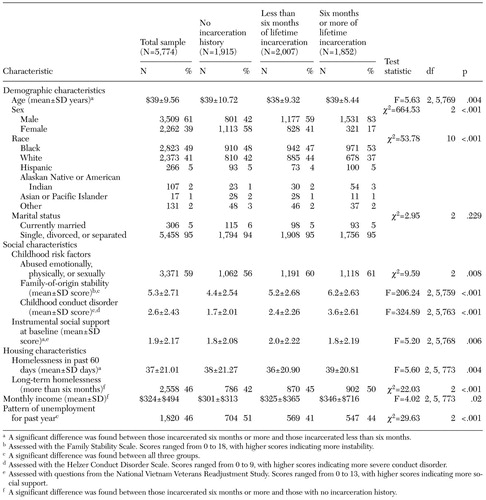 |
Table 1. Sociodemographic characteristics of clients who used ACCESS (Access to Community Care and Effective Services and Supports) services, by incarceration history
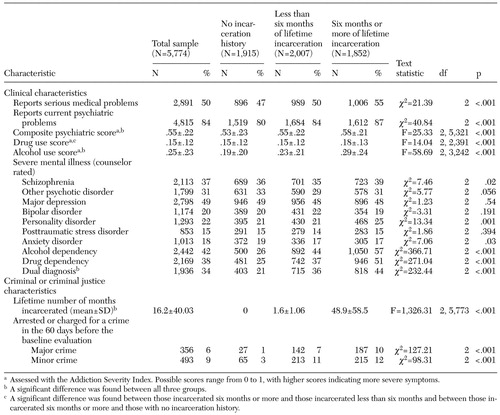 |
Table 2. Clinical and criminal justice characteristics of clients who used ACCESS (Access to Community Care and Effective Services and Supports) services, by incarceration history
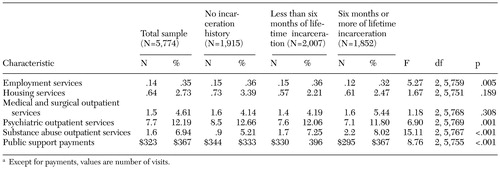 |
Table 3. Use of ACCESS (Access to Community Care and Effective Services and Supports) services among clients at the 12-month follow-up interview, by incarceration history
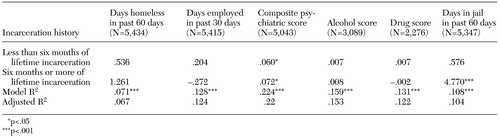 |
Table 4. Correlations (unstandardized betas) between 12-month outcome variables and incarceration histories of clients who used ACCESS (Access to Community Care and Effective Services and Supports) services
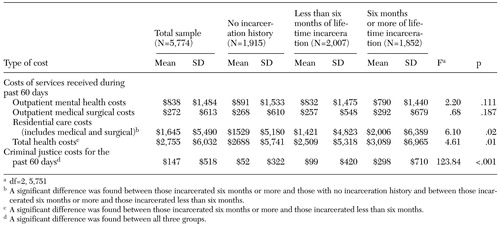 |
Table 5. Health care and criminal justice system costs incurred in the 60 days before the 12-month follow-up interview by clients who used ACCESS (Access to Community Care and Effective Services and Supports) services at the 12-month follow-up interview, by incarceration history
1. Fischer PJ: Criminal activity among the homeless: study of arrests in Baltimore. Hospital and Community Psychiatry 39:4 6–51, 1988Google Scholar
2. Burt MR, Aron LY, Douglas T, et al: Homelessness: Programs and the People They Serve. Findings of the National Survey of Homeless Assistance Providers and Clients. Washington, DC, Urban Institute, 1999Google Scholar
3. Fischer PJ, Shapiro S, Breakey WR, et al: Mental health and social characteristics of the homeless: a survey of mission users. American Journal of Public Health 76:519–524, 1986Crossref, Medline, Google Scholar
4. Illegal to Be Homeless: The Criminalization of Homelessness in the United States. National Coalition for the Homeless and the National Law Center on Homelessness and Poverty, 2003. Available at www.nation alhomeless.org/civilrights/crim2003/report1. htmlGoogle Scholar
5. Desai RA, Lam J, Rosenheck RA: Childhood risk factors for criminal justice involvement in a sample of homeless people with serious mental illness. The Journal of Nervous and Mental Disease 118:324–332, 2000Crossref, Google Scholar
6. Lamb HR, Weinberger LE: Persons with severe mental illness in jails and prisons: a review. Psychiatric Services 49:483–492, 1998Link, Google Scholar
7. Solomon P, Draine J, Meyerson A: Jail recidivism and receipt of community mental health services. Hospital and Community Psychiatry 45:793–797, 1994Abstract, Google Scholar
8. Solomon P, Draine J: Issues in serving the forensic client. Social Work 40:25–33, 1995Medline, Google Scholar
9. Rosenheck R, Frank J, Grabler M: Hospital treatment of patients with pending criminal charges: an ecological approach. Psychiatric Quarterly 58:255–268, 1987Crossref, Medline, Google Scholar
10. Rosenheck R: From conflict to collaboration: psychiatry and the hospital police. Psychiatry 48:254–263, 1985Crossref, Medline, Google Scholar
11. Prochaska JO: Stages of change approach to treating addictions with special focus on DWI offenders, in Research to Results: Effective Community Corrections. Edited by Harris PM. Lanham, Md, American Correctional Association, 1999Google Scholar
12. McGuire JF, Rosenheck RA, Kasprow WJ: Health status, service use, and costs among veterans receiving outreach services in jail or community settings. Psychiatric Services 54:201–207, 2003Link, Google Scholar
13. Randolph F, Blasinsky M, Morrissey JP, et al: Overview of the ACCESS Program. Psychiatric Services 53:945–948, 2002Link, Google Scholar
14. Morrissey JP, Calloway MO, Thakur N, et al: Integration of service systems for homeless persons with serious mental illness through the ACCESS Program. Psychiatric Services 53:949–957, 2002Link, Google Scholar
15. Rosenheck RA, Lam J, Morrissey JP, et al: Service systems integration and outcomes for mentally ill homeless persons in the ACCESS Program. Psychiatric Services 53:958–966, 2002Link, Google Scholar
16. Rosenheck RA, Lam J: Client and provider perceptions of service needs and their relationship to service use in a multisite program for homeless persons with mental illness. Psychiatric Services 48:387–390, 1997Link, Google Scholar
17. Kadushin C, Boulanger G, Martin J: Legacies of Vietnam, vol 4: Long Term Stress Reactions: Some Causes, Consequences, and Naturally Occurring Support Systems. House Committee Print no. 14. Washington, DC, US Government Printing Office, 1981Google Scholar
18. Helzer JE: Methodological issues in the interpretations of the consequences of extreme situations, in Stressful Life Events and Their Contexts. Edited by Dohrenwend BA, Dohrenwend BP. New York, Prodist, 1981Google Scholar
19. Kulka RA: The National Vietnam Veterans Readjustment Study. New York, Brunner/ Mazel, 1990Google Scholar
20. McClellan T, Luborsky L, Woody G, et al: An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. Journal of Nervous and Mental Disease 168:26–33, 1980Crossref, Medline, Google Scholar
21. Robins LN, Helzer JE, Crougham J, et al: The National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Archives of General Psychiatry 38:381–389, 1981Crossref, Medline, Google Scholar
22. Dohrenwend BP, Strout PE, Egri G, et al: Nonspecific psychological distress and other dimensions of psychopathology. Archives of General Psychiatry 37:1229–1236, 1980Crossref, Medline, Google Scholar
23. French MT, Martin RF: The costs of drug abuse consequences: a summary of research findings. Journal of Substance Abuse Treatment 13:453–466, 1996Crossref, Medline, Google Scholar
24. Kasprow WJ, Rosenheck R, Chapdelaine JD, et al: Health Care for Homeless Veterans: The Eleventh Annual Report. VA Northeast Program Evaluation Center. West Haven, Conn, VHA, August 1, 1998Google Scholar
25. Tabachnick BG, Fidell, LS: Using Multivariate Statistics, 2nd ed. New York, Harper and Row, 1989Google Scholar
26. Sherman LW, Gottfredson D, MacKenzie D, et al: Preventing Crime: What Works, What Doesn't, and What's Promising. A Report to the United States Congress. Department of Criminology and Criminal Justice, University of Maryland, 1997Google Scholar
27. Lehman AF, Dixon LB, DeForge BR, et al: A randomized trial of assertive community treatment for homeless persons with severe mental illness. Archives of General Psychiatry 54:1038–1043, 1997Crossref, Medline, Google Scholar
28. Ventura LA, Cassel CA, Jacoby JE, et al: Case management and recidivism of mentally ill persons released from jail. Psychiatric Services 49:1330–1337, 1998Link, Google Scholar



