Acute Stress Disorder, Alcohol Use, and Perception of Safety Among Hospital Staff After the Sniper Attacks
Abstract
OBJECTIVE: This study examined emotional and behavioral effects on hospital staff after a series of sniper shootings in the Washington, D.C., area. METHODS: Employees of a large tertiary care military hospital were anonymously surveyed about their perceptions of safety and threat, changes in activities, and peritraumatic dissociation as possible risk factors for acute stress disorder, depression, and increased alcohol use the week after the sniper suspects were captured. RESULTS: Of 382 study participants, whose average age was 39 years, 24 (6 percent) met criteria for acute stress disorder, 13 (3 percent) reported increased alcohol use, and 31 (8 percent) met criteria for depression. Risk factors for acute stress disorder were female sex (odds ratio [OR]=2.59), increased alcohol use (OR=5.1), comorbid depression (OR=7.28), lower perceived safety, higher perceived threat, higher levels of peritraumatic dissociation, and greater numbers of decreased activities. Risk factors for increased alcohol use were comorbid depression (OR=4.02), lower perceived safety, higher perceived threat, and higher levels of peritraumatic dissociation. Risk factors for depression were lower perceived safety and higher levels of peritraumatic dissociation. CONCLUSIONS: The sniper shootings were associated with substantial changes in perceived safety and threat assessment as well as decreased activities outside the home among highly educated hospital employees. Levels of acute stress disorder were similar to levels of posttraumatic stress disorder in New York City after the terrorist attacks of September 11, 2001. Peritraumatic dissociation was associated not only with acute stress disorder but also with depression and increased alcohol use after the attacks.
During the period from October 2 to October 22, 2002, ten people were killed and two additional people were wounded in a series of sniper attacks that spanned Maryland, Virginia, and the District of Columbia and stirred terror throughout the region. These acts of terrorism were inspired not by a political ideology but by a desire to create fear in the community and then extort money from local government. Because of the random targeting of victims, individuals in the community had limited ability to predict their own risk. The shootings occurred in multiple public settings. A teenage boy was shot as he prepared to enter his middle school. A bus driver was shot in the doorway of his bus. Other shootings occurred at gas stations, shopping malls, and a restaurant. The shootings occurred during daytime and evening hours. The victims had no common characteristics. Few clues were available to law enforcement officials.
Two suspects were finally apprehended on 24 October, 2002. The shootings drew widespread media coverage. School systems curtailed outdoor recess and after-school activities, and sports clubs postponed competitive events. Communities developed indoor alternatives to usual Halloween activities in anticipation that the shootings would continue through the end of the month.
The goals of terrorism are to erode personal and societal security and disrupt the continuity of community function (1). Terrorist acts create a chronic sense of decreased safety that may lead to altered health behaviors, long-term effects on emotional and physical health, and increased use of health care services (2). Three to five days after the terrorist attacks of September 11, 2001, an estimated 47 percent of the U.S. population were worried about their own safety or the safety of loved ones (3). In a survey of Manhattan residents, 24.6 percent also reported increased alcohol use at five to eight weeks after the September 11 attacks (4).
Most studies of the behavioral and psychological effects of shootings have been conducted in the context of a single event rather than an ongoing series of terrorist attacks. In one study, acute stress disorder was seen among 33 percent of persons who worked in the same office building at which multiple shootings occurred, even though the individuals studied did not personally witness the shootings (5). After a school shooting, 38.4 percent of children had moderate or severe symptoms of posttraumatic stress disorder (PTSD) one month after the event (6). In an urban teenage population, those who had directly witnessed a shooting were 1.93 times as likely to use alcohol as those who had not witnessed such an event (7).
Health care providers and hospital staff are often the first responders after a terrorist attack, particularly after bioterrorism or a chemical attack. Thus the effects of terrorism on the mental health of these individuals and their ability to perform their duties are of particular importance. The impact of terrorism on this group is important in planning for future health care resources and victim assistance programs.
Little is known about the effects of terrorism on hospital staff, although other groups of first responders have been studied (8,9). To assess the effects of terror, we studied the staff of a large hospital located in the suburban Washington, D.C., area. We examined perception of safety and threat, changes in activities, and symptoms of dissociation during or shortly after the event (peritraumatic dissociation) as possible risk factors for acute stress disorder, increased alcohol use, and depression in the week after the capture of the sniper suspects.
Methods
Study participants
We contacted military and civilian staff in one of the Washington, D.C., metropolitan area military hospitals after obtaining permission from senior hospital administrators and after review and approval by the institutional review board. The hospital provides a full range of inpatient and outpatient services and is the site of multiple graduate medical education programs. Fifty percent of the staff is military, and approximately 50 percent of the staff are involved in direct patient care, with the remainder serving in support and administrative areas. None of the sniper victims was admitted to this hospital, and, to our knowledge, none was related to any member of the staff.
An electronic questionnaire was distributed to 2,400 employees who had e-mail accounts. The questionnaire informed potential study participants of the voluntary nature of the study, discussed risks and benefits, and provided a contact point should participants have questions or concerns. To preserve confidentiality, the institutional review board waived the requirement for written informed consent. The questionnaire was distributed five days after the apprehension of the sniper suspects. Responses were collected during the next two weeks. Responses were routed anonymously through an Internet server. Of 415 responses received (response rate of 17 percent), we discarded 33 because major portions of the survey were incomplete, leaving 382 valid responses.
Of the 382 respondents, 209 (55 percent) were women, 207 (54 percent) belonged to the military, 233 (62 percent) were married, and 230 (60 percent) had children. The respondents' mean±SD age was 39±10.9 years. The group was predominately Caucasian (268 respondents, or 71 percent). All participants had at least a high school education; 207 (55 percent) had a college degree. The respondents included 49 physicians (13 percent), 53 nurses (14 percent), 55 medical technicians (14 percent), and 223 administrative employees (59 percent). The demographic distribution of the final sample closely resembled that of the overall sample of staff contacted.
Assessments
Acute stress disorder. Acute stress disorder was assessed for the week before the survey with use of the previously validated Acute Stress Disorder Inventory (10). This inventory requires endorsement of symptoms of intrusion, avoidance, hyperarousal, and dissociation in accordance with DSM-IV criteria.
Alcohol use and abuse. Presence of previous substance abuse was assessed with use of the CAGE questionnaire, with responses directed to the year before October 2002. The cutoff score of 1 was used to identify possible substance use problems. This cutoff score provides a sensitivity between .86 and .90 and a specificity between .52 and .93 (11). Alcohol use since October 2 was assessed with one question, "Did you increase your alcohol use for a period of two weeks or more?"
Depression. Depression was assessed with use of the Patient Health Questionnaire Depression Scale (PHQ-9) (12). A person is considered to be depressed when five or more of the nine symptoms have been present for more than half the days in the previous two weeks and one of the symptoms is depressed mood or anhedonia. Severity of depressive symptoms was measured with the sum of the responses to the PHQ-9, with nine items scored from 0, not at all, to 3, nearly every day, for a total score ranging from 0 to 27. A score of 10 or more indicates the potential need for treatment.
Peritraumatic dissociation. Peritraumatic dissociation was scored with use of an abbreviated version of the Peritraumatic Dissociative Experiences Questionnaire (PDEQ), with endorsement of symptoms ranging from 1, not at all true, to 5, extremely true (13). The full scale was used in a previous study with a similar population of persons who had been exposed to the September 11, 2001, attack on the Pentagon (14). Analysis of those data showed that Pearson correlations between the first five questions and the total score ranged from .62 to .83. The Pearson correlation between the five-item abbreviated scale and the ten-item scale was .97 (p<.001, Cronbach's alpha=.84). The score of the abbreviated scale was adjusted to produce a score consistent with the original ten-item scale (ranging from 10, no symptoms, to 50, high dissociation).
Perceived safety, perceived threat, and changes in activity. Respondents' general sense of safety was assessed with use of the Perceived Safety Scale. This scale was previously used in the study of the survivors of the Pentagon attack. The scale uses a total score from three questions: safety at work, safety at home, and safety throughout the day in usual activities and travel. Each item is scored on a 5-point Likert scale ranging from 1, not at all, through 5, extremely, with a range for the overall scale of 3, low safety, to 15, high safety (Cronbach's alpha=.78).
Perceived threat was assessed by using seven questions in which respondents were asked to rate the impact of the sniper attacks on their degree of concern about routine activities for themselves and their family—being in public places, buying gas, sending children to school or to extracurricular activities, attending large public gatherings, traveling by public transportation, traveling by car, and attending faith-based activities. Each item was scored on a 5-point Likert scale ranging from 1, none, through 5, extreme, with a range for the overall scale of 7, low perceived threat, to 35, high perceived threat (Cronbach's alpha=.92). Change in activity level was assessed with use of the same routine activities with choices of decrease, no change, increase, and not applicable. The number of activities decreased per person was totaled for a score ranging from 0 to 7.
Health care use. Use of health care services was assessed with two questions. One question asked for the number of visits to health care providers since the first sniper attack. Another question asked about the number of visits to mental health care providers since the first attack. Responses to these questions were converted to binary variables ("some visits" or "no visits").
Statistical analysis
Potential risk factors for acute stress disorder, depression, and increased alcohol use were evaluated by binary logistic regression against individual variables entered as categorical variables. The estimate of the odds ratio (OR) and its 95 percent confidence interval (CI) are reported. The Mann-Whitney test was used to evaluate differences in means between groups for continuous variables. Significance was set at .05. Statistical analysis was performed by with use of SPSS for Windows.
Results
Acute stress disorder, increased alcohol use, and depression
Of the 382 respondents 55 (14 percent) met criteria for one or more conditions. Twenty-four respondents (6 percent) met criteria for acute stress disorder, 13 (3 percent) reported increased alcohol use after the shootings, 31 (8 percent) met criteria for depression, eight (2 percent) had acute stress disorder and depression, three (1 percent) had acute stress disorder and also endorsed increased alcohol use, three (1 percent) had depression and also endorsed increased alcohol use, and one (<1 percent) reported acute stress disorder, increased alcohol use, and depression.
Perceived safety, perceived threat, and change in activity
A total of 146 respondents (38 percent) reported low perceived safety (moderate or less) in activities at home, at work, and in routine daily activities. A total of 150 respondents (40 percent) reported high perceived threat (moderate or above). Respondents reported mean±SD decreases of 1.35±1.94 of the seven areas of activity assessed. Women were 2.33 times as likely as men to report low perceived safety (Wald χ2=14.73, df=1, p<.001, 95 percent CI=1.51 to 3.59) and 2.24 times as likely to report high perceived threat (Wald χ2=13.54, df=1, p<.001, 95 percent CI=1.46 to 3.45). Women also reported greater decreases in activities than men (1.61±2.02 compared with 1.08± 1.81, U=15,104 Z=−2.838, p=.005).
Respondents who were unmarried were 1.73 times as likely to report low levels of safety (Wald χ2=6.26, df=1, p=.012, 95 percent CI=1.12 to 2.65) compared with those who were married. Those who were married reported a greater decrease in activities than those who were unmarried (1.49±1.94 compared with 1.18±1.96, U=14,355, Z=−2.38, p=.019). No association was found between marital status and perception of threat or between age and perception of safety, perception of threat, or change in activity.
Risk factors for acute stress disorder
Women were 2.59 times as likely as men to have acute stress disorder (Wald χ2=3.88, df=1, p=.049, 95 percent CI=1.01 to 6.68). Respondents with acute stress disorder were 7.28 times as likely to also have depression compared with those without the disorder (Wald χ2=16.85, df=1, p<.001, 95 percent CI=2.82 to 18.79) and were 5.1 times as likely to endorse increased alcohol use after the attacks (Wald χ2=5.46, df=1, p=.019, 95 percent CI=1.30 to 20.00). Respondents with acute stress disorder endorsed lower perceptions of current safety (U=2,045, Z=−4.348, p<.001), higher levels of perceived threat (U=1,757, Z=−4.614, p<.001), greater decreases in activities (U=3,129, Z=−2.44, p=.015), higher levels of peritraumatic dissociation (U=555, Z=−7.964, p<.001), and higher levels of depressive symptoms (U=884, Z=−6.167, p<.001) compared with those without acute stress disorder (Table 1). Respondents with acute stress disorder were 4.56 times as likely to have seen a mental health care provider since the shootings began compared with those without the disorder (Wald χ2=6.23, df=1, p=.013, 95 percent CI=1.38 to 15.01). No relationships were noted between acute stress disorder and previous substance abuse as measured by the CAGE, other health care visits, age, or marital status.
Risk factors for increased alcohol use
Respondents who reported increased alcohol use after the sniper attacks were 4.02 times as likely to have depression as those who did not report increased use of alcohol (Wald χ2=4.06, df=1, p=.044, 95 percent CI=1.04 to 15.54). In addition to the associations with acute stress disorder and depression, respondents who endorsed increased alcohol use reported lower perceived safety (U=944, Z=−3.699, p<.001), higher perceived threat (U=1512, Z=−2.170, p=.03), higher levels of peritraumatic dissociation (U=1514, Z=−2.39, p=.017), and higher levels of depressive symptoms (U=640.5, Z=−4.48, p<.001) compared with those who did not endorse increased alcohol use (Table 1). No associations were found between increased alcohol use and previous substance abuse, level of decreased activities, mental health visits, other health care visits, gender, age, or marital status.
Depression
In addition to the increased risk of acute stress disorder and increased alcohol use, respondents with depression reported lower perceived safety (U=3814, Z=−2.79, p=.005), higher levels of peritraumatic dissociation (U=2893, Z=−4.78, p<.001), and higher levels of depressive symptoms (U=47, Z=−9.06, p<.001) compared with those without depression (Table 1). Respondents with depression were 3.31 times as likely as those without depression to have seen a mental health care provider since the shootings began (Wald χ2=4.01, df=1, p=.045, 95 percent CI=1.02 to 10.66). Persons with depression were 2.67 times as likely to be single as those without depression (Wald χ2=6.38, df=1, p=.012, 95 percent CI=1.25 to 5.73). No associations were found between depression and previous substance abuse, perceived threat, numbers of decreased activities, other health care visits, gender, or age.
Discussion and conclusions
Although hospitals are a critical response component after terrorist attacks, hospital staff are also exposed as potential victims. The impact of terrorist attacks on the ability of health care providers to perform their assigned duties becomes an important part of planning for the availability of resources in a community. To our knowledge, this is the first study to examine psychological symptoms, behavioral changes, and safety and threat perception in a health care population after a three-week period of random terrorist activity. Although none of the study participants directly witnessed a shooting, all were potential victims during this period, resulting in levels of acute stress disorder (6 percent) comparable to those found among survivors of a series of typhoons (7 percent) (10). The rates of acute stress disorder and depression in this study were also similar to the rates of PTSD and depression in New York City one or two months after the September 11 terrorist attacks (8 percent and 10 percent, respectively) (15).
Altered perception of safety appears to be one of the major effects of terrorist events. In this study approximately 40 percent of the sample reported low perceived safety in routine daily activities or high levels of perceived current threat, compared with 60 percent reporting fear of terrorism at two months and 40 percent reporting fear of terrorism at six months after September 11 (16). In our study women were more likely than men to report lower safety and higher perceived threat and to decrease the number of routine activities. In general, decreased safety, increased perceived threat, and decreased activities were more strongly associated with acute stress disorder and increased alcohol use than with depression. Higher levels of peritraumatic dissociation were associated with acute stress disorder, increased alcohol use, and depression. This finding suggests a need for further study to determine the mechanisms by which individuals process information at the time of terrorist events and how this affects their psychological and behavioral responses to terrorism.
This study differed from other postdisaster studies in that questionnaires were distributed electronically within one week of the end of the terrorist event. Other studies have had greater response rates with the use of electronic polling in previously established study populations (17), but that design is less useful in targeting specific subgroups, as in this case, a hospital staff. The timely distribution provides the benefit of greatly reducing recall bias. Generalization of these results is limited, because selection biases are unknown. In addition, we did not determine whether depression or acute stress disorder were preexisting conditions among these patients or whether visits to health and mental health professionals had been scheduled before the shootings began.
Despite these limitations, we found a wide variance in endorsement of symptoms and behaviors and robust associations between perceptions and presence of psychiatric disorders.
The results of this study suggest that as many as 14 percent of hospital staff may have emotional or behavioral limitations after a terrorist attack. In general, these individuals can be expected to have a lower perception of safety and a higher perception of threat. Such individuals are more likely to alter their behaviors to cope with the threat and more likely to seek mental health care.
The authors are affiliated with the department of psychiatry of the Uniformed Services University of the Health Sciences, 430 Jones Bridge Road, Bethesda, Maryland 20814 (e-mail, [email protected]). Dr. Reeves is also affiliated with the department of psychiatry at the National Naval Medical Center in Bethesda. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the U.S. Government. This paper was presented as a poster at the annual meeting of the American Psychiatric Association held May 17 to 22 in San Francisco.
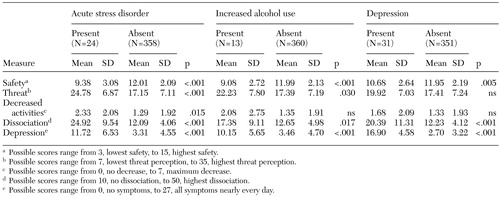 |
Table 1. Perceptions of threat and safety, changes in behavior, dissociation, and severity of depression in a sample of hospital staff after the Washington, D.C., area sniper attacks
1. Ursano RJ, Fullerton CS, Norwood AE (eds): Planning for Bioterrorism: Behavior and Mental Health Responses to Weapons of Mass Destruction and Mass Disruption. Bethesda, Md, Defense Technical Information Center, 2001 (available from authors on request)Google Scholar
2. Ursano RJ: Post-traumatic stress disorder. New England Journal of Medicine 346:130–132, 2002Crossref, Medline, Google Scholar
3. Schuster MA, Stein BD, Jaycox L, et al: A national survey of stress reactions after the September 11, 2001, terrorist attacks. New England Journal of Medicine 345:1507–1512, 2001Crossref, Medline, Google Scholar
4. Vlahov D, Galea S, Resnick H, et al: Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11th terrorist attacks. American Journal of Epidemiology 155:988–996, 2002Crossref, Medline, Google Scholar
5. Classen C, Koopman C, Hales R, et al: Acute stress disorder as a predictor of posttraumatic stress symptoms. American Journal of Psychiatry 155:620–624, 1998Link, Google Scholar
6. Pynoos RS, Frederick C, Nader K, et al: Life threat and posttraumatic stress in school-age children. Archives of General Psychiatry 44:1057–1063, 1987Crossref, Medline, Google Scholar
7. Pastore DR, Fisher M, Friedman SB: Violence and mental health problems among urban high school students. Journal of Adolescent Health 18:320–324, 1996Crossref, Medline, Google Scholar
8. North CS, Tivis L, McMillen JC, et al: Coping, functioning, and adjustment of rescue workers after the Oklahoma City bombing. Journal of Traumatic Stress 15:171–175, 2002Crossref, Medline, Google Scholar
9. Ursano RJ, Fullerton CS, Vance K, et al: Posttraumatic stress disorder and identification in disaster workers. American Journal of Psychiatry 156:3, 1999Google Scholar
10. Staab JP, Grieger TA, Fullerton CS, et al: Acute stress disorder, subsequent posttraumatic stress disorder, and depression after a series of typhoons. Anxiety 2:219–225, 1996Crossref, Medline, Google Scholar
11. Handbook of Psychiatric Measures. Washington, DC, American Psychiatric Publishing, 2000Google Scholar
12. Kroenke K, Spitzer RL: The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals 32:509–515, 2002Crossref, Google Scholar
13. Marmar CR, Weiss DS, Metzler TJ: The peritraumatic dissociative experiences questionnaire, in Assessing Psychological Trauma and PTSD. Edited by Wilson JP, Keane TM. New York, Guilford, 1997Google Scholar
14. Grieger TA, Fullerton CS, Ursano RJ: Posttraumatic stress disorder, alcohol use, and safety after the terrorist attack on the Pentagon. Psychiatric Services 54:1380–1383, 2003Link, Google Scholar
15. Galea S, Ahern J, Resnick H, et al: Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine 346:982–987, 2002Crossref, Medline, Google Scholar
16. Cohen Silver R, Holman EA, McIntosh DN, et al: Nationwide longitudinal study of psychological responses to September 11. JAMA 288:1235–1244, 2002Crossref, Medline, Google Scholar
17. Schlenger WE, Caddell JM, Ebert L, et al: Psychological reactions to terrorist attacks: findings from the National Study of Americans' Reactions to September 11. JAMA 288:581–588, 2002Crossref, Medline, Google Scholar