Posttraumatic Stress Disorder Among Cuban Children and Adolescents After Release From a Refugee Camp
Abstract
OBJECTIVE: The authors compared self-reported symptoms of posttraumatic stress disorder (PTSD) in a cohort of Cuban children and adolescents with assessments of internalizing and externalizing behaviors by the children's teachers. METHODS: Eighty-seven children and adolescents who had left Cuba by sea in the summer of 1994 and who had been confined to refugee camps for up to eight months before arriving in the United States were evaluated four to six months later. Self-reported symptoms of PTSD were assessed with the Post-Traumatic Stress Disorder Reactive Index, and internalizing and externalizing behaviors were assessed with the Child Behavioral Check List—Teacher Report Form. RESULTS: A majority of the children reported moderate to severe PTSD symptoms. The most common symptom clusters were avoidance (67 percent), regressive behaviors (64 percent), reexperiencing the traumatic events (60 percent), somatic symptoms (52 percent), and hyperarousal (51 percent). Eighty-six percent of the children reported that the refugee experience had severely affected most of their peers. A statistically significant dose-effect relationship was found between the number of stressors and the severity of self-reported PTSD symptoms. There was a modest relationship between withdrawn behavior and children's feelings that they would die at sea and witnessing violence at the camps. Age and witnessing violence in the camps were moderately associated with PTSD. Teachers' overall ratings of externalizing and internalizing behaviors did not produce any clinically significant findings. CONCLUSIONS: PTSD symptoms among refugee children and adolescents who have been exposed to multiple and prolonged stressors may continue unabated after the stressors are removed. The symptoms are experienced subjectively and may go unnoticed by adults.
In the past decade, a number of research studies have focused on the long-term effects of psychological trauma on refugee children and adolescents who arrive in the United States. Investigators have used the posttraumatic stress disorder (PTSD) framework to study child and adolescent victims of war and genocide in Cambodia (1,2,3,4,5,6,7), Tibet (8), and the countries of former Yugoslavia (9,10,11,12,13). In a study of Cambodian adolescent refugees in camps along the Thai border, a dose-effect relationship was found between traumatic exposure and psychiatric symptoms but not between traumatic exposure and social functioning (7).
In another study of Cambodian adolescents who were exposed to Khmer Rouge concentration camps, which was conducted six years after the adolescents arrived in the United States, 50 percent were diagnosed as having PTSD (1). This proportion was largely unchanged three years later (2). However, only 25 percent of Bosnian adolescents who were exposed to "ethnic cleansing" and were later reunited with their families in the United States met criteria for PTSD (9). The rate of PTSD was lower among the same adolescents a year later (12). The authors speculated that cultural differences between the refugees' country of origin and the receiving country may have accounted for the better adaptation and lower severity of PTSD among the Bosnian children than among the Cambodians.
Research findings on child and adolescent refugee populations can be summarized as follows. First, the effects of traumatic exposure vary by age, sex, and developmental stage. Girls are more prone to PTSD than boys; boys tend to manifest more aggressive behaviors, whereas girls are more prone to depressive reactions. Second, adolescents appear to be more resilient than younger children but are more prone to delayed reactions (14,15,16,17,18,19,20,21). Third, PTSD symptoms among adolescents tend to persist unabated for up to six years after exposure to the traumatic event, even though adolescents' social functioning remains high (4,5). Fourth, children are likely to be sheltered by family members during the conflict, whereas adolescents tend to become more directly involved, which increases their exposure to the traumatic events (18,20,21,22). Finally, although longitudinal data are still lacking, research findings suggest that early resilience may come at the cost of later development of psychiatric disorders, distorted defensive structures, exaggeration of normal developmental anxieties (18,21), difficulties with separation from the family of origin, or difficulties with the consolidation of identity (9,23).
The Cuban exodus of 1994
The deterioration of financial and political conditions in Cuba reached an unprecedented state in the summer of 1994. This situation was due largely to the collapse of the Soviet Union in 1991, which interrupted commerce and supplies to the island. The crisis was followed by civilian protests, hijacking of boats and ferries, and violent confrontations with government authorities. Fearing the possibility of a civil war, the Cuban government opened its borders on August 12, 1994, allowing any discontented individuals to leave the island. This announcement culminated in a massive exodus by sea in which several thousand people fled by using boats, rafts, and other small craft to reach the United States (24). Children and adolescents described witnessing people passing out or dying from starvation and thirst during the ocean crossing, as well as seeing floating human corpses being devoured by sharks. Others witnessed storms, the sinking of boats and rafts, and drownings.
Editor's Note: This paper is part of an occasional series on anxiety disorders edited by Kimberly A. Yonkers, M.D. Contributions are invited that address panic disorder, agoraphobia, obsessive-compulsive disorder , social phobia, posttraumatic stress disorder, generalized anxiety disorder. Papers should focus on integration new information that is clinical relevant and that has the potential to improve some aspect of diagnosis or treatment. For more information, please contact Dr. Yonkers at 142 Temple Street, Suite 301, New Haven, Connecticut 06510; 203-764-6621; [email protected].
About 32,400 people were intercepted at sea by the U.S. Coast Guard and taken to refugee camps at the U.S. Naval Base at Guantanamo Bay in eastern Cuba and to other Caribbean locations (25). The U.S. Coast Guard deployed 56 vessels in the largest naval mobilization since the Korean War, termed Operation Able Vigil (24). It is not known how many people died at sea, but studies of previous exoduses have indicated that only 25 percent of those who attempt such a crossing survive (24). However, the massive rescue operations by the U.S. Coast Guard may have drastically reduced the casualty rate (25). Once rescued in international waters by smaller U.S. Coast Guard vessels, the refugees were transferred to a "mother ship," where they remained for up to five days before being transferred to the refugee detention camps at Guantanamo Bay (24).
The refugees were confined to detention camps at the naval base for an average of six to eight months. They were subjected to obligatory confinement in a space surrounded by barbed wire and armed guards. In the camps, the children witnessed riots, arrests, multiple acts of violence, suicide attempts, profanity, explicit sexual activity, and frequent surprise searches by U.S. military personnel, who penetrated the tents looking for weapons. Tension was aggravated by the physical conditions of the camps, including heat, mosquitoes, dust, poor hygiene, a monotonous diet, and cramped living space. The prolonged periods of idleness, coupled with an uncertain fate, gave way to fatalistic rumors that the refugees would be returned to the island to face retaliation by Cuban authorities.
Finally, on November 3, 1994, the U.S. government announced that all refugee children under 18 years of age and their nuclear families would be paroled into the United States. However, the slow bureaucratic process of providing the refugees with U.S. visas, administered by the Immigration and Naturalization Service in the camps, would take up to one more year to complete (26,27,28). On November 14, 1994, the refugees endured another catastrophic event when Tropical Storm Gordon blew away the tents and flooded the camps, causing the refugees to lose their shelter and personal possessions.
We previously found an elevated number of PTSD symptoms in a clinic population (27) and in a subgroup of Cuban children and adolescents who were confined to the Guantanamo Bay refugee camps (28). In the study reported here, we examined a group of children and adolescents between the fourth and sixth month after they were released from the refugee camps to assess the prevalence of self-reported PTSD symptoms and to compare the findings with the children's teachers' perceptions of internalizing and externalizing symptoms. The children did not have a history of premorbid psychiatric conditions in Cuba or in the camps. The study was conducted while the children were attending a transitional summer school program sponsored by the Catholic Archdioceses of Miami to facilitate their adaptation to the U.S. public school system.
We previously studied a clinic population of children inside the camp infirmaries by using the Post-Traumatic Stress Disorder Reactive Index (PTSDRI) (27,29). We found an elevated number of self-reported PTSD symptoms in this cohort. We noted that this particular group of children were the most deeply affected by their experiences in the camps and presented with the highest number of externalizing behaviors; that the children in the clinic sample had an elevated number of premorbid psychiatric conditions; and that during camp confinement, rumors among the refugees propagated the belief that if children were found to have an increased severity of PTSD symptoms, they would obtain faster entry into the United States.
These factors may have resulted in a more biased sample. For this study, we selected a more "low-impact" sample, in contrast with this highly symptomatic clinic population of children and adolescents who were studied inside the camp infirmaries (27). None of the children in our school sample had presented to the camp infirmary or reported any symptoms of psychiatric or conduct disorders during their confinement that would have necessitated psychiatric intervention. During camp confinement, the distress of these children and adolescents was contained within the family unit.
We hypothesized that exposure to certain stressors would increase the likelihood of PTSD, which has been reported by other investigators (1,2,3,4,5); that the prevalence of self-reported (subjective) PTSD symptoms would remain elevated in this group after the stressors had been removed, as has been found in similar studies (4,5,6,7); that PTSD symptoms would present silently and go unnoticed by the adults (teachers) responsible for these children, as has previously been reported (2,3,4,5,7,9,10,11,12,13); that girls would be more symptomatic than boys; and that younger children (six to 12 years old) would be more symptomatic than adolescents, which is a consistent finding in the child PTSD literature (21).
We selected these hypotheses on the grounds that the literature is replete with research demonstrating the difficulty in diagnosing PTSD in populations of child and adolescent refugees by clinical observation alone. In addition, we aimed to highlight the need to refine diagnostic instruments and to better understand particular predisposing factors and stressors that increase the severity of PTSD among these children. We believed that our findings could help clinicians who treat these populations to better identify children who are more at risk of developing PTSD. Once these children are identified, appropriate treatment strategies and preventive interventions can be implemented.
Methods
Subjects
The initial cohort consisted of 89 children and adolescents. Two children were excluded from the study because of incomplete data, for a final sample of 87. The children were interviewed while attending one of five transitional summer schools in the Greater Miami area. The Catholic Archdioceses of Miami sponsored these schools to help the children make the transition into the U.S. public school system. All the children left Cuba with their families by sea, had been confined to refugee camps at the U.S. naval base at Guantanamo Bay for an average of six to eight months, and had been living in Miami for four to six months when the interviews commenced. No efforts were made to classify children by ethnicity because of the diverse racial mix of the Caribbean islands and the inherent difficulty of such a task.
Materials
A questionnaire was administered to the parents in Spanish to obtain demographic information about the children and their families. The children and adolescents were administered the PTSDRI. This instrument has 21 questions that assess the degree of PTSD among children and adolescents. It has a reliability of .91, and the items conform with DSM-III-R (30) for the diagnosis of PTSD. Symptoms are rated on a 5-point ordinal scale from 1, none of the time, to 5, most of the time. The instrument produces a total score that translates into five categories: doubtful, mild, moderate, severe, and very severe.
Because of the relatively small sample in this study and to make the results more understandable, the five categories were collapsed into 1, none (never or a few times); 2, moderate (sometimes or many times); and 3, severe (all the time). The instrument was translated into Spanish by using the method established by Breslin (31). To examine the individual questions in terms of the PTSD criteria from DSM-III-R and DSM-IV, the 21 questions were grouped into five categories: reexperiencing phenomena, avoidance, increased arousal, regressive behavior, and, for items that did not fit into the other categories, miscellaneous.
To assess behavioral problems, 11 teachers rated the children by using the Child Behavioral Check List—Teacher Report Form (CBCL-TRF) (32). The CBCL-TRF consists of 113 questions and computes scores for profiles in ten separate categories: internalizing behaviors, externalizing behaviors, aggression, anxiety-depression, attention problems, delinquent behavior, social problems, somatic complaints, thought problems, and withdrawn behavior.
Procedures
The children and adolescents were interviewed during the first three weeks of July 1995. We met with the parents, explained the purpose of the study, and obtained informed consent. The PTSDRI (29,31) was administered to the children in Spanish by a U.S.-trained psychiatrist (EMR), three Cuban-trained psychiatrists (HCM, RB, and LG), two Cuban-trained family physicians (EB and EA), and a Cuban-trained psychologist (CMG)—all of whom had been refugees themselves—as well as by two school psychologists (OM and IM). All the test administrators spoke Spanish as their first language, had been given a four-hour training session by the first author on the use of the PTSDRI, and were able to confer frequently with the first author about the use of the instrument. On the basis of practice administrations of the instrument, the reliability was .75.
The children were observed in the classroom and rated by their 11 American-trained teachers with the CBCL-TRF (32). The teachers were provided with a four-hour training session by the first author on using the English version of the CBCL-TRF and were able to ask him any questions about administration of the measure. All the teachers either spoke Spanish as their first language or were completely bilingual in English and Spanish.
The children were also asked seven questions about the degree of their exposure to traumatic events, such as "Did you leave in a raft or in a boat?"; "How many days did you spend at sea?"; and a list of events that occurred during the ocean crossing: "Did you see sharks?"; "Did you see someone drown or die during the crossing?"; "Did you feel that you would die?"; and "Did the Cuban authorities try to stop you when you were trying to leave?" Finally, they were asked to respond to "What was the worst moment of the whole ordeal?" The possible answers were the ocean crossing, life in the camps, and Tropical Storm Gordon. For the yes-or-no questions, a total exposure variable was summed for the number of positive responses.
Data analyses
Data were entered into a database and analyzed with SPSS for Windows. Frequency and descriptive statistics were used to establish means, standard deviations, and other relevant characteristics of the data. The Pearson product-moment correlation for two continuous variables and the point-biserial correlation for one dichotomous variable and one continuous variable were used to examine relationships between the study's variables—for example, PTSDRI and exposure to stressors. Age, gender, months spent in the camp (four to six months or six or more months), and the yes-or-no exposure questions were entered as independent variables into multiple linear regression equations with the behavioral problems measured by the CBCL-TRF and PTSDRI as dependent variables. Nominal variables were recoded in a binary or dummy format.
Results
The average age of the children and adolescents was 14.9 years, with a range of six to 17 years. Forty-five (52 percent) were six to 12 years old, of whom 24 (27 percent) were boys and 21 (24 percent) were girls, and 42 (48 percent) were adolescents (13 to 17 years old), of whom 26 (30 percent) were boys and 16 (18 percent) were girls. Eighteen of the children and adolescents (21 percent) had left their father behind in Cuba, 11 (13 percent) had left their mother behind, 20 (24 percent) had left a brother or sister, 58 (69 percent) had left one or more grandparents behind, and 66 (79 percent) had left an aunt or an uncle.
The responses to the PTSDRI and the questions about exposure to stressors are summarized in Tables 1 and 2. On the PTSDRI, 37 of the children and adolescents (43 percent) showed no evidence of PTSD, 28 (32 percent) showed evidence of moderate PTSD, and 22 (25 percent) showed evidence of severe PTSD. Thus 50 children (57 percent) were considered to have PTSD according to the PTSDRI. Correlations of the CBCL-TRF with the PTSDRI and exposure to stressors were nonsignificant. A significant positive correlation was found between the total number of stressors to which a child was exposed and the score on the PTSDRI (r=.34, p<.01).
We evaluated the effects of age, gender, months spent in the camp, and responses to the yes-or-no questions about exposure on scores on the behavioral scales of the CBCL-TRF and the PTSDRI. All equations were nonsignificant—that is, the overall F test was nonsignificant, except for trends found for the withdrawn scale on the CBCL-TRF (p<.09) and the score on the PTSDRI (p<.09). For the withdrawn scale, feeling that one would die at sea and witnessing acts of violence at the camp were the only significant predictors, as can be seen in Table 3. For the score on the PTSDRI, age (t=2.06, p<.05) was the only significant predictor, as can be seen in Table 4; the effect of witnessing acts of violence at the camp approached significance (p=.06).
Discussion
Traumatic events such as fleeing on an ocean journey with inadequate means; being exposed to death, violence, harsh weather, and poor environmental conditions; and being confined in a military refugee camp can have profound and long-lasting effects on children and adolescents. We examined children and adolescents who left Cuba with members of their families, were rescued by the U.S. military, and were taken to camps at Guantanamo Bay. Up to six months after leaving the refugee camps, a majority of children in our sample reported moderate to severe symptoms of PTSD, including avoidance, regressive behaviors, reexperiencing the traumatic events, somatic symptoms, and hyperarousal.
Most of the children reported that the refugee experience had severely affected their peers. We found modest significant relationships between self-reported PTSD symptoms and withdrawn behavior with age and exposure to certain stressors, such as violence. However, none of the 11 teachers reported observing any clinically significant internalizing or externalizing behaviors among the children and adolescents.
A majority of the children left Cuba accompanied by intact nuclear families. However, most of them had left behind grandparents and other members of the extended family. This separation constitutes a significant emotional loss to children in a culture that places great importance on the extended family and in which the grandparents and other relatives care for the children when both parents are at work (33).
The children and adolescents were exposed to multiple stressors during the ocean crossing. These stressors appeared to be less severe than those found among a highly symptomatic population of children and adolescents who were seen inside the camps for psychiatric care (27). However, no statistically significant correlations between the stressors and the severity of self-reported PTSD symptoms were found in that sample.
The global score on the self-report PTSDRI indicated that a majority of the children continued to experience moderate to severe symptoms of PTSD four to six months after they left the camps. The most severe types of symptoms reported were avoidance, regressive behaviors (characterized by separation anxiety and clinging behaviors), and reexperiencing of symptoms. All three clusters of symptoms tend to be less florid and more subjective than the symptoms of hyperarousal. Therefore, the symptoms may be less likely to result in the child's being singled out as problematic in a group situation, which would make the child's distress less likely to be noticed by the adults responsible for his or her care.
In the cluster of miscellaneous symptoms, a majority of children considered the migratory experience to have had a strong impact on their lives and on the lives of most of their peers. The children tended to attribute personal meanings to the experience, which varied considerably among the children. The personal meanings of the experience should be explored in individual psychotherapy, because the meaning attached to these experiences may acquire importance in later stages of the child's development and adult life.
Somatization was reported by more than half of the cohort and represents a common expression of internal distress in most children. Surprisingly, only a quarter of the sample reported an onset of externalizing behaviors after the migratory experience. This finding reflects a more subjective and less overtly noticeable expression of the traumatic experience among these children.
In the regression analysis we found a trend toward statistical significance for the withdrawn scale of the CBCL-TRF. A feeling that one would die at sea and witnessing acts of violence in the camps contributed to withdrawn behavior. These findings suggest that internal and external factors combined to contribute to withdrawn behavior in our sample. We also found a trend on the total score of PTSDRI. Being older and witnessing acts of violence in the camps were the significant predictors of this self-report measure. Although the experience of witnessing violence contributed to both behaviors, older children may appear more resilient during the actual traumatic situation but be more prone to experiencing delayed reactions once the stressors have been removed. The family usually shelters older children less than younger children, so these older children may suffer more direct exposure to the traumatic situation.
Also, the finding of witnessing violence was consistent across self-report and observation by a caretaker (a teacher). This finding suggests that violence in a chaotic and traumatic situation will be readily apparent to children and adolescents, as well as to their teachers, and that such experiences will have an impact on the various domains of functioning reported by both.
Our findings are similar to those of other investigators (1,7), which reveal that after the stressors have been removed, subjective levels of severity of PTSD symptoms among children and adolescents remain high, while social functioning—in our study, functioning in a classroom—remains relatively unaffected. In our study, even though teachers reported that the children exhibited mild difficulties in certain areas, the overall academic and social functioning was found to be largely intact.
Conclusions
The results of this study are important to parents, educators, mental health professionals, government authorities, and anyone in receiving communities who come into contact with newly arrived child and adolescent refugees. Our findings highlight the difficulties encountered by teachers in identifying psychologically traumatized child and adolescent refugees who need psychiatric treatment. They also suggest that certain characteristics, such as exposure to stressors and exposure to another person's death or attempted suicide and other types of violence, increase the severity of PTSD and have an impact on particular areas of functioning.
The significance of subjective PTSD symptoms with high levels of psychosocial functioning in this population and the long-term prognosis of these children remain to be determined. The results of our study underscore the need for long-term follow-up studies in this population. Despite their relatively intact psychosocial functioning, these children continued to experience subjective psychic suffering and internal distress.
Clinicians should be alert to the presence of PTSD when they encounter refugee children in their practices. Self-report questionnaires, a comprehensive psychosocial history, and a psychiatric interview should be conducted to more accurately identify subjective psychic suffering and to provide appropriate treatment for these children. Finally, our results highlight the importance of developing culturally sensitive, ethnographic research methodology and instrumentation for research among refugees so that research findings can be applied appropriately.
Dr. Rothe is associate professor of psychiatry and pediatrics at the University of Miami School of Medicine, P.O. Box 305, Key Biscayne, Florida 33149 (e-mail, [email protected]). Dr. Lewis is assistant professor of psychology at the University of Miami School of Medicine. Dr. Castillo-Matos and Dr. Busquets are affiliated with Miami Behavioral Health Center. Mr. and Mrs. Martinez are co-principals of the School of the Americas. An earlier version of this paper was presented at the Institute on Psychiatric Services held October 25-29, 2000, in Philadelphia.
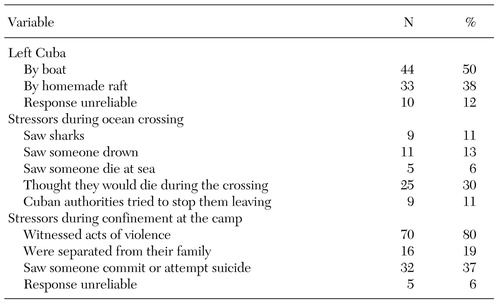 |
Table 1. Exposure to stressors among Cuban children and adolescents after release from confinement in refugee camp
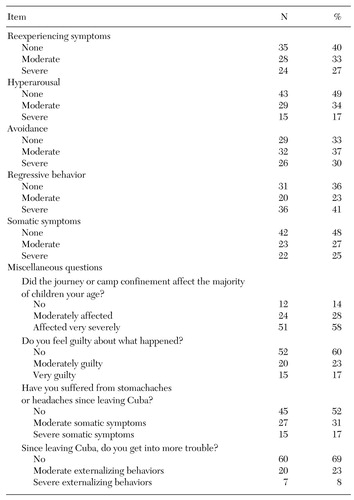 |
Table 2. Cuban children's responses to items on the Post-traumatic Stress Disorder Reactive Index
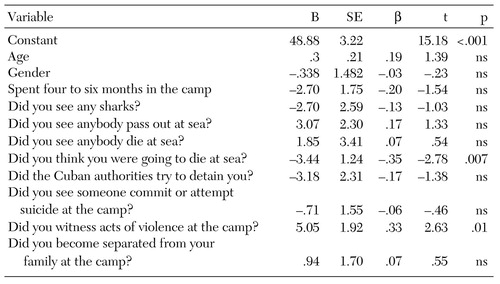 |
Table 3. Results of multiple linear regression using "withdrawn" as the dependent variable
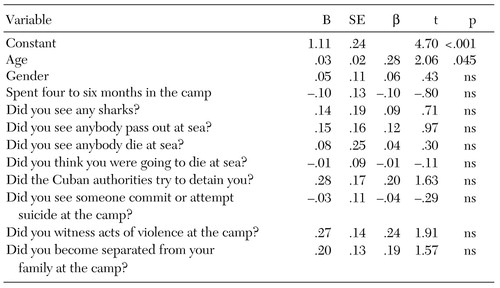 |
Table 4. Results of multiple linear regression using Post-traumatic Stress Disorder Reactive Index as the dependent variable
1. Kinzie JD, Sack W, Angell R, et al: The psychiatric effects of massive trauma on Cambodian children: I. the children. Journal of the American Academy of Child and Adolescent Psychiatry 25:307-376, 1986Google Scholar
2. Kinzie JD, Sack W, Angell R, et al: A three year follow-up of Cambodian young people traumatized as children. Journal of the American Academy of Child and Adolescent Psychiatry 28:501-504, 1989Crossref, Medline, Google Scholar
3. Kinzie JD, Boehnlein JK, Leung PK, et al: The prevalence of post-traumatic stress disorder and its clinical significance among Southeast Asian refugees. American Journal of Psychiatry 147:913-917, 1990Link, Google Scholar
4. Sack WH, Clarke G, Hin C, et al. A six-year follow-up study of Cambodian adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 32:431-437, 1993Crossref, Medline, Google Scholar
5. Sack WH, McSharry S, Clarke G, et al: The Khmer Adolescent Project: I. epidemiologic findings in two generations of Cambodian refugees. Journal of Nervous and Mental Disease 1982:387-395, 1994Crossref, Google Scholar
6. Savin D, Sack WH, Clarke GN, et al: The Khmer Adolescent Project: III. a study of trauma from Thailand's site II refugee camp. Journal of the American Academy of Child and Adolescent Psychiatry 35:384-391, 1996Crossref, Medline, Google Scholar
7. Mollica RF, Poole C, Son L: Effects of war trauma on Cambodian refugee adolescents' functional and mental health status. Journal of the American Academy of Child and Adolescent Psychiatry 36:1098-1106, 1997Crossref, Medline, Google Scholar
8. Servan-Schreiber D, Lelin B, Birmaher B: Post-traumatic stress disorder and major depressive disorder in Tibetan refugee children. Journal of the American Academy of Child and Adolescent Psychiatry 37:874-879, 1998Crossref, Medline, Google Scholar
9. Weine S, Becker DF, McGlashan TH, et al: Adolescent survivors of "ethnic cleaning": observations on the first year in America. Journal of the American Academy of Child and Adolescent Psychiatry 34:1153-1159, 1995Crossref, Medline, Google Scholar
10. Weine SM, Becker DF, McGlashan TH, et al: Psychiatric consequences of "ethnic cleaning": clinical assessment and trauma testimonies of newly resettled Bosnian refugees. American Journal of Psychiatry 152:536-542, 1995Link, Google Scholar
11. Weine SM, Vojvoda D, Becker DF, et al: PTSD symptoms in Bosnian refugees one year after resettlement in the United States. American Journal of Psychiatry 155:562-563, 1998Link, Google Scholar
12. Becker DF, Weine SM, Vojvoda D, et al: PTSD symptoms in adolescent survivors of "ethnic cleansing": results from a one-year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry 38:775-781, 1999Crossref, Medline, Google Scholar
13. Weine SM: When History Is a Nightmare: Lives and Memories of Ethnic Cleansing in Bosnia Herzegovina. Piscataway, NJ, Rutgers University Press, 1999Google Scholar
14. Gleser G, Green BL, Winget C: Prolonged Psychological Effects of Disaster: A Study of Buffalo Creek. New York, Academic, 1981Google Scholar
15. Terr LC: Chowchilla revisited: the effect of psychic trauma four years after a school bus kidnapping. American Journal of Psychiatry 140:1543-1550, 1983Link, Google Scholar
16. Terr LC: Childhood trauma: an outline and overview. American Journal of Psychiatry 148:1-20, 1991Link, Google Scholar
17. Green BL, Korol M, Grace MC: Children and disaster: age, gender, and parental effect on PTSD symptoms. Journal of the American Academy of Child and Adolescent Psychiatry 30:945-951, 1991Crossref, Medline, Google Scholar
18. Jensen PS, Shaw JA: Children as victims of war: current knowledge and future research needs. Journal of the American Academy of Child and Adolescent Psychiatry 32:697-708, 1993Crossref, Medline, Google Scholar
19. Green BL, Grace MC, Vary MG, et al: Children of disaster in the second decade: a 17 year follow-up of the Buffalo Creek survivors. Journal of the American Academy of Child and Adolescent Psychiatry 33:71-79, 1994Crossref, Medline, Google Scholar
20. Sack WH: Multiple forms of stress in refugee and immigrant children. Child and Adolescent Psychiatry Clinics of North America 7:153-167, 1998Crossref, Medline, Google Scholar
21. Shaw JA: Children, adolescents, and trauma. Psychiatric Quarterly 71:227-243, 2000Crossref, Medline, Google Scholar
22. Pynoos RS, Steinberg AM, Wraith R: A developmental model of childhood traumatic stress, in Developmental Psychopathology, vol 2. Edited by Chicchetti D, Cohen DJ. New York, Wiley, 1995Google Scholar
23. Weine SM, Vojvoda D, Hartman S, et al: A family survives genocide. Psychiatry 60:24-39, 1997Crossref, Medline, Google Scholar
24. Ackerman H, Clark J: The Cuban Balseros: Voyage of Uncertainty. Miami, Policy Center of the Cuban American National Council, Inc., 1995Google Scholar
25. United States Seventh Coast Guard District: Cuban Rescue Statistics:1981-1995. Miami, Public Affairs Office, 1995Google Scholar
26. Alvarez L: Elated exiles prepare to meet their loved ones: first 10,000 detainees could arrive next week. Miami Herald, Nov 7, 1994, p 1AGoogle Scholar
27. Rothe E, Castillo H, Busquets R, et al: Posttraumatic symptomatology in Cuban adolescent refugees during camp confinement. Adolescent Psychiatry 26:97-124, 2002Google Scholar
28. Rothe E, Castillo H, Brinson K, et al: La odisea de los balseros Cubanos. [The odyssey of the Cuban rafters.] Medico Interamericano 19:578-581, 2000Google Scholar
29. Frederick CJ, Pynoos RS, Nader K: Post-traumatic Stress Disorder Reactive Index. University of California, Los Angeles, department of psychiatry, 1992Google Scholar
30. Pynoos RS: Scoring and Interpretation of the Post-Traumatic Stress Disorder Reactive Index (PTSDRI). University of California, Los Angeles, department of psychiatry, 1992Google Scholar
31. Breslin R: The wording and translation of research instruments, in Field Methods in Cross-Cultural Research. Edited by Loaner WJ, Berry TW. Beverly Hills, Calif, Sage, 1986Google Scholar
32. Achenbach TM, Edelbrock C: Manual for the Teacher Report Form and Teacher Version of the Child Behavioral Profile. Burlington, University of Vermont, department of psychiatry, 1986Google Scholar
33. Bernal G: Cuban families, in Ethnicity and Family Therapy. Edited by McGoldrick M, Pearce JK, Giordano J. New York, Guilford, 1982Google Scholar



