Datapoints: Variations in Mental Health Specialty Care Across Metropolitan Areas
Health care disparities associated with sociodemographic characteristics are well known, but little is known about how area of residence affects service use. Although no recent data on geographic variations in mental health care in the general population are available, there are reasons to suspect that mental health care differs across areas: Medicare spending, for example, varies by more than a factor of two across regions, with even wider variations in certain procedures and no relationship between health care quality and costs (1).
We estimated annual rates of mental health specialty care among school-age children and adults across the 12 primary sites of the Community Tracking Study conducted by the Center for Studying Health System Change (2). We pooled the data from the first two waves to increase the sample sizes after testing for significant time trends (we found none). About half the respondents in the study are at the 12 primary sites (6,343 children and 44,975 adults), and the other half are at 48 secondary sites.
Figure 1 suggests that there are substantial regional variations in specialty care in the United States. Indeed, focusing on national averages obscures differences whose impact is greater than that of sociodemographic factors. Regional rates for children across the 12 communities can differ by 170 percent, with rates ranging from less than 5 percent in Phoenix to more than 13 percent in Boston, both significantly different from the national average of 8.6 percent. Even wider variations exist across all 60 communities of the larger study, some of which have significantly lower rates than Phoenix.
The geographic variations for adults largely replicate the patterns for children. The larger samples for adults also provide better statistical power; rates of specialty care at five of the sites are significantly different from the national average of 7.1 percent.
The Community Tracking Study data do not allow us to determine the extent to which variations in need account for variations in use. However, for medical procedures among Medicare recipients, need was generally found to be a minor contributor to geographic variations. Legal and market factors, including the supply of psychiatrists, are more likely determinants of service use and are independent of patients' needs.
Acknowledgments
This research was funded by the Robert Wood Johnson Foundation's Changes in Health Care Financing and Organization program and by the Child Mental Health Foundation and Agency Network.
The authors are affiliated with Rand 1700 Main Street, Santa Monica, California 90401 (e-mail, [email protected]). Harold A. Pincus, M.D., and Terri L. Tanielian, M.A., are editors of this column.
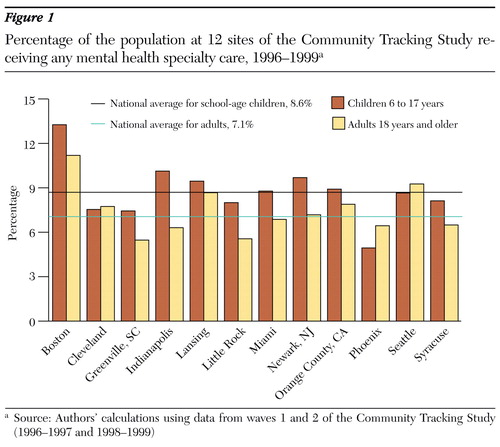
Figure 1. Percentage of the population at 12 sites of the Community Tracking Study receiving any mental health specialty care, 1996-1999a
a Source: Authors' calculations using data from waves 1 and 2 of the Community Tracking Study (1996-1997 and 1998-1999)
1. Wennberg JE, Fisher ES, Skinner JS: Geography and the debate over Medicare reform. Health Affairs Web Exclusive W96-W114, 2002Google Scholar
2. Kemper P, Blumenthal D, Corrigan JM, et al: The design of the Community Tracking Study: a longitudinal study of health system change and its effects on people. Inquiry 33:195-206, 1996Medline, Google Scholar