An Analysis of Reported Deaths Following Electroconvulsive Therapy in Texas, 1993-1998
Abstract
Since 1993, Texas law has required that all deaths that occur within 14 days of electroconvulsive therapy (ECT) be reported to the Texas Department of Mental Health and Mental Retardation. This study attempted to differentiate deaths that may have been due to ECT or the associated anesthesia from those due to other causes. Among more than 8,000 patients who received 49,048 ECT treatments between 1993 and 1998, a total of 30 deaths were reported to the mental health department between 1993 and 1998. Only one death, which occurred on the same day as the ECT, could be specifically linked to the associated anesthesia. An additional four deaths could plausibly have been associated with the anesthesia, for which the calculated mortality rate is between two and ten per 100,000, but probably not with the stimulus of the ECT or seizure. The mortality rate associated with ECT (less than two per 100,000 treatments) in Texas is extremely low.
Electroconvulsive therapy (ECT) is a safe and effective treatment (1,2). The risk of mortality with ECT and associated anesthesia is about ten times lower than that with childbirth (1) and compares favorably with the risk associated with general anesthesia alone (3).
Since 1993, Texas law has required reporting of all ECT performed in the state, excluding federal jurisdictions (4). Clinical and demographic data are submitted quarterly, including details of any death that occurs within 14 days of ECT. The data, minus any identifying information, are publicly available. The second author has reported statewide data for the first 18 months after the law came into effect, including eight deaths that occurred within 14 days of ECT (2). We report the results of an extension of that study to five years (1993 to 1998), focusing on whether patients' deaths can reasonably be related to ECT.
Methods
We obtained data from the Texas Department of Mental Health and Mental Retardation on the use of ECT and outcomes for all ECT conducted in nonfederal settings for the period of June 1, 1993, to May 31, 1998. For each report of a patient who died within 14 days of receiving ECT, we contacted the treatment site to amplify or clarify the report. Data on mortality after ECT were compared with age-matched data on mortality from all causes in the state of Texas. We also queried the Texas Department of Health, which oversees implementation of and complaints about the reporting law.
Results
Over the study period, 8,148 patients received a total of 49,048 ECT treatments, both series treatments and continuation—or maintenance—treatments. During 1996—a typical year —1,699 patients (or about .94 per 10,000 of the general population) received ECT. These statistics suggest that ECT is used less in Texas than in many other states. The rate of deaths after ECT was not noted to be excessive in 1996 when the data were compared with the overall death rate for the Texas population (data available from the authors).
No deaths occurred during ECT over the five years. Thirty patients, at 18 different sites, died within 14 days of receiving ECT. One of those patients died the same day as the treatment, and seven died within 48 hours of the treatment. Table 1 shows the patients' cause of death, sex, age, time since last treatment, and whether treatment was a series treatment or a maintenance treatment.
Five causes of death were corroborated by autopsy reports, five by death certificates or clinical summaries, and five by separate communications with the facility. The remaining causes of death came solely from the reporting form of the Texas Department of Mental Health and Mental Retardation. The proportion of deaths was not significantly different between public and private facilities.
Discussion and conclusions
Our results are consistent with those of many other studies and reviews. In other studies, the mortality rate associated with properly administered ECT has not been excessive, even among patients of advanced age or compromised cardiovascular or neurologic condition (5,6). The relative risk of death associated with ECT and related procedures such as anesthesia was low in our sample, especially compared with the mortality and morbidity of the illnesses for which the therapy is prescribed.
Any deaths that occurred on the same day as the ECT—one death from laryngospasm—or within 48 hours—two cardiac deaths, three sepsis deaths, one suicide, and one death for which the cause was unknown—are of interest, because they may be related to the ECT and the associated anesthesia. The death due to laryngospasm of a 40-year-old man who required intubation can be considered to be related to anesthesia; the mortality rate associated with anesthesia is two per 100,000 sessions, calculated on the basis of 48,852 sessions.
An additional death on the day after ECT—a 70-year-old woman who died of pneumonitis secondary to inhaled vomitus—may have been indirectly related to the therapy; the mortality rate for this type of death is four per 100,000. If three other deaths—two from myocardial infarction in a 48-year-old man and a 50-year-old woman and one for which the cause was unknown—are included, a mortality rate of ten per 100,000 treatments is obtained. Two more deaths from sepsis were variously attributed to peritonitis following a burst diverticulum in a 51-year-old man who had diverticulitis, confirmed at autopsy, and "overwhelming sepsis with multiple organ failure" in a 79-year-old woman. These two deaths are unlikely to have been related to the ECT.
A conservative estimate of two to ten deaths per 100,000 treatments in a five-year period compares favorably with the 3.3 to 3.7 deaths per 100,000 treatments reported for general anesthesia (7). Ideally, we would have compared our results with age-matched data on mortality from anesthesia, but such information was not available to us.
The most frequent causes of death were cardiac events (ten patients, or 33 percent), none of which occurred during treatment, and suicide (eight patients, or 27 percent). The rate of death from cardiovascular disease and some other causes has been shown to be higher among persons who have severe depression whether or not they receive ECT (8). The two cardiovascular deaths that occurred very soon after ECT in our study could have been related to anesthesia, but the ages of the patients placed them at some risk independent of their treatment. No treatment connection was established, and none should be inferred.
Suicides after ECT may indicate treatment failure and a need for closer and more aggressive care, but one must also consider the severity of the mental illness that is being treated and the time required for this or any other treatment to have positive effects. The rate of mortality from any cause among persons with severe depression—the most frequent diagnosis for which ECT is prescribed—is substantially higher than that in the general population (8). Much of the variance can be accounted for by suicides, which occur at a rate of about 5.5 per 1,000 per year for all persons with untreated depression (9). Bipolar disorder, another illness for which ECT is often considered, has comparable risks.
A recent survey of public-sector psychiatrists in Texas showed that very few refer clinically appropriate patients for ECT. Many of the psychiatrists cited social and political controversy about the treatment—but not clinical doubts—and viewed the state's restrictions and reporting requirements as "repressive" as far as good patient care was concerned (10).
We can find no clinical or scientific justification for reporting deaths that occur up to 14 days after ECT. By assuming that there is some connection between such deaths and the treatment, the current law promotes misrepresentation and misunderstanding of an important medical procedure. Such misunderstanding supports harassment of physicians and hospitals, who are already burdened by administrative hurdles, by those who oppose ECT for political—not clinical—reasons. We believe the current law and its associated attitudes have decreased the availability of this type of therapy to patients who need it.
Acknowledgments
The authors thank Sandy Keller for help in providing the data.
Dr. Shiwach is affiliated with the department of psychiatry at the University of Texas Southwestern Medical Center in Dallas and with Terrell State Hospital, P.O. Box 70, Terrell, Texas 75160 (e-mail, [email protected]). Dr. Reid is with the department of psychiatry at the University of Texas Health Science Center in San Antonio. Dr. Carmody is with academic computing services at the University of Texas Southwestern Medical Center.
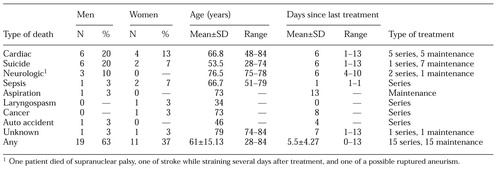 |
Table 1. Characteristics of 30 patients who died within 14 days of electroconvulsive therapy in Texas between June 1, 1993, and May 31, 1998
1. Abrams R: The mortality rate with ECT. Convulsive Therapy 13:125-127, 1997Medline, Google Scholar
2. Reid WH, Keller S, Leatherman M, et al: ECT in Texas:19 months of mandatory reporting. Journal of Clinical Psychiatry 59:8-13, 1998Google Scholar
3. Fink MF: Convulsive Therapy: Theory and Practice. New York, Raven, 1979Google Scholar
4. Texas Health and Safety Code. Section 5.01, subtitle C, title 7, 1993Google Scholar
5. Casey DA, Davis MH: Electroconvulsive therapy in the very old. General Hospital Psychiatry 18:436-439, 1996Crossref, Medline, Google Scholar
6. Zwil AS, Pelchat RJ: ECT in the treatment of patients with neurological and somatic disease. International Journal of Psychiatry and Medicine 24:1-29, 1994Crossref, Medline, Google Scholar
7. Roy CR, Overdyk FJ: The adult patient, in Patient Safety in Anesthetic Practice. Edited by Morell RC, Eichorn JH. St Louis, Churchill Livingstone, 1997Google Scholar
8. Wulsin LR, Vaillant GE, Wells VE: A systematic review of the mortality of depression. Psychosomatic Medicine 61:6-17, 1999Crossref, Medline, Google Scholar
9. Angst J, Angst F, Stassen HH: Suicide risk in patients with major depressive disorder. Journal of Clinical Psychiatry 60(suppl 2):57-62, 1999Medline, Google Scholar
10. Finch JM, Sobin PB, Carmody TJ, et al: A survey of psychiatrists' attitudes toward electroconvulsive therapy. Psychiatric Services 50:264-265, 1999Link, Google Scholar



