A National Survey of Care for Persons With Co-occurring Mental and Substance Use Disorders
Abstract
OBJECTIVE: The delivery of appropriate treatment to persons who have mental and substance use disorders is of increasing concern to clinicians, administrators, and policy makers. This study sought to describe use of appropriate mental health and comprehensive substance abuse care among adults in the United States with probable co-occurring disorders. METHODS: Data from the Healthcare for Communities survey, which is based on a national household sample studied in 1997 and 1998, were used to identify individuals who had probable co-occurring mental and substance use disorders. The sociodemographic and clinical characteristics of these individuals and their use of services were recorded. Logistic regression analysis was used to identify variables associated with receipt of mental health and substance abuse treatment and with receipt of appropriate treatment. RESULTS: Estimates for the U.S. adult population based on the weighted survey data indicated that 3 percent of the population had co-occurring disorders. Seventy-two percent did not receive any specialty mental health or substance abuse treatment in the previous 12 months; only 8 percent received both specialty mental health care and specialty substance abuse treatment. Only 23 percent received appropriate mental health care, and 9 percent received supplemental substance abuse treatment. Perceived need for treatment was strongly associated with receipt of any mental health care and with receipt of appropriate care. CONCLUSIONS: Despite the availability of effective treatments, most individuals who had co-occurring mental health and substance use problems were not receiving effective treatment. Efforts to improve the care provided to persons who have co-occurring disorders should focus on strategies that increase the delivery of effective treatment.
The co-occurrence of mental and substance use disorders, or dual diagnosis, is highly prevalent, and the delivery of appropriate treatment to persons who have dual diagnoses is of increasing concern to clinicians, administrators, and policy makers (1,2,3). Epidemiologic data suggest that of individuals who have a current addictive disorder, almost half have a co-occurring mental disorder; among individuals who have a current mental disorder, between 15 percent and 40 percent have a co-occurring addictive disorder (4,5). Although some of these co-occurring disorders are organic brain syndromes caused by the effects of substance use, the temporal relationships between the disorders and the high proportion of primary lifetime conditions suggest that most of them are primary independent disorders—that is, one did not cause the other (4). This independence implies that most people who have co-occurring disorders will need treatment for both their mental illness and their substance use problems.
Although persons who have dual diagnoses use mental health and substance abuse treatment services more frequently than persons who have only one disorder, most report having received no mental health or substance abuse treatment in the previous year (4,5,6). Among those who seek treatment, the outcomes of substance abuse and mental health treatment are typically worse (7,8,9,10,11,12,13,14,15,16,17)—and treatment costs higher (18,19,20,21)—than among persons who have only one disorder.
There are multiple reasons for poorer treatment outcomes. In addition to the inherent difficulty of treating two problems rather than one, a variety of institutional, attitudinal, and financial factors have been posited as affecting the clinical processes of care, which in turn affect outcomes (22,23,24,25). Substance abuse and mental health treatment programs are funded and managed separately, and coordination of treatment regimens across established bureaucracies has been difficult. The two treatment systems deal with clients in different ways that may conflict or may fail for clients who have multiple problems. Because resources in the public treatment system are scarce, each system tries to exclude individuals who are likely to require more resources, to fail in treatment, or to cause disruption to programs. Thus it has been difficult to respond to the needs of clients with dual diagnoses.
These systemic problems likely influence outcomes by affecting the delivery of appropriate care. However, no studies have used a nationally representative sample to assess the delivery of care to individuals who have co-occurring disorders. It is not known what individual-level factors—such as demographic characteristics, perceived need for treatment, and type of health insurance—affect access to appropriate care or what type of care individuals who have co-occurring disorders receive. Current guidelines recommend that services for individuals who have co-occurring disorders be available regardless of the setting in which the individual enters the service system (26,27). The proportion of individuals who receive parallel or integrated care or who receive care for only one disorder is not known.
This paper describes care among U.S. adults with probable co-occurring disorders. We examined the sociodemographic characteristics, health status, and perceived needs of individuals with co-occurring disorders, stratified by type of mental health disorder. We also looked at patterns of service use, the appropriateness of the mental health care these individuals are receiving, and the comprehensiveness of the substance abuse treatment they are receiving. Finally, we determined factors that predict access to care and the delivery of appropriate mental health or comprehensive substance abuse care.
Methods
Design
We used data drawn from the Healthcare for Communities (HCC) survey. The HCC survey studied a selected subset of adults who participated in the Community Tracking Study (CTS), a nationally representative study of the U.S. civilian, noninstitutionalized population (28). Some demographic data for our analyses came from the parent CTS survey. The CTS included both a national sample and a cluster sample of 60 randomly selected U.S. communities and was conducted in 1996 and 1997. The HCC survey was conducted from October 1997 through December 1998 and consisted of a random sample of 9,585 CTS respondents. The respondents were interviewed by telephone; the average duration of the telephone interviews was 34 minutes.
To provide more precise estimates of the need for and use of behavioral health care, the HCC survey oversampled individuals who had low incomes, had high levels of psychological distress, or used specialty mental health care, as indicated by their responses to the CTS survey. The design of the HCC survey has been described previously (29). We weighted the data so that they would be representative of the U.S. population. We used CTS data to adjust for the probability of selection, nonresponse, and the number of households in the HCC survey that did not have a telephone.
Measures
Independent variables. The short-form Composite International Diagnostic Interview (CIDI) (30) was used to assess the 12-month prevalence of major depression, dysthymia, or generalized anxiety disorder and lifetime mania on the basis of DSM-III-R criteria. Screening items from the CIDI, supplemented by additional items from the full interview, were used to assess for probable panic disorder (31). To reduce the potential number of false-positive responses, we required the presence of a limitation in social or role functioning by using items from the Short Form Health Questionnaire (SF-12) and the Sickness Impact Profile (32). The presence of chronic psychosis was assessed by asking respondents whether they had been hospitalized because of psychotic symptoms or had ever been told that they had schizophrenia or schizoaffective disorder. The Alcohol Use Disorders Identification Test (33) and items adapted from the CIDI were used to assess the presence of substance abuse or dependence within the previous 12 months.
Physical and mental health functioning was assessed with use of the SF-12 mental and physical subscales (34) as well as a count of the number of chronic medical conditions. Type of health insurance was categorized as no insurance, public insurance (Medicaid, Medicare, or both), and private insurance. We also asked the respondents whether they had been on probation or parole or in prison during the previous 12 months.
Outcome variables. Use of health services during the previous 12 months was determined by self-report and was categorized as either primary care with a behavioral health care component or specialty behavioral health care. Primary care with a behavioral health care component consisted of a clinician's suggesting that the respondent reduce his or her use of alcohol or drugs, referring the respondent to specialty behavioral health care, suggesting medication for a substance use or mental health problem, or counseling the respondent for at least five minutes about a mental health or substance use problem. Specialty behavioral health care distinguished between visits for mental health care and visits for substance abuse treatment. Mental health visits included visits to a psychiatrist, a psychologist, a social worker, a psychiatric nurse, or a counselor for an emotional or mental health problem; substance abuse visits included inpatient and outpatient visits for a substance use problem and excluded participation in self-help groups, such as Alcoholics Anonymous.
We defined integrated treatment as receipt of both mental health care and substance abuse care from one provider, which was determined by asking respondents whether they received treatment for both a mental health problem and a substance use problem at a single visit. Parallel treatment was defined as receipt of mental health care and substance abuse care from different providers during a 12-month period.
For persons who had a probable disorder, appropriate care for a bipolar or psychotic disorder was defined as use of any antipsychotic or mood stabilizer during the previous year. Appropriate care for a depressive or anxiety disorder was defined as receipt of appropriate counseling or use of psychotropic medication during the previous year. For counseling to be considered appropriate, the respondent had to have had at least four visits in the previous year, but information on the type of counseling was not recorded. Appropriate medication for a depressive or anxiety disorder was defined as use of an efficacious antidepressant or antianxiety medication for at least two months at a dosage exceeding the minimum recommended dosage, as established by national guidelines (35,36). The relationship between dosage and effectiveness is less clear for antipsychotics and mood stabilizers, and varies according to age, diagnosis, and adverse effects. Thus although respondents were asked about dosages of these medications, the data were not analyzed.
For respondents who had multiple psychiatric disorders, we assessed the appropriateness of care for the most significant disorder on the basis of a hierarchy in which bipolar or psychotic disorder was ranked highest, major depression second, dysthymia third, panic disorder fourth, and generalized anxiety disorder fifth.
We defined comprehensive care for a substance use disorder as consisting of inpatient or outpatient substance abuse treatment that included a physical examination, a mental health evaluation, or job or relationship counseling. The management of medical and mental health problems and the provision of appropriate treatment improve the overall health and functioning of persons who are in recovery (37,38,39), and the provision of job or relationship counseling is likely to be an indicator of programs that provide comprehensive services. The number of services provided is related to treatment retention and to a variety of outcomes (40,41).
Statistical analyses
We used SUDAAN software (42) to estimate individual-level characteristics and to fit multivariate logistic regression models to the data. All estimates were weighted, and standard errors of the multivariate logistic regression estimates were adjusted to account for the complex design of the sample and clustering of individuals within communities.
Separate multiple logistic regressions were used to predict the four dependent variables—receipt of any specialty mental health care, receipt of any substance abuse care, receipt of any appropriate mental health treatment, and receipt of any comprehensive substance abuse treatment. We used the Aday and Andersen (43) model of health services use to select independent variables for inclusion in the models. Predictor variables were selected from each of the three components of this model—predisposing characteristics, enabling resources, and need for treatment—and were included in the model if they were bivariately associated with the dependent variable at a significance level of less than .20.
Because the number of predictors based on the Aday and Andersen model is large relative to the number of observations available for analysis, we were concerned about overfitting in our multivariate logistic regression analyses. To address this concern, we selected a final set of variables for each logistic regression on the basis of a backwards-elimination variable-selection procedure in which a logistic regression coefficient was retained in the final model only if it was significant at p<.10. There was no requirement for any specific variable to be included in the model.
Results
A total of 180 respondents (2 percent) had a probable 12-month depressive or anxiety disorder and a substance use disorder, and 96 respondents (1 percent) had a bipolar or psychotic disorder and a substance use disorder. Table 1 presents the 1998 survey data for respondents with dual diagnoses weighted to reflect the U.S. population, stratified by type of mental illness.
Table 2 presents estimates based on weighted survey data of the types of treatment received by adults with co-occurring mental and substance use disorders in the United States. The estimates indicate that 17 percent received alcohol, drug, or mental health treatment only from a primary care provider, and 23 percent received some treatment from a primary care provider and some from a specialty provider. Seventy-two percent did not receive any specialty mental health or substance abuse treatment in the previous 12 months, and 8 percent received both mental health and substance abuse treatment, either parallel or integrated. Among persons with a probable depressive or anxiety disorder, 32 percent received appropriate treatment; of those with a bipolar or psychotic disorder, 19 percent received an appropriate medication.
Estimates for persons in substance abuse treatment showed that 4 percent received a physical examination, 7 percent received a mental health evaluation or treatment, 2 percent received employment counseling, and 5 percent received some form of relationship or family counseling.
The associations between specific predictor variables and receipt of any mental health care or of any appropriate mental health care for individuals who had a probable co-occurring disorder are shown in Table 3. As we expected, women were more likely than men to have received any mental health care or appropriate mental health care. Having either public or private health insurance was also associated with receipt of mental health care; those with either type of insurance were significantly more likely to receive care than those with no insurance.
Although individuals who had a probable bipolar or psychotic disorder were twice as likely to have received any mental health care as those who had a probable depressive or anxiety disorder, they were less likely to have received appropriate mental health care. Each additional chronic medical condition increased the expected odds of receipt of any appropriate mental health care by 1.2. Perceived need for mental health care was also associated with receipt of care and with receipt of appropriate mental health treatment. Age, race, employment status, income, number of years of education, and physical and emotional functioning were not associated with the receipt of any mental health care or with the receipt of appropriate mental health care.
Table 4 shows the effects of specific predictor variables on receipt of any substance abuse care or any comprehensive substance abuse care among individuals who had a probable co-occurring disorder. Similar to the results shown in Table 3, most predictor variables that we screened for inclusion were not associated with the dependent variables and thus were not included in the final models. Having been on probation or parole or in prison in the previous 12 months was positively associated with receipt of any substance abuse care and with receipt of comprehensive care. Perceived need for substance abuse care was also highly associated with receipt of any care and with receipt of comprehensive treatment. The type of co-occurring disorder was not associated with receipt of any care or of comprehensive care, and neither was sex, race, type of insurance, employment status, income, number of years of education, co-occurrence of medical conditions, or physical or mental health functioning.
Discussion
This study had several limitations. We identified respondents who had probable disorders on the basis of self-reported screening variables and did not confirm the diagnoses with diagnostic interviews. We relied on self-report to identify individuals who had substance use problems. Self-report may result in underestimation of the true prevalence, especially in the case of persons who are using illicit drugs. In addition, the HCC survey is based on a household sample. Many individuals who have severe mental illness and who abuse substances are homeless (44,45,46) or institutionalized (5) and thus would likely have been excluded from the survey.
Our measures of service use and treatment were also limited. Our definitions of service use and appropriate treatment were lenient, and our clinical measures of treatment lacked detail. For individuals who had a probable depressive or anxiety disorder, appropriate mental health treatment consisted of at least four visits during which counseling or appropriate medication at therapeutic dosages was provided; for persons who had a bipolar or psychotic disorder, such treatment consisted of an appropriate medication at any dose. We were unable to determine the content of the counseling visit or whether the counseling was effective. We were also unable to assess whether therapeutic dosages of medication were provided to persons who had probable bipolar or psychotic disorders. Some of the individuals whom we categorized as having received appropriate treatment thus may not in fact have received such treatment. Our measures of comprehensive substance abuse treatment were also broad and consisted of any treatment that included a physical examination, a mental health evaluation or treatment, or job or family counseling. We believe that these are indicators of good-quality care, but we did not evaluate the quality of care directly.
Several million Americans suffer from co-occurring mental health and substance use disorders (3). Our data show that the majority of those in our study had received no mental health or substance abuse treatment in the previous 12 months, confirming the results of earlier studies (4,5). This lack of treatment included both specialty visits and visits to a primary care provider during which behavioral health problems were addressed. In addition, many individuals did not receive care that was consistent with current treatment recommendations. Among the patients who had a probable co-occurring disorder, fewer than a third received appropriate mental health treatment, and only 9 percent received any supplemental substance abuse services. Despite the recommendation that individuals who have co-occurring disorders receive treatment for both their mental health and substance use problems, only 8 percent received either integrated or parallel treatment.
Receipt of mental health care was particularly uncommon among men and among persons who had no health insurance. Among the general population, health insurance status and gender are both important predictors of the use of health care services (47,48). The men in our sample were also less likely to have received appropriate mental health care.
Persons who had a probable bipolar or psychotic disorder were much less likely to have received appropriate mental health treatment than those who had a probable depressive or anxiety disorder. This finding may be related to the introduction of new medications for depression and anxiety that make it easier to treat depressive and anxiety disorders or may have been because our screening instruments captured a number of individuals who did not have a psychotic or bipolar disorder.
Perceived need for treatment was a strong predictor of receipt of mental health and substance abuse care as well as appropriate mental health treatment and comprehensive substance abuse treatment. Although it is possible that a person who receives treatment becomes more aware of his or her need for care, the strong relationship we found suggests that public programs to increase recognition of the need for mental health or substance abuse treatment may be an important strategy for increasing access to effective care. Public education programs may also help to decrease the stigma associated with mental illness (49). Having been on probation or parole or in prison during the previous year was also associated with receipt of any substance abuse treatment and with receipt of comprehensive substance abuse treatment. This finding suggests that the criminal justice system may facilitate access to substance abuse treatment for individuals who have co-occurring disorders.
The low levels of treatment use are of particular concern because of recent studies suggesting that treatment improves a variety of outcomes. Effective treatments exist for depressive, anxiety, and psychotic disorders and have been recommended through national treatment guidelines (35,50-53). Some evidence from clinical trials suggests that treatment of depressive and anxiety disorders among substance abusers is also effective (54,55,56,57,58,59). Studies suggest that for individuals who have chronic or severe mental illness, integrated rather than parallel treatment programs are superior (60).
At a minimum, most experts agree that individuals who have co-occurring disorders should be receiving care for both their mental health and substance use problems (27). Although there is less consensus about what constitutes effective substance abuse treatment, many studies have shown that the management of medical and mental health care problems and the provision of appropriate treatment improve the overall health and functioning of people who are receiving substance abuse treatment (37,38,39). In addition, the number of services provided is related to treatment retention and to a variety of other outcomes (40,41) and is an indicator of good-quality substance abuse treatment.
Conclusions
Despite the availability of effective treatments and treatment models for both mental illness and substance abuse, most persons who have co-occurring disorders are not receiving care. Many of those who do receive care are not receiving effective care. Our findings are particularly worrisome given the broad definitions of appropriate and comprehensive care we used and may explain why individuals with co-occurring disorders have poor treatment outcomes.
Clinicians, administrators, and policy makers can use these results in several ways. Clinicians can recognize that they may not be providing appropriate care and can review their practice patterns to determine whether they can identify individuals with co-occurring disorders who may benefit from more effective treatment. Administrators can address the paucity of substance abuse services provided in mental health treatment programs (61) and the lack of mental health services provided in substance abuse treatment programs (62,63). Policy makers can address the lack of funding for integrated treatment programs for individuals who have serious mental illness and substance use problems. Efforts to improve the quality of care provided to people who have co-occurring disorders should focus on strategies that improve the delivery of effective treatments.
The authors are affiliated with Rand, 1700 Main Street, Santa Monica, California 90407-2138 (e-mail, [email protected]).
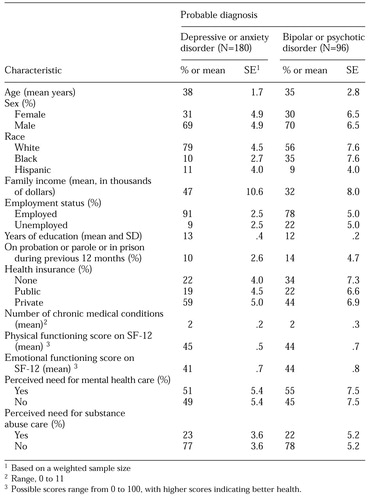 |
Table 1. Estimated percentage of adults with co-occurring mental and substance use disorders in the US. population in 1998 who had the indicated characteristic, by psychiatric diagnosis
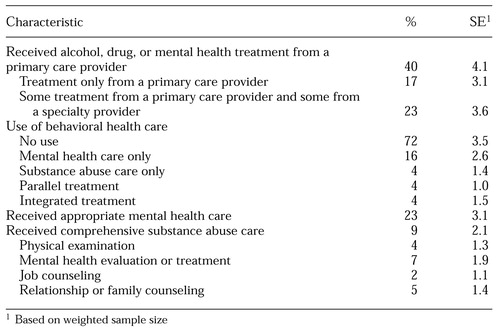 |
Table 2. Estimates of treatment received in 1998 by US. adults with co-occurring mental and substance use disorders
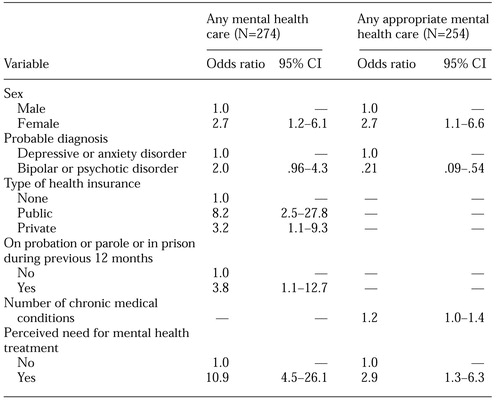 |
Table 3. Predictors of receipt of any mental health care or appropriate mental health care among adults with co-occurring mental and substance use disorders
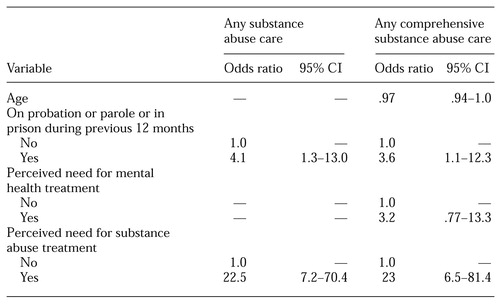 |
Table 4. Predictors of receipt of any substance abuse care or comprehensive substance abuse care among 275 adults with co-occurring mental and substance use disorders
1. National Dialogue on Co-occurring Mental Health and Substance Abuse Disorders. Washington, DC, June 16-17, 1998. Arlington, Va, National Association of State Mental Health Program Directors (NASMHPD) and National Association of State Alcohol and Drug Abuse Directors (NASADAD), 1998Google Scholar
2. Dual Diagnoses: The Challenge of Serving People With Concurrent Mental Illness and Substance Abuse Problems: A Roundtable Discussion. Issue Brief 718. Washington, DC, National Health Policy Forum, Apr 14, 1998Google Scholar
3. National Advisory Council: Improving Services for Individuals at Risk of, or With, Co-occurring Substance-Related and Mental Health Disorders. Rockville, Md, Substance Abuse and Mental Health Services Administration, Jan 1997 (updated 1998)Google Scholar
4. Kessler RC, Nelson CB, McGonagle KA, et al: The epidemiology of co-occurring addictive and mental disorders: implications for prevention and service utilization. American Journal of Orthopsychiatry 66:17-31, 1996Crossref, Medline, Google Scholar
5. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse. JAMA 264:2511-2518, 1990Crossref, Medline, Google Scholar
6. Narrow WE, Regier DA, Rae DS, et al: Use of services by persons with mental and addictive disorders: findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Archives of General Psychiatry 50:95-107, 1993Crossref, Medline, Google Scholar
7. Brown RA, Monti PM, Myers MG, et al: Depression among cocaine abusers in treatment: relation to cocaine and alcohol use and treatment outcome. American Journal of Psychiatry 155:220-225, 1998Abstract, Google Scholar
8. Carroll KM, Power ME, Bryant K, et al: One-year follow-up status of treatment-seeking cocaine abusers: psychopathology and dependence severity as predictors of outcome. Journal of Nervous and Mental Disease 181:71-79, 1993Crossref, Medline, Google Scholar
9. McLellan AT, Luborsky L, Woody GE, et al: Predicting response to alcohol and drug abuse treatments: role of psychiatric severity. Archives of General Psychiatry 40:620-625, 1983Crossref, Medline, Google Scholar
10. Rounsaville BJ, Kosten TR, Weissman MM, et al: Prognostic significance of psychopathology in treated opiate addicts. Archives of General Psychiatry 43:739-745, 1986Crossref, Medline, Google Scholar
11. Rounsaville BJ, Dolinsky ZS, Babor TF, et al: Psychopathology as a predictor of treatment outcome in alcoholics. Archives of General Psychiatry 44:505-513, 1987Crossref, Medline, Google Scholar
12. Platt JJ: Heroin Addiction Theory, Research, and Treatment, vol 2: The Addict, the Treatment Process, and Social Control. Malabar, Fla, Krieger, 1995Google Scholar
13. Bartels SJ, Drake BE, Wallach MA: Long-term course of substance use disorders among patients with severe mental illness. Psychiatric Services 46:248-251, 1995Link, Google Scholar
14. Mueser KT, Drake RE, Miles KM: The course and treatment of substance use disorder in persons with severe mental illness, in Treatment of Drug-Dependent Individuals With Comorbid Mental Disorders. Edited by Onken LS, Blaine JD, Genser S, et al. NIDA Research Monograph 172. Rockville, Md, National Institute of Drug Abuse, 1997Google Scholar
15. Cornelius JR, Salloum IM, Mezzich J, et al: Disproportionate suicidality in patients with comorbid major depression and alcoholism. American Journal of Psychiatry 152:358-364, 1995Link, Google Scholar
16. Osher FC, Drake RE: Reversing a history of unmet needs: approaches to care for persons with co-occurring addictive and mental disorders. American Journal of Orthopsychiatry 66:4-11, 1996Crossref, Medline, Google Scholar
17. Case N: The dual-diagnosis patient in a psychiatric treatment program: a treatment failure. Journal of Substance Abuse Treatment 8:69-73, 991Google Scholar
18. Dickey B, Azeni H: Persons with dual diagnoses of substance abuse and major mental illness: their excess costs of psychiatric care. American Journal of Public Health 86:973-977, 1996Crossref, Medline, Google Scholar
19. Garnick DW, Hendricks AM, Drainoni M: Private sector coverage of people with dual diagnoses. Journal of Mental Health Administration 23:317-328, 1996Crossref, Medline, Google Scholar
20. Hoff RA, Rosenheck RA: The cost of treating substance abuse patients with and without comorbid psychiatric disorders. Psychiatric Services 50:1309-1315, 1999Link, Google Scholar
21. Hoff RA, Rosenheck RA: Long-term patterns of service use and cost among patients with both psychiatric and substance abuse disorders. Medical Care 36:835-843, 1998Crossref, Medline, Google Scholar
22. Ridgely MS, Goldman HH, Willenbring M: Barriers to the care of persons with dual diagnoses: organizational and financing issues. Schizophrenia Bulletin 16:123-132, 1990Crossref, Medline, Google Scholar
23. Howland RH: Barriers to community treatment of patients with dual diagnoses. Hospital and Community Psychiatry 41:1134-1135, 1990Abstract, Google Scholar
24. Pulice RT, Lyman SR, McCormick LL: A study of provider perceptions of individuals with dual disorders. Journal of Mental Health Administration 21:92-99, 1994Crossref, Medline, Google Scholar
25. Rohrer GE, Schonfeld L: The mentally ill substance abuser: challenges for the administrator. Journal of Mental Health Administration 17:217-221, 1990Crossref, Medline, Google Scholar
26. National Dialogue on Co-occurring Mental Health and Substance Abuse Disorders, June 1998. Rockville, Md, Center for Mental Health Services, 1999Google Scholar
27. American Association of Community Psychiatrists: Principles for the Care and Treatment of Persons With Co-occurring Psychiatric and Substance Disorders. Available at http://www.comm.psych.pitt.edu/ finds/dualdx.htmlGoogle Scholar
28. Kemper P, Blumenthal D, Corrigan JM, et al: The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry 33:195-206, 1996Medline, Google Scholar
29. Sturm R, Gresenz C, Sherbourne C, et al: The design of Healthcare for Communities: a study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry 36:221-233, 1999Medline, Google Scholar
30. Kessler RC, Andrews G, Mroczek D, et al: The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). Geneva, World Health Organization, 1998Google Scholar
31. Composite International Diagnostic Interview (CIDI), version 2.1. Geneva, World Health Organization, 1997Google Scholar
32. Bergner M: The Sickness Impact Profile (SIP), in Assessment of Quality of Life in Clinical Trials of Cardiovascular Therapies. Edited by Wenger NK, Mattson ME, Furberg CD, et al. New York, Le Jacq, 1984Google Scholar
33. The Alcohol Use Disorder Identification Test (AUDIT): Guidelines for Use in Primary Health Care. Geneva, Switzerland, World Health Organization, 1992Google Scholar
34. Ware J Jr, Kosinski M, Keller SD: A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Medical Care 34:220-233, 1996Crossref, Medline, Google Scholar
35. Depression Guideline Panel: Depression in Primary Care, vol 2: Treatment of Major Depression. Pub 93-0551. Rockville, Md, Agency for Health Care Policy and Research, 1993Google Scholar
36. Roy-Byrne P, Stein M, Bystrisky A, et al: Pharmacotherapy of panic disorder: proposed guidelines for the family physician. Journal of the American Board of Family Practice 11:282-290, 1998Crossref, Medline, Google Scholar
37. McLellan AT, Hagan TA, Levine M, et al: Supplemental social services improve outcomes in public addiction treatment. Addiction 93:1489-1499, 1998Crossref, Medline, Google Scholar
38. Umbricht-Schneiter A, Ginn DH, Pabst KMM, et al: Providing medical care to methadone clinic patients: referrals vs on-site. American Journal of Public Health 84:207-210, 1994Crossref, Medline, Google Scholar
39. D'Aunno TA: Linking substance abuse treatment and primary health care, in Treating Drug Users Effectively. Edited by Egertson JA, Fox DM, Leshner AI. Malden, Mass, Blackwell, 1997Google Scholar
40. Joe GW, Simpson DD, Hubbard RL: Treatment predictors of tenure in methadone maintenance. Journal of Substance Abuse 3:73-84, 1991Crossref, Medline, Google Scholar
41. McLellan AT, Arndt IO, Metzger DS, et al: The effects of psychosocial services in substance abuse treatment. JAMA 269:1953-1959, 1993Crossref, Medline, Google Scholar
42. SUDAAN: Professional Software for Survey Data Analysis, version 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
43. Aday LA, Andersen RM: A framework for the study of access to medical care. Health Services Research 9:208-220, 1974Medline, Google Scholar
44. Drake RE, Osher FC, Wallach MA: Homelessness and dual diagnosis. American Psychologist 46:1149-1158, 1991Crossref, Medline, Google Scholar
45. Susser E, Betne P, Valencia E, et al: Injection drug use among homeless adults with severe mental illness. American Journal of Public Health 87:854-856, 1997Crossref, Medline, Google Scholar
46. Dennis ML, Bray RB, Lachan R, et al: Drug use and homelessness, in Drug Use in Metropolitan America. Edited by Bray RM, Marsden ME. Thousand Oaks, Calif, Sage, 1999Google Scholar
47. Berk ML, Schur CL: Measuring access to care: improving information for policymakers. Health Affairs 17(1):180-186, 1998Google Scholar
48. Health, United States, 1990. Pub (PHS) 91-1232. Washington, DC, National Center for Health Statistics, 1991Google Scholar
49. Link BG, Phelan JC, Bresnahan M, et al: Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American Journal of Public Health 89:1328-1333, 1999Crossref, Medline, Google Scholar
50. Depression Guidelines Panel: Depression in Primary Care, vol 1: Detection and Diagnosis. Pub 93-0550. Rockville, Md, Agency for Health Care Policy and Research, 1993Google Scholar
51. Van Balkom AJLM, Bakker A, Spinhoven P, et al: A meta-analysis of the treatment of panic disorder with or without agoraphobia: a comparison of psychopharmacological, cognitive-behavioral, and combination treatments. Journal of Nervous and Mental Disease 185:510-516, 1997Crossref, Medline, Google Scholar
52. Gould RA, Otto MW, Pollack MH: Cognitive behavioral and pharmacological treatment of generalized anxiety disorder: a preliminary meta-analysis. Behavior Therapy 28:285-305, 1997Crossref, Google Scholar
53. American Psychiatric Association Practice guideline for the treatment of patients with panic disorder. American Journal of Psychiatry 155(May suppl):1-34, 1998Google Scholar
54. Nunes EV, Quitkin FM: Treatment of depression in drug-dependent patients: effects on mood and drug use, in Treatment of Drug-Dependent Individuals With Comorbid Mental Disorders. Edited by Onken LS, Blaine JD, Genser S, et al. NIDA Research Monograph 172. Rockville, Md, National Institute of Drug Abuse, 1997Google Scholar
55. Mason BJ, Kocsis JH, Ritvo EC, et al: A double-blind, placebo-controlled trial of desipramine for primary alcohol dependence stratified on the presence or absence of major depression. JAMA 275:761-767, 1996Crossref, Medline, Google Scholar
56. Nunes EV, Quitkin FM, Donovan SJ, et al: Imipramine treatment of opiate-dependent patients with depressive disorders. Archives of General Psychiatry 55:153-160, 1998Crossref, Medline, Google Scholar
57. Cornelius JR, Salloum IM, Hasket RF, et al: Fluoxetine versus placebo for the marijuana use of depressed alcoholics. Addictive Behaviors 24:111-114, 1999Crossref, Medline, Google Scholar
58. Barlow DH: Anxiety disorders, comorbid substance abuse, and benzodiazepine discontinuation: implications for treatment, in Treatment of Drug-Dependent Individuals With Comorbid Mental Disorders. Edited by Onken LS, Blaine JD, Genser S, et al. NIDA Research Monograph 172. Rockville, Md, National Institute of Drug Abuse, 1997Google Scholar
59. McGrath PJ, Nunes EV, Stewart JV, et al: Imipramine treatment of alcoholics with primary depression. Archives of General Psychiatry 53:232-240, 1996Crossref, Medline, Google Scholar
60. Drake RE, Mercer-McFadden C, Mueser KT, et al: Review of integrated mental health and substance abuse treatment for patients with dual disorders. Schizophrenia Bulletin 24:589-608, 1998Crossref, Medline, Google Scholar
61. Young NK, Grella CE: Mental health and substance abuse treatment services for dually diagnosed clients: results of a statewide survey of county administrators. Journal of Behavioral Health Services and Research 25:83-92, 1998Crossref, Medline, Google Scholar
62. Friedmann PD, Alexander JA, Jin L, et al: On-site primary care and mental health services in outpatient drug abuse treatment units. Journal of Behavioral Health Services and Research 26:80-94, 1999Crossref, Medline, Google Scholar
63. Grella CE, Hser Y-H: A county survey of mental health services in drug treatment programs. Psychiatric Services 48:950-952, 1997Link, Google Scholar



