Variations in Utilization and Cost of Inpatient Psychiatric Services Among Adults in Maryland
Abstract
The author examined variations in the clinical characteristics, costs, utilization, and discharge patterns of adult inpatients who were hospitalized for psychiatric disorders in Maryland state general hospitals in 1998. Administrative discharge data on all 30,121 adult psychiatric patients in the state in 1998 were used to calculate descriptive statistics on elderly (age 65 years and over) and nonelderly (age 19 to 64 years) patients. The most common reasons for hospitalization were substance-related disorders, which affected 25 percent of the patients, and major depressive disorders, which affected 24.6 percent of the patients. After the effects of Medicare's prospective payment system were disregarded, the average cost of treating elderly persons for depression was calculated to be around 80 percent higher than national estimates.
More than 20 years ago, Mechanic (1) recognized the need for health services researchers to produce large, comprehensive cost studies of psychiatric disorders as well as smaller, more detailed studies to better address the needs of public policy. Although national and provider- or payer-specific cost estimates are well covered in the literature on the cost of mental health care (2,3,4,5), little is known about variations in state and local government costs of treating psychiatric disorders. Most national-level studies have used data collected more than ten years ago, and few of these studies addressed variations in the cost and utilization of mental health services between elderly and nonelderly adults at the state level.
This study contributes to the literature by addressing two issues. First, because of the role of state and local governments in financing mental health services (4), the study examined variations in cost and length of stay in subpopulations in the only remaining state that is not subject to Medicare's prospective payment system—Maryland. Second, given the considerable concern among policy makers and others about access to mental health services among uninsured persons, it seemed useful to explore variations in length of stay in populations with public insurance, private insurance, and no insurance.
Maryland has a federal waiver that requires Medicare to pay hospitals according to state rules. In fact, Maryland's hospital rate-setting system is referred to as an all-payer system because all third-party payers—health maintenance organizations, Medicare, Medicaid, and other insurers—are subject to the same rates for hospital care. These rates vary by hospital and type of service. As a result, it is expected that all Maryland citizens will be provided with access to hospital care for both physical and mental disorders. The goal of this study was to describe and compare the use of mental health services between elderly and nonelderly adults treated in general hospitals in Maryland. The study addressed the question of whether costs, lengths of stay, and discharge destinations varied between these two groups.
Methods
Hospital discharge data were obtained from the Maryland Health Services Cost Review Commission for all patients admitted to Maryland hospitals during the calendar year 1998 with a principal diagnosis indicating a psychiatric disorder. Hospitalizations for psychiatric disorders were defined as those involving a primary ICD-9-CM diagnosis in the range of codes 290 to 319. Psychiatric disorders were aggregated into ten categories: schizophrenic disorder, other psychotic disorder, bipolar disorder, major depressive disorder, other depressive disorder, anxiety disorder, dementia, organic disorder other than dementia, substance-related disorder, and all other disorders.
Aggregate statistics on psychiatric hospitalizations and inpatient costs were based on all 1998 Maryland inpatient admissions to general hospitals of adult patients who had a primary psychiatric diagnosis. First, psychiatric inpatient admission rates and the associated costs were computed. Next, the distribution of primary diagnosis by the age group of the patients—65 years or older (elderly) and 19 to 64 years (nonelderly) was compiled. Finally, average cost, average length of stay, and whether the patient was discharged to home care or to an institution were examined according to primary diagnosis.
Because the data used in this study were from the entire population rather than from a sample, statistical tests were not strictly necessary; however, they were performed nevertheless. Chi square and t tests showed that all differences across subgroups were statistically significant (p<.001).
Results
During 1998 a total of 31,121 adult patients were hospitalized because of a primary psychiatric diagnosis. The mean±SD age of these patients was 39±15.2 years. Fifty-two percent of the patients were male, and 58 percent were white. The mean±SD length of stay for a person hospitalized for a psychiatric disorder was 6.1±6.5 days, and the mean±SD cost was $5,034±$5,055. This cost is consistent with those reported in other studies of average Medicare payments for hospitalized elderly persons with psychiatric disorders (2,5).
Table 1 shows the distribution of primary diagnoses of patients in each age group. For both age groups combined, the most common diagnoses coded as the reason for hospitalization were substance-related disorders, affecting 25 percent of patients; major depressive disorder, affecting 24.6 percent; bipolar disorder, affecting 11.9 percent; and schizophrenic disorder, affecting 16 percent. Major depressive and substance-related disorders accounted for more than half of the inpatient stays.
The prevalence of dementia was higher among elderly than among nonelderly patients. Nearly 25 percent of the elderly patients were treated for a primary diagnosis of dementia or other organic disorder. The greater frequency of organic disorders among the elderly was often accompanied by a lower frequency of the other diagnoses. A few notable exceptions were the higher frequencies of psychotic disorders other than schizophrenia, and anxiety disorders among elderly patients.
Table 1 also shows average costs, lengths of stay, and discharge destinations by primary diagnosis. Average lengths of stay varied substantially across subgroups, from a low of 3.1 days for substance-related disorders among nonelderly patients to a high of 13.8 days for schizophrenic disorders among elderly patients.
Costs were consistently highest for elderly patients who were treated for major depressive disorder, bipolar disorder, or schizophrenic disorder. The cost of treating elderly patients for these disorders was nearly $11,000. A possible explanation for this finding is the higher rate of comorbidity among elderly patients with a primary psychiatric diagnosis admitted to general hospitals in Maryland.
When the effects of Medicare's prospective payment system were disregarded, the average cost of treating elderly patients for depression in general hospitals was $10,920.
The average costs and average lengths of stay were consistently higher for patients covered by public insurance programs, such as Medicare and Medicaid, than for patients with private or no insurance. One possible explanation for these differences is that elderly patients are more likely to be covered by such programs and, because they have more comorbidity, are more expensive to treat. On average, uninsured patients were charged less and had shorter hospital stays than insured patients.
The highest rates of discharge to home care were found among nonelderly patients who were hospitalized for major depressive disorders, anxiety disorders, other depressive disorders, bipolar disorder, or schizophrenic disorder. Elderly patients with dementia and other organic disorders were less likely to be discharged to home care than nonelderly patients, probably because of their inability to care for themselves adequately.
Discussion and conclusion
In the entire population of adults who were treated for psychiatric disorders in Maryland in 1998, the average length of general hospital stay was 6.1 days and the average cost per stay was $4,944. About two-thirds of the hospital stays ended with the patient's being discharged to home care.
Although previous studies (2,5) reported that the average cost of inpatient care for elderly Medicare beneficiaries who were hospitalized in general hospitals for depression was around $6,000, our study showed that when the effects of Medicare's prospective payment system were disregarded, the average cost of treating elderly patients for depression in general hospitals was $10,920, around 80 percent higher than national estimates.
Elderly patients were treated in general hospitals in Maryland for major depression at nearly the same rate as nonelderly patients. However, the average cost of treating the elderly patients was 2.3 times higher and the average length of stay nearly eight days longer than those of the nonelderly patients. This finding suggests that, independent of the effects of insurance coverage, particularly the effect of Medicare's prospective payment system, elderly patients are underutilizing mental health services for depression because they are delaying treatment until they become more severely ill and more expensive to treat.
Dr. Brown is assistant professor of public administration at the Martin School of Public Policy and Administration at the University of Kentucky, 431 Patterson Office Tower, Lexington, Kentucky 40506-0027 (e-mail, [email protected]).
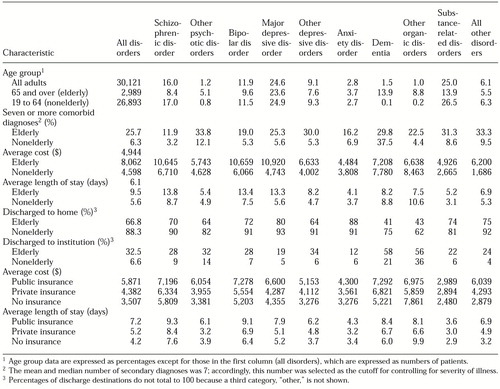 |
Table 1. Distribution of psychiatric diagnoses among all adult inpatients in Maryland state general hospitals in 1998 by age group, number of comorbid diagnoses, cost, length of stay, discharge destination, and type of insurance
1. Mechanic D: Correlates of physician utlilization: why do major multivariate studies of physician utilization find trivial psychosocial and organizational effects? Journal of Health and Social Behavior 20:387-396, 1979Google Scholar
2. Ettner SL, Hermann RC: Inpatient psychiatric treatment of elderly Medicare beneficiaries. Psychiatric Services 49:1173-1179, 1998Link, Google Scholar
3. Druss BG, Rosenheck RA: Patterns of health care costs associated with depression and substance abuse in a national sample. Psychiatric Services 50:214-218, 1999Link, Google Scholar
4. Mental Health: A Report of the Surgeon General. Washington, DC, US Department of Health and Human Services, 1999Google Scholar
5. Cano C, Hennessy KD, Warren JL, et al: Medicare part A utilization and expenditures for psychiatric services:1995. Health Care Financing Review 18:177-193, 1997Google Scholar



