Factors Associated With Use of Mental Health Services for Depression by Children and Adolescents
Abstract
OBJECTIVE: This study examined patterns of mental health service use among depressed children and adolescents and factors associated with help seeking and treatment modalities. METHODS: The sample consisted of 206 children and adolescents aged 9 to 17 years who were assessed as part of a larger survey of mental health service use in five service systems and in the community and who met DSM-III-R criteria for depressive disorders (major depression or dysthymia). RESULTS: Among the 206 children, 75 (36 percent) never received professional help for depressive symptoms. Among the 131 children who received professional help for depression, antidepressants were prescribed for 40 (31 percent) in the year before the interview. The findings indicate possible undertreatment of depression among children and adolescents, especially among African Americans. Socioeconomic factors, such as the mother's education and the child's health insurance, were not associated with receiving professional help for depressive symptoms but were associated with receiving antidepressants. Parental perception of a child's mental health service need was associated with receiving professional help but not with receiving antidepressants. Also, depressed children were more likely to receive antidepressants when they had life-threatening or severe symptoms, such as a suicide attempt or drug abuse. CONCLUSIONS: Whether a depressed child receives mental health services and the types of treatment received are influenced by different individual and family factors and by the type of symptoms exhibited. Better understanding of these factors will help in meeting the service needs of depressed children and adolescents.
National studies have indicated increasing rates of depression and a shift to a younger age of onset (1,2,3,4). Depression is one of the leading risk factors for suicide among children and adolescents (5,6).
The Epidemiologic Catchment Area study (7) found that about one-third of adults who suffered from a major depressive disorder had not sought treatment. In a review of studies of adult depression, Hirshfeld and associates (8) found serious undertreatment of persons with depression, even though effective treatments have been available for several decades. They concluded that patient-associated reasons for undertreatment include failure to recognize symptoms, limited access to services, lack of insurance, fear of being stigmatized, and noncompliance with treatment. A further conclusion was that inadequate training of health care providers and barriers created by mental health care delivery systems also contribute to undertreatment. The cost to individuals, families, and society of undertreatment is substantial (8,9,10).
The situation of children who need mental health services is no different from that of adults: many children receive inappropriate services (11) or no services at all (12,13,14). Children with depressive disorders are less likely to receive mental health services than children with disruptive disorders (15,16,17).
Individual characteristics found to affect child mental health service utilization include the child's age (18,19,20), gender (18,20,21,22), ethnicity (19,20,21,23), physical illness (24), and level of functioning (17,25,26). Family characteristics include socioeconomic status (19,22,24) and the parents' use of mental health services (22), their perception of the child's need for mental health services and whether the need was met (17), and their perceived burden (27). All these factors, with the exception of perceived parental burden, were taken into account in this study.
Most studies of child and adolescent mental health service need and service use have not examined the association between service use and specific psychiatric disorders. Little is known about the factors that affect mental health service use for depression or the types of treatment received by children with depression. In this context, our study addressed three questions: What are the factors associated with receiving professional help for childhood depression? What are the factors associated with receiving antidepressants for depression? Are there shared and unique factors associated with receiving professional help and receiving antidepressants?
Methods
Sample and data
Our analysis used data from a group of 206 children and adolescents aged 9 to 17 years who met DSM-III-R criteria for depressive disorders (major depression or dysthymic disorder). This group is a subsample of a survey of mental health service need and service utilization among children and adolescents from nonresidential child service systems and the community in Westchester County, New York (28). The group comprises all the subjects in the Westchester study who met criteria for depressive disorders.
The Westchester study included 763 children and adolescents randomly selected from five child service systems: mental health, substance use, child welfare, special education, and probation. The study also included 533 children and adolescents recruited from the community, including 360 children from the Westchester site of the Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) study by the National Institute of Mental Health (NIMH) (29,30,31,32), selected from the same sampling frame and assessed with identical measures of child psychopathology, impairment, and service use.
The child and one parent or guardian in each household were interviewed for approximately three hours by trained interviewers about childhood psychopathology, mental health service use, and a wide array of risk factors (29,32).
Measures of psychopathology and impairment
Depression and other mental disorders. Children's depression and other mental disorders in the six months preceding the interview were assessed by the NIMH Diagnostic Interview Schedule for Children (DISC) (DSM-III-R) or DISC 2.3 (30). The validity and reliability of the measures have been reported elsewhere (30,31). A diagnostic criterion was considered to be positive if reported by either the parent or the child (30). Depressive disorders included major depression and dysthymia. The number of depressive symptoms was also included in the analysis as an indicator of severity. Other mental disorders included anxiety disorders, disruptive disorders, and substance use disorders.
Impairment. Impairment was measured by the Child Global Assessment Scale (CGAS). The CGAS scores range from 1 to 100, with a lower score representing greater impairment. The interviewer's rating, based on the parent interview with satisfactory validity, was used (25).
Service use and perceived need
Child mental health service use for depression. Specific questions about service use for depression, including treatment and medications received, were asked for children who met the NIMH-DISC criteria for depression (30). As with the DISC diagnoses, treatment information from the parent and the child was aggregated. In addition, in the non-DISC service use section, the parent and child were asked about the child's treatments and medications for emotional, behavioral, and drug problems. We used two variables in our analysis: whether the child had ever been seen by a health professional—psychiatrist, psychologist, physician, social worker, or guidance counselor —for depressive symptoms, and whether the child used an antidepressant in the previous year.
Parental perception of a child's service needs and unmet needs. Parents were asked if they believed their children needed any mental health service (perceived need) and whether any had been received. A perception of unmet need was recorded if a parent reported that a child's need for services was not met. This measure is imprecise, however, because a child could have been receiving services but the parent may still have believed that the need had not been met.
Maternal mental health service use. We used two variables in the parent interview: whether the biological mother had ever been seen by any mental health professional for a psychological or emotional problem, and whether the biological mother ever took any medication for a psychological or emotional problem.
Sociodemographic factors
Data on each child's gender, age, race or ethnicity, household income, maternal education, and health insurance status were used in the analyses. Health insurance status was classified as no insurance, Medicaid, or private insurance (which included all non-Medicaid health insurance).
Analysis
We were mainly interested in two binary dependent variables: whether the depressed children had received professional help for depression, and whether those who received professional help received antidepressants. A univariate analysis was first conducted to compare sociodemographic characteristics, other psychiatric disorders, and other factors of depressed children who received professional help with those who never received any professional help for depression. Among those who received professional help, univariate analysis was used to compare those who received antidepressants with those who did not. A chi square test was used for categorical variables, and a t test was used for continuous variables.
Multiple logistic regression analysis was used to identify factors that affected mental health service use for depression among all depressed children. For those who received help, the same method was used to identify the factors differentiating those who were taking antidepressants from those who were not.
The two dependent variables—receipt of professional help and receipt of antidepressants—correspond to the two dichotomies of the service use hierarchy; the comparison for antidepressant treatment was nested within the comparison for getting professional help. Therefore, in the last stage of our analysis, we used a nested response model (33) to examine whether the factors affecting receipt of professional help for depression were the same as those affecting receipt of antidepressants. The model was tested using the SAS generalized linear models (GENMOD) procedure (34).
Results
Sample description
Of the 206 depressed children and adolescents, 116 (56 percent) were girls, 82 (40 percent) were white, 71 (35 percent) were African American, 38 (18 percent) were Hispanic, and 15 (7 percent) were other. The mean age±SD was 14.4±2.3 years. Thirty-nine children in the community sample (7.3 percent) and 167 children in the child service systems sample (21.9 percent) were depressed.
Comparisons of demographic and socioeconomic characteristics of depressed children from the community with those from the service systems show that depressed children from the service systems were more likely to be boys, to be ethnic minorities, to be from disadvantaged families with a low income, and to be on Medicaid (data not shown). These notable differences between the children from the community and those from service systems were anticipated. In the subsequent multivariate analyses, a dummy variable—services versus community—was included to control for differences in the community and service systems samples.
Univariate analyses
Of the 206 depressed children, 131 (64 percent) received professional help; 75 (36 percent) did not seek professional help for depressive symptoms. Table 1 shows the family and individual characteristics of depressed children who received professional help compared with those who did not. African-American youth were less likely to receive professional help than those from other ethnic groups. As expected, depressed children who received professional help were more likely to have a greater number of depressive symptoms and more impairment than those who did not receive such help. Mothers of depressed children who received professional help reported greater use of mental health services and medication for their own psychiatric problems and were more likely to think that their children needed mental health services than mothers of depressed children who did not receive help.
Among the 131 children who received professional help, antidepressants were prescribed for 40 (31 percent) in the year before the interview. As Table 1 shows, children who received antidepressants were significantly more likely than children who did not to be white, to have a mother who had received professional help and antidepressants, and to be more impaired. Families of children who received antidepressants also had a higher average income and a higher level of maternal education and were more likely to have private insurance. Children who received antidepressants were also more likely to meet criteria for substance abuse disorders and to have recently attempted suicide.
Multivariate Analyses
Table 2 shows the results of two logistic regression analyses. Because the results shown in Table 1 indicated that the major ethnic difference was between African Americans and other ethnic groups, African Americans were compared with all other ethnic groups in the logistic regression analysis. Table 2 shows the adjusted odds ratios and confidence intervals for the analysis comparing depressed children who received professional help with those who never received any help and for the analysis comparing those who received antidepressants with those who did not.
As shown in Table 2, children who received professional help for depression were significantly less likely to be African American, had more depressive symptoms, and were more impaired. Their parents were also more likely to report that the child needed mental health services and were less likely to report unmet need. Girls tended to receive professional help more often than boys, and children with disruptive disorders were less likely than other depressed children to receive treatment for depression.
Among children who received professional help, factors significantly associated with receiving antidepressants included being male, a higher level of maternal education, comorbid substance use disorders, a recent suicide attempt, and greater impairment. Children from families with private health insurance tended to receive antidepressants more often than those from families with no insurance.
As discussed above, we were interested in identifying factors that affected whether children received professional help for depression and that influenced whether antidepressant medication was prescribed for those who received help. In addition, we wanted to identify shared and unique factors associated with receiving professional help and antidepressants. Because the comparison of children who received antidepressants was nested within the comparison of children who received professional help, the model of nested responses (33) was applied to the data.
We identified four factors with differential impact on the receipt of professional help for childhood depression compared with the use of antidepressants among those receiving professional help. Girls were more likely to receive professional help for depression; however, among all those who received help, boys were more likely to receive antidepressants (p<.01). Also, the mother's education and the child's comorbid substance use disorders and previous suicide attempt were significantly related to antidepressant treatment (p<.05) but not to receiving professional help for depression.
Discussion and conclusions
Most studies of child mental health service use have not examined service use in terms of a specific disorder. The study reported here assessed child mental health service use for depression and compared factors affecting the use of professional help and treatment with antidepressants for childhood depression.
Consistent with findings of studies of adults (7,8), depression appears to be undertreated among children and adolescents, especially among African Americans (21,35,36). However, it has been suggested that African-American youth more frequently seek help for psychological symptoms from nonprofessional domains such as church and family before seeking formal mental health services than do whites (37). Further research in this area is needed.
After the analysis controlled for other possible confounding factors, depressed girls appeared to be somewhat more likely to receive professional help for depression than boys. This gender difference is consistent with that found among adults (38,39). However, among children who received professional help for depression, boys were more likely to receive antidepressants. These findings suggest that the gender effect may differ by types of service and treatment. More studies are needed to replicate these findings.
Family socioeconomic characteristics did not appear to be significant factors in whether children received professional help, but they did play an important role in whether antidepressants were prescribed. Children who received antidepressants were more likely to come from families of higher socioeconomic status. Although the association with income disappeared in the multivariate analyses, the mother's education remained a significant predictor, suggesting that parental knowledge of depression and of available medications for treatment may influence the type of services received.
Like other studies (40,41), our findings did not show a correlation between having insurance and receiving professional help for depression. However, among children receiving such help, those with private insurance tended to be somewhat more likely to receive antidepressants than those with no insurance. These findings suggest that studies examining mental health service use without simultaneously exploring the type of treatment received may not reveal— and may consequently underestimate—the impact of having health insurance. The impact of insurance on different types of treatment for depression and possibly other disorders should be explored.
Consistent with previous studies (26,40), our results indicate that level of impairment and severity of depression (number of depressive symptoms) were related to receiving mental health services. The occurrence of other disorders did not appear to be related to a child's receiving professional help for depression. However, among children who received such help, those who received antidepressants were more likely to have a comorbid substance use disorder and to have had a previous suicide attempt. This finding is consistent with previous studies (1) and suggests that children with depression are more likely to receive antidepressants if they have some life-threatening or severe symptoms, such as a suicide attempt and drug abuse.
In summary, our findings suggest that parental failure to recognize depressive symptoms, lack of knowledge about depression and its related treatment, and lack of adequate health insurance may all influence whether or not a child receives services as well as the type of treatment received. Mental health education should be offered to parents to improve early identification and treatment of depressed children and adolescents.
A limitation of this study is that the information on treatment for depression was limited, as we did not have a measure of psychotherapy. Consequently, the children who did not receive antidepressant treatment could have received anything from a single evaluation to a full range of treatment without antidepressants. It is also possible that some depressed children who received antidepressants had previously received another type of treatment. Therefore, we do not mean to imply that children who received antidepressants got better service than those who did not.
In fact, the literature indicates that although both psychotherapy and pharmacotherapy have been found to be beneficial for depressive disorders, children do not seem to respond to antidepressants as well as adults do (1,42,43,44,45). Psychotherapy has been recommended as the first treatment for most depressed youth, with antidepressants considered only for those with more severe depression, bipolar disorder, and depression with psychotic features and those who do not respond to psychotherapeutic intervention (1). Future research, including detailed treatment information, is needed.
Finally, because of the low prevalence of depression, data from our community and service systems samples were combined to increase the power of the analysis. Although sample differences were statistically controlled and detailed analyses were conducted to ensure that our findings were not due to sample differences, a large-scale study is needed to replicate these findings.
Acknowledgments
Work on this paper was partly supported by a grant to Dr. Wu from the National Alliance for Research on Schizophrenia and Depression, by National Institute for Mental Health (NIMH) research training grant MH-13043 in psychiatric epidemiology, and by NIMH grant MH-469091 (Dr. Hoven, principal investigator). The authors thank Cordelia Fuller for her assistance in analyzing the data.
The authors are affiliated with the department of child and adolescent psychiatry at the New York State Psychiatric Institute, 1051 Riverside Drive, Unit 43, New York, New York 10032 (e-mail, [email protected]).
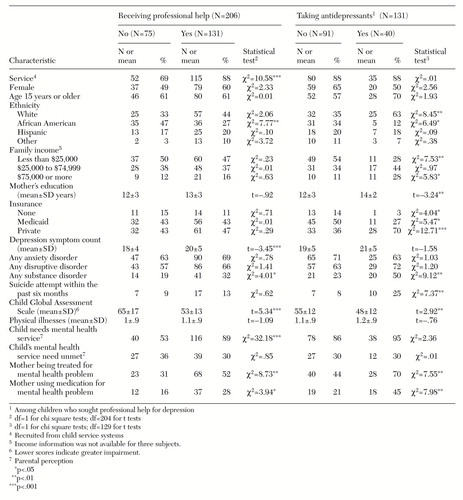 |
Table 1. Family and individual characteristics of children with depression by whether they received professional help and used antidepressants
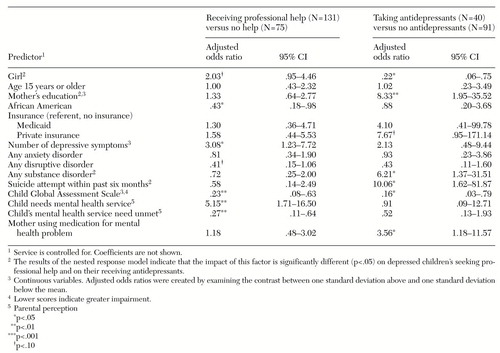 |
Table 2. Logistic regression analyses predicting receipt of professional help and receipt of antidepressants among children with depression
1. American Academy of Child and Adolescent Psychiatry: practice parameters for the assessment and treatment of children and adolescents with depressive disorders. Journal of the American Academy of Child and Adolescent Psychiatry 37(suppl):63S-83S, 1998Google Scholar
2. Burke KC, Burke JD, Rae DS, et al: Comparing age at onset of major depression and other psychiatric disorders by birth cohorts in five US community populations. Archives of General Psychiatry 48:789-795, 1991Crossref, Medline, Google Scholar
3. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
4. Weissman MM, Klerman GL: Depression: current understanding and changing trends. Annual Review of Public Health 13:319-339, 1992Crossref, Medline, Google Scholar
5. Brent D, Perper J, Moritz G, et al: Psychiatric risk factors for adolescent suicide: a case-control study. Journal of the American Academy of Child and Adolescent Psychiatry 32:11-16, 1993Google Scholar
6. Shaffer D, Gould MS, Fisher P, et al: Psychiatric diagnosis in child and adolescent suicide. Archives of General Psychiatry 53:339-348, 1996Crossref, Medline, Google Scholar
7. Robins LN, Regier DA: Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, Free Press, 1991Google Scholar
8. Hirschfeld RMA, Keller MB, Panico S, et al: The National Depressive and Manic-Depressive Association consensus statement on the undertreatment of depression. JAMA 277:333-340, 1997Crossref, Medline, Google Scholar
9. Keller MB, Harrison W, Fawcett JA, et al: Treatment of chronic depression with sertraline and imipramine: preliminary blinded response rates and high rates of undertreatment in the community. Psychopharmacology Bulletin 31:205-212, 1995Medline, Google Scholar
10. Rice DP, Miller LS: The economic burden of affective disorders. British Journal of Psychiatry 166:34-42, 1995Crossref, Google Scholar
11. Saxe L, Cross T, Silverman N: Children's mental health: the gap between what we know and what we do. American Psychologist 43:800-807, 1988Crossref, Medline, Google Scholar
12. Burns B: Mental health service use by adolescents in the 1970s and 1980s. Journal of the American Academy of Child and Adolescent Psychiatry 30:144-150, 1991Crossref, Medline, Google Scholar
13. Burns B, Costello EJ, Angold A, et al: Children's mental health service use across service sectors. Health Affairs 14:147-159, 1995Crossref, Medline, Google Scholar
14. Whitaker A, Johnson J, Shaffer D, et al: Uncommon troubles in young people: prevalence estimates of selected psychiatric disorders in a nonreferred adolescent population. Archives of General Psychiatry 47:487-496, 1990Crossref, Medline, Google Scholar
15. Anderson JC, Williams S, McGee R, et al: DSM-III disorders in preadolescent children: prevalence in a large sample from the general population. Archives of General Psychiatry 44:69-76, 1987Crossref, Medline, Google Scholar
16. Cohen P, Kasen S, Brook JS, et al: Diagnostic predictors of treatment patterns in a cohort of adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 30:989-993, 1991Crossref, Medline, Google Scholar
17. Wu P, Hoven CW, Bird HR, et al: Depressive and disruptive disorders and mental health service utilization in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 38:1081-1090, 1999Crossref, Medline, Google Scholar
18. Barber CC, Rosenblatt A, Harris L, et al: Use of mental health services among severely emotionally disturbed children and adolescents in San Francisco. Journal of Child and Family Studies 1:183-207, 1992Crossref, Google Scholar
19. Cohen P, Hesselbart CS: Demographic factors in the use of children's mental health services. American Journal of Public Health 83:49-52, 1993Crossref, Medline, Google Scholar
20. Zahner GEP, Daskalakis MS: Factors associated with mental health, general health, and school-based service use for child psychopathology. American Journal of Public Health 87:1440-1448, 1997Crossref, Medline, Google Scholar
21. Cuffe SP, Waller JL, Cuccaro ML, et al: Race and gender differences in the treatment of psychiatric disorders in young adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 34:1536-1543, 1995Crossref, Medline, Google Scholar
22. Garralda ME, Bailey D: Child and family factors associated with referral to child psychiatrists. British Journal of Psychiatry 153:81-89, 1988Crossref, Medline, Google Scholar
23. Neighbors HW, Bashshur R, Price R, et al: Ethnic minority mental health service delivery: a review of the literature. Research in Community and Mental Health 7:55-71, 1992Google Scholar
24. John LH, Offord DR, Boyle MH, et al: Factors predicting use of mental health and social services by children 6-16 years old: findings from Ontario Child Health Study. American Journal of Orthopsychiatry 65:76-86, 1995Crossref, Medline, Google Scholar
25. Bird HR, Schwab-Stone M, Andrews H, et al: Global measures of impairment for epidemiologic and clinical use with children and adolescents. International Journal of Methods in Psychiatric Research 6:295-307, 1996Crossref, Google Scholar
26. Leaf PJ, Alegria M, Cohen P, et al: Mental health service use in the community and schools: results from the four community MECA study. Journal of the American Academy of Child and Adolescent Psychiatry 35:889-897, 1996Crossref, Medline, Google Scholar
27. Angold A, Messer SC, Stangl D, et al: Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health 88:75-80, 1998Crossref, Medline, Google Scholar
28. Hoven CW, Cohen P, Moore RE, et al: Multi-service system involvement of emotionally disturbed youth. Presented at the annual meeting of the American Public Health Association, Washington, DC, Nov 17-19, 1998Google Scholar
29. Lahey BB, Flagg EW, Bird HR, et al: The NIMH Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) study: background and methodology. Journal of the American Academy of Child and Adolescent Psychiatry 35:855-864, 1996Crossref, Medline, Google Scholar
30. Shaffer D, Fisher P, Dulcan M, et al: The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence and performance in the MECA study. Journal of the American Academy of Child and Adolescent Psychiatry 35:865-877, 1996Crossref, Medline, Google Scholar
31. Schwab-Stone ME, Shaffer D, Dulcan MK, et al: Criterion validity of the NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3). Journal of the American Academy of Child and Adolescent Psychiatry 35:878-888, 1996Crossref, Medline, Google Scholar
32. Goodman SH, Hoven CW, Narrow WE, et al: Measurement of risk for mental disorders and competence in a psychiatric epidemiologic community survey: the NIMH Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) study. Social Psychiatry and Psychiatric Epidemiology 33:162-173, 1998Crossref, Medline, Google Scholar
33. McCullagh P, Nelder JA: General Linear Models. New York, Chapman and Hall, 1989Google Scholar
34. SAS/STAT User's Guide, ver 8. Cary, NC, SAS Institute Inc, 1999Google Scholar
35. Sussman LK, Robins LN, Earls F: Treatment-seeking for depression by black and white Americans. Social Science and Medicine 24:187-196, 1987Crossref, Medline, Google Scholar
36. Zito JM, Safer DJ, DosReis S, et al: Racial disparity in psychotropic medications prescribed for youths with Medicaid insurance in Maryland. Journal of the American Academy of Child and Adolescent Psychiatry 37:179-184, 1998Crossref, Medline, Google Scholar
37. McMiller WP, Weisz JR: Help-seeking preceding mental health clinic intake among African-American, Latino, and Caucasian youths. Journal of the American Academy of Child and Adolescent Psychiatry 35:1086-1094, 1996Crossref, Medline, Google Scholar
38. Shapiro S, Skinner EA, Kessler LG, et al: Utilization of health and mental health services. Archives of General Psychiatry 41:971-978, 1984Crossref, Medline, Google Scholar
39. Wells KB, Manning WG, Duan N, et al: Sociodemographic factors and the use of outpatient mental health services. Medical Care 24:75-85, 1986Crossref, Medline, Google Scholar
40. Burns BJ, Costello EJ, Erkanli A, et al: Insurance coverage and mental health service use by adolescents with serious emotional disturbance. Journal of Child and Family Studies 6:89-111, 1997Crossref, Google Scholar
41. Glied S, Hoven CW, Moore R, et al: Children's access to mental health care: does insurance matter?. Health Affairs 16:167-174, 1997Crossref, Medline, Google Scholar
42. Birmaher B, Ryan ND, Williamson BA, et al: Child and adolescent depression: a review of the past 10 years. Part II. Journal of the American Academy of Child and Adolescent Psychiatry 35:1575-1582, 1996Crossref, Medline, Google Scholar
43. Clarke GN, Rohde P, Lewinsohn PM, et al: Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child and Adolescent Psychiatry 38:272-279, 1999Crossref, Medline, Google Scholar
44. Emslie GJ, Walkup JT, Pliszka SR, et al: Nontricyclic antidepressants: current trends in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 38:517-528, 1999Crossref, Medline, Google Scholar
45. Geller B, Reising D, Leonard HL, et al: Critical review of tricyclic antidepressant use in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 38:513-516, 1999Crossref, Medline, Google Scholar



