Tenure in Supportive Housing for Homeless Persons With Severe Mental Illness
Abstract
OBJECTIVE: The study examined the long-term effectiveness of approaches to housing homeless persons with serious mental illness. METHODS: A total of 2,937 persons placed in high-, moderate, -and low-intensity housing were followed for up to five years. Intensity reflected on the amount of structure and degree of clients' independence. The outcome variable was tenure in housing. Cox stepwise regression was used to calculate risk ratios of becoming discontinuously housed. RESULTS: Thirty percent of the sample were initially placed in high-intensity settings, 18 percent in moderate-intensity settings, and 52 percent in low-intensity settings. Those in high-intensity settings tended to be younger, to be referred from hospitals, and to have a history or diagnosis of substance abuse. Individuals in moderate-intensity settings were more likely to be female and were least likely to have substance abuse problems. Individuals in low-intensity settings were more likely to be referred by municipal shelters and to have lived in municipal shelters for four or more months. After one, two, and five years, 75 percent, 64 percent, and 50 percent, respectively, of the sample were continuously housed. Older age was associated with longer tenure, and having a history of substance abuse was associated with shorter tenure. Individuals referred from a state psychiatric center had a greater risk of shorter tenure than other types of referrals. CONCLUSIONS: Results show that homeless persons with serious mental illness can remain in stable housing for periods of up to five years, supporting the premise that long-term residential stability can be enhanced by providing access to safe and affordable supportive housing.
Although homelessness among persons with serious mental illness remains a major social problem in America, mounting evidence suggests that it is far from intractable. A range of housing alternatives developed in combination with specialized service programs, generally referred to as supportive housing, has proven effective in providing stable housing for homeless persons with serious mental illness (1,2).
In recent years interest has grown in developing supportive housing that combines principles of community mainstreaming, tenant empowerment, and flexibility in the programming of mental health services (3). Several studies have contrasted the effectiveness of different types of supportive housing and have examined factors affecting housing stability. More knowledge about the long-term effectiveness of the various approaches is required to guide future planning and development efforts.
One of the first housing studies compared two groups of homeless persons with serious mental illness (4). One group had been admitted to an acute inpatient psychiatric service and was discharged to supportive single-room-occupancy residences, and the other received routine discharge planning. After one year, those in supportive housing had spent significantly more nights in stable housing and fewer nights in hospitals or undomiciled.
The second series of McKinney research demonstration programs for homeless persons with serious mental illness sponsored by the National Institute of Mental Health supported five experimental studies in four cities (1). The demonstrations did not compare housing models but did examine housing outcomes for individuals who received different types of case management services linked to housing resources. Results pooled from the five sites indicated that access to a variety of housing options, in conjunction with case management, treatment, and rehabilitation, was effective in engaging and housing homeless persons with serious mental illness and that individuals reported some improvement in quality of life (1). But in none of the five sites was a significant change in functioning over time demonstrated (5). The presence of a concomitant substance use disorder was shown to strongly affect housing outcomes at the San Diego site (6).
One notable debate in the literature on housing for persons with serious mental illness focuses on the supported housing model as contrasted with other housing in the residential continuum of care. In this paper, the term "supportive housing" describes all housing approaches linked to some form of support services regardless of configuration. The term "supported housing" —a form of supportive housing—is reserved for housing that is permanent independent housing with flexible individualized services and supports that are integrated into the community and chosen by the consumer. Housing needs are viewed as being paramount and as separate from treatment needs. Treatment-oriented supportive housing options constitute the remainder of the residential continuum (3,7,8). They include group homes, supportive apartments, community residences, and halfway houses where housing and services are generally integrally related. The Center for Mental Health Services of the Substance Abuse and Mental Health Services Administration, which uses the terms supportive and supported housing in a similar manner, has recently funded a multisite evaluation to compare outcomes for tenants in supported housing and those in other housing types on the residential continuum.
Evidence suggests that consumers are more likely to have good outcomes if they feel satisfied with their housing and perceive their living environment to be a good match for their needs (9). Consumer preference studies indicate that individuals consistently prefer to live in housing that is their own, affordable, permanent, and integrated into the community and that offers flexible supports as needed (10). Consumer choice, autonomy, and control are important themes in studies that have explored housing preferences (11,12). Bebout and Harris (8) described environmental factors that affect housing tenure, including types and level of structure, level of interpersonal intensity, expectations for self-sufficiency, anticipated lengths of stay, and orientation toward growth or maintenance.
In three studies in which housing environments were characterized by their levels of structure and expectation, environments that provided supportive social relationships with moderate levels of structure and expectation were associated with better outcomes, whereas those with higher levels of structure and demand were associated with poorer outcomes (13). The extent to which a housing type will result in good housing for a given tenant requires further exploration.
In response to a scarcity of housing for homeless persons with serious mental illness in New York City, the New York-New York Agreement was signed in August 1990 by the mayor of New York City and the governor (14). The agreement was to place 5,225 homeless persons with serious mental illness into housing and to develop 3,314 units of supportive housing. New York City pledged to develop 1,426 new single-room-occupancy residence units, and the state pledged to develop 1,888 units. By the end of December 31, 1997, a total of 3,048 new housing units had been opened, and 8,594 homeless persons with serious mental illness who were eligible under the agreement had obtained housing. A total of 5,660 individuals moved into existing and newly developed supportive housing units.
Housing models developed under this agreement cover a variety of models along the residential continuum. Information on the target population and the characteristics of the housing allowed us to conduct a naturalistic study of tenure in housing and the factors affecting residential stability. This paper reports the results of the longest follow-up study conducted to date, which tracked individuals for up to five years.
Methods
Population and data
The sample was composed of 2,937 homeless persons with serious mental illness who became residents of 67 supportive housing settings through the New York-New York Agreement from May 1, 1990, through August 31, 1995. Individuals were tracked from the time they moved into one of the housing settings to September 30, 1995, or until the time they were no longer considered to be residing in stable housing. Differential follow-up times are accounted for in the statistical methods described below.
Eligibility of consumers for housing is determined through a central application process operated by New York City's Human Resources Administration. More than 200 referral agencies submit housing applications annually, requesting a determination of eligibility for individual clients. After access to housing is approved, the referring agencies submit approved applications to housing and service providers requesting interviews for clients at specific housing sites. Acceptance criteria vary depending on the type of housing and the individual provider.
Administrative databases on consumers and housing types were available to the researchers. The Human Resources Administration's office of health and mental health services, as part of its responsibilities under the agreement, maintains data on client characteristics collected at the time of referral and the residential outcomes of individuals who move into the housing. The latter information is collected from monthly reports submitted by housing providers. Tenant data include information about demographic characteristics, financial support, referral source, and history of homelessness. Clinical information includes reported DSM diagnoses, history of substance abuse, psychopharmacological treatments, present and past symptoms, and level of functioning.
Data on housing characteristics of supportive housing settings throughout New York City came from the residential placement management system of the Center for Urban Community Services maintained as part of its contractual responsibilities with the state and the city. Approximately 25 variables are used to describe housing characteristics, including size, physical configuration, tenant mix, tenancy rights, licensure, geographic location, house rules, and types of on-site services. If the individual units in the setting differed on a characteristic, the most predominant characteristic was used to describe the setting.
Groupings
Housing setting categories.
For this study, the housing settings were categorized into high, moderate, or low intensity based on the amount of structure imposed and the degree of independence offered to tenants. Structure refers to the level of daily scheduled routines and activities, house rules, security features, and requirements for program participation. Independence refers to the tenant's level of autonomy, including control over decisions about his or her living environment, activities, personal income, management of medications, and degree of privacy. A multisite national study of housing approaches for persons with serious mental illness uses similar variables as measured by the unpublished Center for Mental Health Services Housing Initiative Fidelity Instrument (Substance Abuse and Mental Health Services Administration, 1998).
The two authors most familiar with the housing (FRL and AH) categorized the different settings based on the predominant characteristics of a site. Housing consultants who had expert knowledge of the housing developed through the New York-New York Agreement, working with data from the residential placement management system, reviewed the groupings and concurred with the researchers' categorizations.
Nineteen sites were classified as high intensity. These sites had a total of 512 beds and ranged in size from 12 to 60 beds, with a mean of 28.1 beds per site. High-intensity settings are exclusively dedicated to persons with serious mental illness and are licensed by the state. Forty-two percent of these settings, or eight sites, exclusively serve individuals who are dually diagnosed. The vast majority of the high-intensity settings (17 sites, or 90 percent) are regarded as transitional, with a projected length of stay of 18 to 24 months, although individuals can and frequently do stay longer. Residents do not have leases or rental agreements. Rent payment is set at the level II Supplemental Security Income (SSI) rate of $823, and consumers receive a monthly personal-needs allowance of approximately $110.
More than half of the 19 high-intensity settings (11 sites, or 58 percent) provided congregate living arrangements, and meals were often supplied. High staffing levels at such sites are typical, and on-site policies are restrictive. Most of the high-intensity settings in the study had a curfew (15 sites, or 78 percent) and did not permit overnight guests (16 sites, or 84 percent). Money management was mandatory at 16 sites (84 percent), and the remaining three sites (16 percent) provided the service as needed. At 17 sites (90 percent) medications were dispensed, and at the remaining two sites (10 percent) medications were monitored. Attendance at a structured day activity for 20 to 30 hours per week was required at 13 sites (68 percent).
Ten settings, with a total of 499 units, were classified as moderate intensity. The number of units within a site ranged from 24 to 78, with a mean of 50 units per site. All moderate-intensity settings provide housing exclusively to persons with serious mental illness. They are operated by not-for-profit agencies and licensed by the state. Residents in moderate-intensity settings have their own rooms or studio apartments, and cooking facilities are shared. The housing, which is generally considered permanent, has common space for group activities. Tenants receive occupancy agreements that delineate the mutual responsibilities of the housing provider and the resident. Seventy-nine of the tenants in moderate-intensity settings had leases. Rent payment is set at level II of the SSI rate, and residents receive a personal needs allowance of $400.
House rules governing curfews and visitors at moderate-intensity sites do exist but are flexible. At six of the study sites (60 percent) overnight guests were not allowed, and two sites (20 percent) imposed a curfew. Moderate-intensity settings provide on-site 24-hour staff coverage. Services offered on site are fairly intensive but are usually not mandatory. At nine study sites (90 percent) money management was provided as needed, and it was mandatory at one site (10 percent). Seven study sites (70 percent) provided a high level of medication management, and three sites (30 percent) provided a lower level. Program participation was required at only one site.
Thirty-eight sites in the study were classified as low intensity, with a total of 1,524 units. The sites ranged from six to 650 units, with a mean of 87 units per site. At one end of the spectrum were single apartments in a mixed-tenancy building, and at the other end were units in a large hotel-type facility. Low-intensity settings provide permanent housing, are unlicensed, and in most cases are owned or managed by not-for-profit agencies. Twenty-eight study sites (73 percent) had mixed tenancies of disabled and nondisabled populations. Tenants at low-intensity sites hold legally binding leases for individual furnished private rooms or small studio-type apartments, with access to either shared or private bathrooms and cooking facilities. Twenty-six of the study sites (68 percent) offered shared cooking arrangements. Rent is no more than 30 percent of a tenant's income.
Many of the low-intensity sites in the study had lounges and recreational and social service space. Overnight guests were permitted at 32 sites (84 percent), and only seven sites (19 percent) imposed a curfew. Services are provided to tenants on or off site through multidisciplinary teams. Only five sites (14 percent) required program participation. Money and medication management services were offered at 30 sites (80 percent), but these services were not mandatory.
Outcome categories
The outcome variable used in the study was tenure in housing. Individuals who became homeless, moved into unstable and marginal housing situations, or were imprisoned were considered to no longer be residing in stable housing and were classified as discontinuous placements. Those who remained in their initial housing or moved to settings regarded as stable housing were classified as being continuously housed. Individuals who were admitted to hospitals for physical conditions for extended times, who died, or who moved to appropriate housing but who could not be followed up by the Human Resources Administration were considered to be "censored" at the time of the move and hence were not categorized as a discontinuous placement or as continuously housed.
Hypotheses and statistical methods
Using the policy analysis framework of intent to treat, in the statistical analyses tenants were associated with their initial housing placement even though they could have moved. We hypothesized that consumers in initial placements of different intensities would differ in their demographic characteristics and previous use of mental health service modalities as well as homeless services. To test for significant differences, we used the t statistic in a test of equality of means and the chi square statistic in a test of equality of binomial proportions.
We hypothesized that the time an individual spent continuously housed would differ according to the initial housing type, that both client characteristics and housing characteristics of the initial placement would affect tenure in continuous housing, and that the characteristics affecting tenure would be different based on the level of intensity of the initial housing site. To examine the set of hypotheses concerning tenure in housing, we used survival models that take into account that members of the study cohort have different follow-up times. The survival variable in all analyses was time continuously housed. A "failure" occurred at the time that a person was determined to have a discontinuous placement. The tenure data of a tenant who was followed for less than five years and who was continuously housed at the last observation point was treated as a censored observation.
Tenure for the full sample was examined across all initial placements and by initial type of housing placement using a Kaplan-Meier estimate of the distribution function of survival time. The hazard rate, the probability of leaving housing at any given point in time (given being continuously housed up to time t) was estimated using the life table method with an interval of seven days.
The effects of client and housing characteristics on tenure were examined separately for each initial placement category. For each housing type, a forward stepwise Cox regression survival model was used in which the hazard rate and the effect of covariates on the rate are simultaneously modeled. For each housing type, the variables with risk ratios significantly different from 1 (p<.05), the level of significance, and the order of entry of the variable into the model are reported.
The risk ratio for continuous variables is the increased risk of one unit of change in the variable on the likelihood of becoming discontinuously housed when all other variables are held constant. For categorical variables, for each category of a variable (except for one binary indicator), variables were introduced that contrast the category with the excluded category. In this case, the risk ratio is the increase in risk of being in that category of the variable versus being in any other of its categories on the likelihood of becoming discontinuously housed when all other variables are held constant. Risk ratios greater than 1 indicate an increased risk, and those less than 1 indicate a decreased risk.
Results
Sample description
Table 1 shows demographic and clinical characteristics of the 2,937 consumers in the sample by their type of placement, as well as their previous use of homeless services and referral sources. Thirty percent were initially placed in high-intensity settings, 18 percent in moderate-intensity settings, and 52 percent in low-intensity settings. Sixty-seven percent of the sample were male, and the mean age of the sample was 40 years. Fifty-eight percent were African American, 16 percent were Hispanic, and 20 percent were Caucasian.
Fifty percent were diagnosed as having schizophrenia, 37 percent had bipolar disorder or some other form of mood disorder, 7 percent had a delusional disorder or other psychotic disorder, and the remainder had other axis I diagnoses. Fifty-six percent of the sample had a diagnosis of substance abuse, and 69 percent had a history of substance abuse.
As Table 1 indicates, 31 percent were long-term users of municipal shelters, having lived in shelters for four or more consecutive months; 21 percent used municipal shelters for shorter periods or on an episodic basis; and 18 percent used drop-in centers or voluntary shelters. Twenty-one percent were living on the streets or in other public spaces.
Individuals were referred from a variety of agencies, with the largest number (23 percent) referred by community hospitals, including municipal and not-for-profit hospitals and veterans' facilities. Fourteen percent were referred by state psychiatric centers, 13 percent by municipal shelters, 7 percent by shelter-based mental health programs, 18 percent by shelter-based transitional housing programs for persons with serious mental illness, and 14 percent by programs that work with individuals who live on the streets.
Group comparisons
On all the variables listed in Table 1, tenant profiles differed significantly (p<.001). Compared with consumers initially placed in moderate- or low-intensity settings, those placed in high-intensity settings tended to be younger, more likely to be referred from either state or community hospitals (53 percent), and more likely to have a history of substance abuse (84 percent) or a diagnosis of substance abuse (60 percent). Individuals in moderate-intensity settings were more likely to be female (46 percent) than those in the other housing categories, and they were least likely to have a substance abuse history (52 percent) or diagnosis (26 percent).
Individuals in low-intensity housing settings were more likely to be referred by municipal shelters (22 percent) and to have lived in municipal shelters for four or more months (36 percent). Compared with consumers in the high-intensity and moderate-intensity housing, this group was in the middle in terms of having a substance abuse history (65 percent) or diagnosis (41 percent). Both moderate- and high-intensity settings were more likely to house persons with schizophrenia (64 percent) than were low-intensity settings (36 percent), where the predominant diagnosis was bipolar disorder or another mood disorder (47 percent).
Tenure in housing
For the sample as a whole, 75 percent, 64 percent, and 50 percent of consumers were continuously housed after one, two, and five years, respectively. The likelihood of becoming discontinuously housed was greatest—approximately 15 persons per 1,000—in the first four months of being housed, and it was lower and fairly stable—approximately five persons per 1,000—over all subsequent time points in the follow-up period.
Individuals placed in high-intensity settings accounted for most of the increased hazard of becoming discontinuously housed during the first 120 days after placement. Among those placed in low-intensity settings, 54 percent were still continuously housed after five years. This figure was 56 percent for moderate-intensity settings and 37 percent for high-intensity settings.
In Table 2 it can be seen that in all housing types, older age was associated with longer tenure, and having a history of substance abuse was associated with shorter tenure. Other personal characteristics differentially entered each of the models for the different intensities of housing. In high-intensity housing, those who had no income source had a decreased risk of shorter tenure. In moderate-intensity housing, African Americans had a decreased risk of shorter tenure. In low-intensity housing the risk was decreased by having a diagnosis of bipolar disorder or another mood disorder. In addition, in moderate-intensity housing, those who had fewer difficulties performing activities of daily living had a greater likelihood of a better outcome.
Individuals referred from a state psychiatric center had a greater risk of shorter housing tenure than individuals referred from any other source. Other person-system variables differentially entered the models for different intensity housing. In high-intensity housing, being a short-term shelter user (less than four months) was associated with shorter tenure, as was having a referral from a community-based mental health agency in moderate-intensity housing and having a referral from a community hospital in low-intensity housing.
Housing characteristics that played a role in tenure varied by housing type. In high-intensity housing, consumers who lived in noncongregate living arrangements and medium-size units (28 to 99 beds) had longer housing tenures. Those who lived in high-intensity settings that provided minimal medication management services had shorter tenures. Consumers initially placed in moderate-intensity housing had shorter tenures if their housing units granted occupancy agreements and allowed overnight guests. Forty percent of the moderate-intensity units allowed overnight guests.
For those initially placed in low-intensity housing, tenure was longer in settings in which studio floor plans predominated and shorter in settings in which all units had their own bathrooms. Most persons living in units with individual bathrooms were in buildings in which studio floor plans predominated; the correlation coefficient of these two housing conditions was .84. Thus the shorter tenure was accounted for by the 3 percent of persons in low-intensity housing who lived in units in buildings in which studio floor plans did not predominate and in which all units had an individual bathroom.
Discussion and conclusions
A small but growing number of longitudinal studies consistently demonstrate that homeless persons with serious mental illness can achieve residential stability for 12 to 24 months in various types of supportive housing (1,2,4,6). The findings of this study demonstrate that homeless persons with serious mental illness can remain in stable housing for significantly longer periods of up to five years, supporting the premise that long-term residential stability can be enhanced by providing this population with access to safe and affordable supportive housing. Improved long-term residential stability should have significant cost implications and should also have an impact on service utilization.
The tenure analysis in this study showed that homeless persons with serious mental illness had a heightened vulnerability to move into unstable living arrangements in the first four months after placement, especially those placed in high-intensity settings. Moving into a new residence is a stressful life event for anybody, necessitating a series of adaptations to a variety of changes. For individuals with a significant level of functional impairment, the need to simultaneously adjust to a new community with new neighbors, different resources, different demands, and uncertain expectations may strain their already tenuous survival skills.
The stress of moving may be further compounded by a heightened level of scrutiny that a new resident experiences when interacting with a landlord who is interested in determining whether the client will be a "good" tenant who abides by the house rules, gets along with neighbors, and fits in with the community. Strategies to enhance engagement, minimize stress, and facilitate adaptation during this critical period are needed in some supportive housing programs, as well as in programs that help individuals gain access to housing (15).
The results resoundingly indicate the negative effect that substance abuse can have on the residential stability of homeless persons with serious mental illness in all housing types. This finding is consistent with those of the McKinney demonstration project in San Diego, which found that housing stability was strongly affected when subjects were involved with drugs or alcohol (6,16). The study reported here also examined housing tenure among dually diagnosed consumers, although those results are not presented in this paper. It was found that persons who initially moved into highly structured settings dedicated exclusively to mentally ill consumers with chemical dependency problems were less likely to achieve residential stability than their counterparts in housing that did not focus on chemical dependency.
In light of the prevalence of substance abuse in this population, a critical need exists to develop new strategies to enhance residential stability. Greater flexibility and tolerance about the management of relapse, including the use of harm reduction strategies, may be necessary. High levels of structure and supervision may not be well tolerated by consumers during the engagement phase of treatment for substance abuse (17). Research to elucidate effective strategies is essential.
Homeless individuals referred from community and state psychiatric hospitals were more likely to have poor housing outcomes regardless of the type of housing. Multiple interrelated factors may provide an explanation for this finding. Those referred from hospitals may have higher levels of functional impairment and higher rates of substance abuse, which could adversely affect tenure outcomes. In addition, individuals discharged from hospitals may need enhanced access to rehabilitation programs that specifically focus on the development of housing readiness skills. Greater consumer input into the process of housing selection may also be vital to improving outcomes for those discharged from hospitals (18).
Specific characteristics of the initial housing type can strongly influence tenure. In high-intensity settings, a low level of medication management predicted poorer outcomes, suggesting that treatment compliance is a major issue in a population in which more than half have been referred to housing directly from psychiatric hospitals. However, in high-intensity settings, more normalized living conditions appear to lead to more favorable outcomes. Persons who entered high-intensity housing that was of medium size and offered noncongregate living arrangements had better housing outcomes.
Normalization had a converse effect for initial placements in moderate-intensity housing. In these settings, having an occupancy agreement and being able to have overnight guests increased the risk of poor outcomes, suggesting that for this type of housing, normalized conditions may need to be more slowly introduced. In low-intensity housing, persons in units with studio floor plans fared better than those in the less normalized housing units composed of single rooms, suites, or shared apartments.
Overall, our study demonstrates that homeless persons with serious mental illness can have positive residential outcomes in housing that has many of the characteristics described by supported housing advocates, as well as in housing that is more treatment oriented. Discussions about housing for this population have at times unnecessarily pitted the residential continuum model against the supported housing model. Normalized housing seems an unassailable goal for some individuals, but clinical realities can prevent its attainment. Although some individuals will initially benefit from normalized housing, others may require various degrees of structure, interpersonal intensity, and support. Varied types of housing are needed to meet the heterogeneous needs of a diverse consumer group.
The study has several limitations. The only outcome data available pertained to an individual's tenure in housing, and the relationship of these outcomes to consumer satisfaction, quality of life, symptoms, and levels of functioning is not known. Neither did we have data on some variables that others have reported may influence outcome, such as duration of homelessness, symptoms, or consumer preferences. Finally, the naturalistic design allowed us to examine outcomes within a housing type but did not allow us to compare outcomes among housing types. Randomized studies or those aimed at controlling client characteristics across housing categories would be required to compare outcomes among housing types.
Solving the problem of homelessness among the mentally ill population is contingent on the development of an adequate range of housing options linked to a comprehensive and integrated array of services (19,20). Although housing in and of itself will not solve the problem or meet the multifaceted needs of homeless mentally ill individuals, it is one of the crucial missing links (21). We join other researchers in the field who have cautioned that placement into housing should not be accompanied by expectations of permanence but should be viewed as part of an ongoing process of community integration (22). Nonetheless, this study emphasizes the fact that supportive housing is a powerful vehicle through which homeless mentally ill individuals can be reintegrated into the community and linked to community-based services.
Acknowledgment
Partial support for this study was received from center grant P50-51359 from the National Institute of Mental Health.
Dr. Lipton is deputy commissioner and medical director of the office of health and mental health services of the New York City Human Resources Administration, 136 Church Street, New York, New York 10007. He is also clinical associate professor of psychiatry at New York University School of Medicine. Dr. Siegel is research professor in the department of psychiatry of New York University School of Medicine. She is also head of the epidemiology and health services research laboratory at the Nathan Kline Institute for Psychiatric Research in Orangeburg, New York, where Dr. Samuels and Dr. Baker are research scientists. Mr. Hannigan is executive director of the Center for Urban Community Services in New York City.
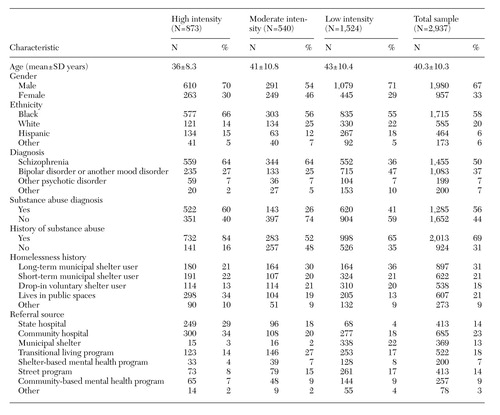 |
Table 1. Demographic and clinical characteristics that significantly differentiated (p<001) among 2,937 homeless persons with serious mental illness placed in high-, moderate-, or low-intensity housing
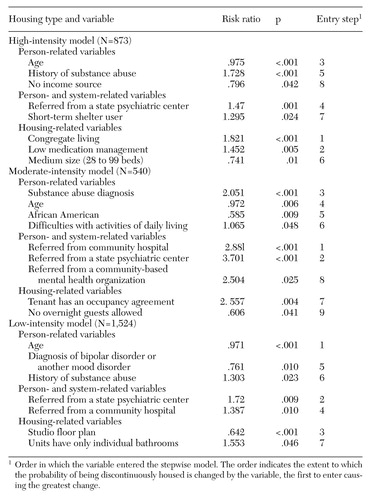 |
Table 2. Results of three separate Cox stepwise regression survival models for each housing intensity type
1. Shern DL, Felton CJ, Hough RL, et al: Housing outcomes of homeless adults with mental illness: results for the second-round McKinney program. Psychiatric Services 48:239-241, 1997Link, Google Scholar
2. Newman SJ, Reschovsky JD, Kaneda K, et al: The effects of independent living on persons with chronic mental illness: an assessment of the Section 8 certificate program. Milbank Quarterly 72:171-198, 1994Crossref, Medline, Google Scholar
3. Carling PJ: Housing and supports for persons with mental illness: emerging approaches to research and practice. Hospital and Community Psychiatry 44:439-449, 1993Abstract, Google Scholar
4. Lipton F, Nutt S, Sabitini A: Housing the homeless mentally ill: a longitudinal study of a treatment approach. Hospital and Community Psychiatry 39:40-45, 1988Abstract, Google Scholar
5. Rog DJ, Holupka CS, Brito MC: The impact of housing on health: examining supportive housing for individuals with mental illness. Current Issues in Public Health 2:153-160, 1996Google Scholar
6. Hurlburt MS, Hough R, Wood PA: Effects of substance abuse and housing stability of homeless mentally ill persons in supported housing. Psychiatric Services 47:731-736, 1996Link, Google Scholar
7. Ridgeway PA, Zipple A: The paradigm shift in residential services: from linear continuum to supported housing approaches. Psychosocial Rehabilitation Journal 12(4):11-31, 1990Google Scholar
8. Bebout RR, Harris M: In search of pumpkin shells: residential programming for the homeless mentally ill, in Treating the Homeless Mentally Ill: A Task Force Report of the American Psychiatric Association. Edited by Lamb HR, Bachrach LL, Kass FL. Washington, DC, American Psychiatric Association, 1992Google Scholar
9. Coulton CJ, Holland TP, Fitch VF: Person-environment congruence and psychiatric patient outcome in community care homes. Administration in Mental Health 12:71-88 1984Crossref, Google Scholar
10. Tanzman B: An overview of surveys of mental health consumers' preferences of housing and support services. Hospital and Community Psychiatry 44:450-455, 1993Abstract, Google Scholar
11. Srebnik D, Livingston J, Gordon L, et al: Housing choice and community success for individuals with serious and persistent mental illness. Community Mental Health Journal 31:139-152, 1995Crossref, Medline, Google Scholar
12. Schutt RK, Goldfinger SM: Housing preferences and perceptions of health and functioning among homeless mentally ill persons. Psychiatric Services 47:381-386, 1996Link, Google Scholar
13. Cournos F: The impact of environmental factors on outcome in residential programs. Hospital and Community Psychiatry 38:848-852, 1987Abstract, Google Scholar
14. Lipton FR: The New York-New York Agreement to House Homeless Mentally Ill Individuals: Summary Placement Report. New York City, Human Resources Administration, Office of Health and Mental Health Services, Mar 1998Google Scholar
15. Susser E, Valencia E, Conover S, et al: Preventing recurrent homelessness among mentally ill men: a "critical time" intervention after discharge from a shelter. American Journal of Public Health 87:256-262, 1997Crossref, Medline, Google Scholar
16. Dickey B, Gonzalez O, Latimer E, et al: Use of mental health services by formerly homeless adults residing in group and independent housing. Psychiatric Services 47:152-158, 1996Link, Google Scholar
17. Drake RE, Osher FC, Wallach MA: Homelessness and dual diagnosis. American Psychologist 46:1149-1158, 1991Crossref, Medline, Google Scholar
18. Minsky S, Riesser G, Duffy M: The eye of the beholder: housing preferences of inpatients and their treatment teams. Psychiatric Services 46:173-176, 1995Link, Google Scholar
19. Talbott JJ, Lamb HR: Summary and recommendations, in The Homeless Mentally Ill. Edited by Lamb HR. Washington, DC, American Psychiatric Association, 1984Google Scholar
20. Dennis DL, Buckner JC, Lipton FR, et al: A decade of research and services for homeless mentally ill persons: where do we stand? American Psychologist 46:1129-1138, 1991Google Scholar
21. Baxter E, Hopper K: Shelter and housing for the homeless mentally ill, in The Homeless Mentally Ill. Edited by Lamb HR. Washington, DC, American Psychiatric Association, 1984Google Scholar
22. Bachrach LL: What we know about homelessness among mentally ill persons: an analytical review and commentary. Hospital and Community Psychiatry 43:453-464, 1992Abstract, Google Scholar



