Datapoints: Mental Health Parity and Employer-Sponsored Health Insurance in 1999-2000: II. Copayments and Coinsurance
Health plans that limit coverage partly insure individuals against smaller expenses for mental health care but leave them at full risk for large expenses that exceed the limit. In 1999-2000, four of every five persons with employer-sponsored insurance were subject to limits on the number of inpatient days and outpatient visits for mental health care (1).
We examined changes in copayments and coinsurance for covered benefits. Data on plan benefits were obtained from the employer survey in the Health Care for Communities Study, conducted between July 1999 and July 2000 (2). Data for earlier years were obtained from the Bureau of Labor Statistics (3). Copayments are a fixed dollar amount that the patient pays for each service, regardless of the service's cost. Coinsurance, on the other hand, requires the patient to pay a fixed proportion of the total cost of the visit.
Figure 1 contrasts outpatient copayments for mental health and medical care in 1999-2000. Four of five employees have medical copayments of less than $20 per visit, whereas only two of five have mental health copayments of less than $20. No employee reports coinsurance rates greater than 20 percent for medical care. However, two of five employees report coinsurance rates for mental health care of 50 percent.
Figure 2 shows the percentage of employees who are subject to different copayments or coinsurance rates for outpatient mental health care compared with primary care or specialty medical care. The proportion of persons with different copayments or coinsurance rates for mental health care appears to have changed little over time.
Acknowledgment
The Health Care for Communities Study was funded by the Robert Wood Johnson Foundation.
The authors are affiliated with Rand, 1700 Main Street Santa Monica, California 90401 (e-mail, [email protected]). Harold Alan Pincus, M.D., and Terri L. Tanielan, M.A., are editors of this column.
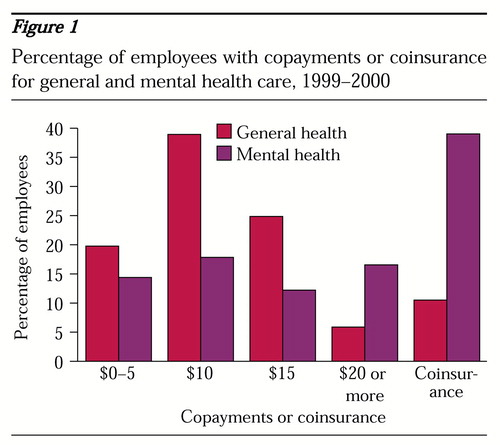
Figure 1. Percentage of employees with copayments or coinsurance for general and mental health care, 1999-2000
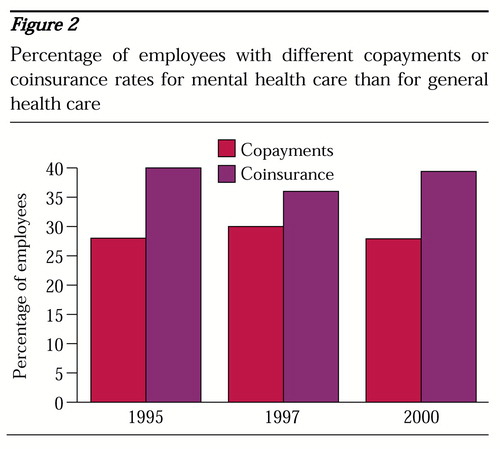
Figure 2. Percentage of employees with different copayments or coinsurance rates for mental health care than for general health care
1. Sturm R, Pacula RL: Mental health parity and employer-sponsored health insurance in 1999-2000: I. limits. Psychiatric Services 51:1361, 2000Link, Google Scholar
2. Sturm R, Gresenz CR, Sherbourne CD, et al: The design of Health Care for Communities: a study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry 36:221-233, 1999Medline, Google Scholar
3. Employee Benefits in Medium and Large Private Establishments. Washington, DC, Bureau of Labor Statistics, various yearsGoogle Scholar



