Patient Flow and Reutilization of Crisis Services Within 30 Days in a Comprehensive Crisis System
Abstract
Objective:
Crisis services are undergoing an unprecedented expansion in the United States, but research is lacking on crisis system design. This study describes how individuals flow through a well-established crisis system and examines factors associated with reutilization of such services.
Methods:
This cross-sectional study used Medicaid claims to construct episodes describing the flow of individuals through mobile crisis, specialized crisis facility, emergency department, and inpatient services. Claims data were merged with electronic health record (EHR) data for the subset of individuals receiving care at a crisis response center. A generalized estimating equation was used to calculate adjusted odds ratios for demographic, clinical, and operational factors associated with reutilization of services within 30 days of an episode’s end point.
Results:
Of 41,026 episodes, most (57.4%) began with mobile crisis services or a specialized crisis facility rather than the emergency department. Of the subset (N=9,202 episodes) with merged EHR data, most episodes (63.3%) were not followed by reutilization. Factors associated with increased odds of 30-day reutilization included Black race, homelessness, stimulant use, psychosis, and episodes beginning with mobile crisis services or ending with inpatient care. Decreased odds were associated with depression, trauma, and involuntary legal status. Most (59.3%) episodes beginning with an involuntary legal status ended with a voluntary status.
Conclusions:
Crisis systems can serve a large proportion of individuals experiencing psychiatric emergencies and divert them from more restrictive and costly levels of care. Understanding demographic, clinical, and operational factors associated with 30-day reutilization may aid in the design and implementation of crisis systems.
HIGHLIGHTS
Most episodes (57.4%) began with mobile crisis services or specialized crisis facilities rather than the emergency department.
Most episodes (63.3%) were not followed by service reutilization; of those that were, 73.0% occurred in crisis settings (mobile or specialized facility) rather than in the emergency department.
Factors associated with higher odds of service reutilization were male sex, age range of 35–44 years, Black race, homelessness, stimulant use, psychosis, index episode beginning with mobile crisis care, and index episode ending in inpatient care.
Factors associated with lower odds of service reutilization were depression, trauma, and involuntary legal status.
In most communities, the typical response to a psychiatric crisis is to call 911, go to the emergency department (ED), or both. Unlike general medical emergencies, a 911 call for a mental disorder or substance use disorder emergency often leads to a law enforcement response, putting persons in crisis at risk for incarceration or death and potentially preventing them from receiving the treatment they need. ED visits for psychiatric emergencies have steadily grown in recent years and now account for one in eight ED visits annually (1). Despite this increase in volume, most EDs are poorly equipped to address emergencies related to mental disorders or substance use disorders, and individuals can be held in the ED for hours or days without treatment while awaiting transfer to inpatient psychiatric units (2). This practice results in a poor experience for the person in crisis and a poor use of resources. These disparities in psychiatric versus general medical emergency care are magnified for people of color, and Black Americans experiencing psychiatric emergencies are at the highest risk for dying in police encounters and being physically restrained in the ED (3, 4).
There is increasing interest in creating community-based crisis systems that provide treatment in less restrictive and less costly settings. In 2021, the Substance Abuse and Mental Health Services Administration (SAMHSA) outlined a vision in which everyone has access to three pillars of crisis care: someone to call (crisis lines), someone to respond (mobile crisis teams), and a safe place to go (specialized crisis facilities) (5). Subsequently, a National Council for Mental Wellbeing report emphasized the importance of an “accountable entity” to ensure that these individual components are integrated as a coordinated system of care (6). The recent implementation of the 988 Suicide and Crisis Lifeline was an important first step toward creating a better system of care for people in crisis, and communities across the nation are in various stages of developing the rest of the crisis continuum. Preliminary single-site studies have shown that crisis services can improve outcomes and reduce costs (7–9). However, best practices are still emerging, and more research is needed to understand how individuals interact with the different components of the crisis continuum and which services benefit which populations (10).
To address these questions, we analyzed crisis service utilization in Arizona, which, over the past several decades, has developed a comprehensive, coordinated, and financially sustainable crisis system that heavily influenced the SAMHSA guidelines (5). In the Arizona model, individuals can access crisis services through a 24/7 crisis line (now linked to the 988 Suicide and Crisis Lifeline) instead of calling 911. Most calls are resolved by telephone (11), but for those who need a higher level of intervention, mobile crisis teams and specialized crisis facilities provide alternatives to the ED and are able to stabilize most persons in crisis without the need for inpatient hospitalization. A regional behavioral health authority (RBHA) functions as the “accountable entity” and ensures that its contracted service providers work together to form a coordinated system. The RBHA receives financing through the Arizona Health Care Cost Containment System (AHCCCS), the state Medicaid agency, which braids multiple funding streams together to ensure that crisis services are provided to anyone in need, regardless of payer type.
In this study, we focused on mobile and facility-based services in Pima County, Arizona. First, we analyzed Medicaid claims to describe how individuals flow through the crisis and emergency care systems and how they may be diverted from the ED and inpatient utilization. Next, we merged claims with electronic health record (EHR) data from the Crisis Response Center (CRC) in Tucson, which provides 24/7 urgent care and 23-hour observation, as well as short-term inpatient care, to individuals who can access the facility via walk-in, transfer from an ED, or drop-off by mobile crisis teams or police. Finally, we examined demographic, clinical, and operational factors associated with reutilization of crisis services within 30 days after the end of an index episode (hereinafter termed 30-day reutilization).
Methods
Study Setting and Description of Crisis Services
Pima County is the second most populous county in Arizona, with a population of 1.06 million, 546,574 of whom reside in the city of Tucson. Pima County shares a border with Mexico, and over one-third (38.5%) of county residents identify as Hispanic or Latino. Racial demographic characteristics are as follows: 84.2% White, 50.1% non-Hispanic White, 4.5% Black or African American, 4.4% American Indian or Alaska Native, 3.4% Asian, and 3.3% two or more races (12). The crisis system in Pima County is overseen by the RBHA, which contracts with multiple provider organizations to deliver services (13). The mobile crisis service system comprises 12–16 two-person teams staffed by a combination of clinicians and peers who are dispatched by the crisis line, are required to respond within 60 minutes, and provide 24/7 coverage. The CRC, located in Tucson, provides 24/7 access to crisis services to anyone in need, including individuals experiencing acute distress who are actively suicidal, violent, intoxicated, or under an involuntary commitment. Individuals arrive as walk-ins, are referred from mobile crisis services, are transported by law enforcement, or are transferred from EDs. To incentivize law enforcement to use the crisis center instead of a jail or the ED, police officers are never turned away and can return to patrol duties within 10 minutes. “Medical clearance” at an ED is not required before arrival. Individuals with low levels of distress are seen in the clinic-like urgent care area and typically discharged within 2 hours. Individuals with more complex needs receive treatment in the secure 23-hour observation unit, which is staffed by an interdisciplinary team of 24/7 onsite medical providers (psychiatrists, nurse practitioners, or physician assistants), registered nurses, case managers, behavioral health technicians, and peers. Individuals who are in need of additional treatment after the 23-hour observation period are admitted to the short-term inpatient unit or transferred to one of several external inpatient psychiatric facilities. A second crisis stabilization facility in Tucson provides 23-hour observation and inpatient services only to individuals who arrive voluntarily and focuses on populations with substance use disorder needs.
Data Sources
In this cross-sectional study, we utilized data from two sources: AHCCCS Medicaid claims and EHR data from Connections Health Solutions, which operates the CRC. The AHCCCS claims and encounter data used in this study were provided by the Arizona State University Center for Health Information and Research. The initial analysis of AHCCCS data between January 10, 2018, and January 3, 2020, included all claims with billing codes for mobile crisis services (CPT code H2011), crisis facilities (CPT code S9484 or S9485), EDs (Universal Billing [UB] codes 0450–0459 or 0981 with a diagnosis of mental disorder or substance use disorder as defined by the Clinical Classifications Software Refined [CCSR] categories 650–670, with the exception of intellectual and developmental disability diagnoses [653, 654, and 655]), and inpatient facilities (UB codes with bill types 11x and 12x or revenue code 0114 with a diagnosis of mental disorder or substance use disorder). Records for people identified as dually eligible for Medicaid and Medicare were excluded. The claims data were then merged with all available CRC EHR data from the same time frame on the basis of AHCCCS IDs and crisis episode dates for all adults ages 18–64.
Crisis Episode Definition and Flow Analysis
AHCCCS claims were categorized as mobile crisis, crisis facility, ED, or inpatient on the basis of the related billing codes used for inclusion. AHCCCS covers mobile crisis and crisis facility services for anyone in need, regardless of Medicaid enrollment or eligibility (including people with private insurance that does not cover crisis services), for up to 72 hours (13), although approximately 80% of Arizonans seeking crisis services are Medicaid enrollees (14). If a claim for a higher level of care occurred within 72 hours of the initial claim, this subsequent claim was considered an escalation of care in the same crisis episode and was consolidated, with a defined starting point and end point (these data are available in the online supplement to this article). For example, an individual with a mobile crisis claim followed by a crisis facility claim within 72 hours would have “mobile crisis” as the starting point and “crisis facility” as the end point. A stand-alone crisis facility claim with no subsequent claims within 72 hours would have “crisis facility” as both the starting point and end point. These crisis care sequences were used as the basis for the flow analyses presented in Sankey charts and as independent variables in a generalized estimating equation (GEE) analysis.
Records of the CRC’s 24/7 urgent care and 23-hour observation unit were considered crisis facility records, in contrast to those of the CRC’s short-term inpatient unit, which was considered an inpatient facility. CRC records were consolidated into a single episode defined by the highest level of care if they met one of the following criteria: urgent care followed by observation, urgent care followed by observation followed by inpatient care, observation followed by inpatient care, and two or more episodes within 24 hours. A total of 41,026 crisis episodes were identified in the AHCCCS claims, of which 9,202 were matched with CRC records and consolidated, representing 5,530 unique individuals. Unmatched episodes represented either individuals who received no crisis facility services (e.g., mobile crisis or ED only) or individuals who received care at the other crisis facility or other inpatient units located in Pima County.
Dependent Variables
The crisis service reutilization outcome variable was defined as any new crisis service (mobile crisis, crisis facility, ED, or inpatient) with a start date within 30 days of the index crisis episode’s end date. The four crisis service categories were used for Sankey charts.
Independent Variables
Demographic variables, including sex, age, and race-ethnicity, were created on the basis of AHCCCS claims data. Homelessness status was based on the most recent documentation in the EHR. A variable for rural versus urban residence was created with the AHCCCS claim record of a patient’s address and the U.S. Census Bureau’s 2010 urban-rural classification definitions. Insurance status was simplified into a dichotomous variable, indicating enrollment (yes or no) with AHCCCS Medicaid, on the basis of the claims data.
Diagnosis variables were created on the basis of AHCCCS claims and the CCSR categories. A single categorical variable was created for mental disorders when used as the primary diagnosis, including anxiety disorder, bipolar disorder, depressive disorder, and psychotic disorder, or no diagnosis. Dichotomous variables were created when the claim included any diagnosis (including nonprimary) for alcohol use disorder, opioid use disorders, stimulant use disorders, and suicidality (on the basis of ICD-10 Z codes and clinical documentation). Clinical records indicating blood or urine toxicology positive for alcohol or methamphetamine were also incorporated into these dichotomous variables. We created a dichotomous variable to indicate whether the index episode started with mobile crisis services. Finally, we used EHRs to create a variable describing an individual’s legal status during the crisis facility visit: voluntary throughout, involuntary throughout, converted from involuntary to voluntary, or converted from voluntary to involuntary.
GEE Analysis
To account for potential correlations between outcomes for individuals with multiple crisis episodes, we used GEE analysis to create an overarching model of how the independent variables relate to 30-day reutilization. We calculated adjusted odds ratios (AORs) for each independent variable, controlling for other independent variables, with a confidence interval of 95% and p<0.05 as compared with the reference variable. Episodes with an ED end point were removed from the model because of issues with model convergence. Statistical analyses were conducted by using SAS, version 9.4. A human subjects research review was conducted by the Arizona State University Institutional Review Board (protocol 00011824).
Results
Crisis Episode Flow
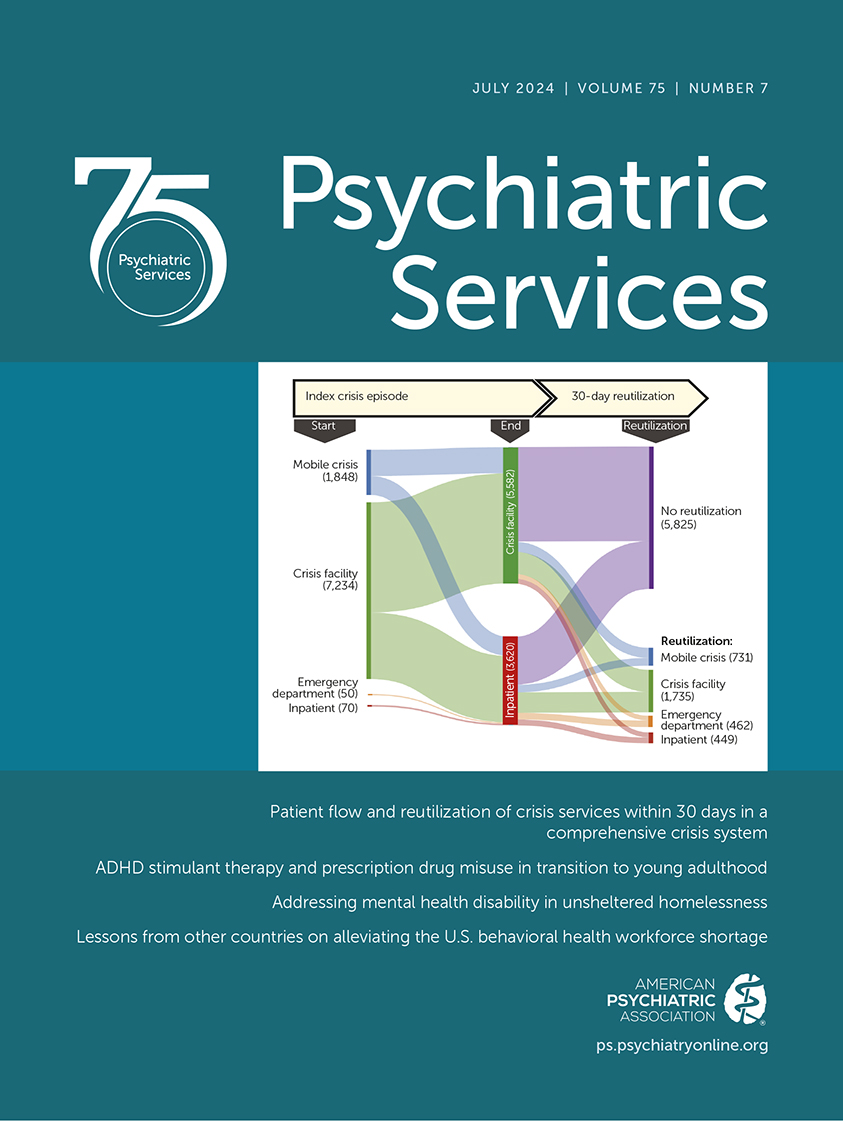
The flow analysis of AHCCCS claims included 41,026 crisis episodes (Figure 1A). Most episodes (N=23,547, 57.4%) began with mobile crisis or crisis facility services rather than ED or inpatient services. Of those episodes, 16,280 (69.1%) ended within the crisis system (mobile crisis or crisis facility). A total of 12,093 (29.5%) episodes ended at a crisis facility.
FIGURE 1. Crisis episode flow and 30-day reutilization of crisis servicesa
aA: starting points and end points of all crisis episodes (N=41,026) in Pima County, Arizona, during the study period; B: subset of individuals with crisis episodes (N=9,202) that included an encounter at the Crisis Response Center (CRC). These episodes were linked with CRC electronic health record data to create the generalized estimating equation model. Data source: Arizona Health Care Cost Containment System (AHCCCS). The Center for Health Information and Research at Arizona State University performed the analysis of AHCCCS data. The data that were used to construct these Sankey charts are included in the online supplement.
The analysis of 30-day reutilization for the subset of individuals who received crisis facility services at the CRC included 9,202 episodes (Figure 1B). Most CRC episodes (N=5,825, 63.3%) were not followed by 30-day reutilization. Of the 3,377 that were, most (N=2,466, 73.0%) occurred in a crisis setting—a specialized crisis facility (N=1,735, 51.4%) or mobile crisis unit (N=731, 21.6%)—rather than at the ED (N=462, 13.7%) or at an inpatient facility (N=449, 13.3%). Most of the episodes that began with an involuntary legal status ended with a voluntary status (N=1,700 of 2,865, 59.3%).
GEE Analysis
Demographic characteristics of the study population are shown in Table 1. AORs for demographic, clinical, and operational factors associated with 30-day reutilization are shown in Table 2 and discussed in the following text. (The working correlation matrix is included as a figure in the online supplement.)
| Characteristic | N | % |
|---|---|---|
| Sex | | |
| Male | 3,353 | 60.6 |
| Female | 2,177 | 39.4 |
| Age range (years) | | |
| 18–24 | 1,243 | 22.5 |
| 25–34 | 1,767 | 32.0 |
| 35–44 | 1,169 | 21.1 |
| 45–54 | 839 | 15.2 |
| 55–64 | 512 | 9.3 |
| Race and ethnicity | | |
| Non-Hispanic White | 2,461 | 44.5 |
| Hispanic/Latino | 1,780 | 32.2 |
| Black/African American | 408 | 7.4 |
| Native American | 300 | 5.4 |
| Asian/Pacific Islander | 61 | 1.1 |
| Other | 520 | 9.4 |
TABLE 1. Baseline characteristics for the study population of individuals who received care at the Crisis Response Center (N=5,530)
| Demographic factors | N of episodes | AOR | 95% CI |
|---|---|---|---|
| Sex | | | |
| Female (reference) | 3,419 | | |
| Male | 5,783 | 1.29*** | 1.13–1.47 |
| Age range (years) | | | |
| 18–24 (reference) | 1,863 | | |
| 25–34 | 3,087 | 1.17 | .98–1.40 |
| 35–44 | 2,036 | 1.29** | 1.06–1.56 |
| 45–54 | 1,379 | 1.23 | 1.00–1.52 |
| 55–64 | 837 | 1.01 | .80–1.29 |
| Race and ethnicity | | | |
| Non-Hispanic White (reference) | 4,151 | | |
| Hispanic/Latino | 2,896 | .91 | .79–1.04 |
| Black/African American | 812 | 1.31* | 1.03–1.65 |
| Native American | 528 | 1.19 | .93–1.53 |
| Asian/Pacific Islander | 98 | .74 | .41–1.32 |
| Other | 717 | .89 | .69–1.14 |
| Urban vs. rural residence | | | |
| Rural (reference) | 1,005 | | |
| Urban | 8,197 | 1.04 | .87–1.25 |
| Homeless | | | |
| No (reference) | 6,563 | | |
| Yes | 2,639 | 2.00*** | 1.75–2.28 |
| Payer | | | |
| Other (reference) | 2,634 | | |
| Medicaid/AHCCCS | 6,568 | 1.72*** | 1.46–2.02 |
| Clinical factors | | | |
| Alcohol use disorder | | | |
| No (reference) | 7,291 | | |
| Yes | 1,911 | 1.12 | .99–1.28 |
| Opioid use disorder | | | |
| No (reference) | 8,452 | | |
| Yes | 750 | .91 | .75–1.10 |
| Stimulant use | | | |
| No (reference) | 6,818 | | |
| Yes | 2,384 | 1.27*** | 1.11–1.45 |
| Suicidality | | | |
| No (reference) | 7,912 | | |
| Yes | 1,290 | .93 | .79–1.09 |
| Psychiatric diagnosis | | | |
| None (reference) | 2,724 | | |
| Psychotic disorder | 2,541 | 1.30** | 1.11–1.52 |
| Depressive disorder | 1,443 | .74** | .62–.89 |
| Bipolar disorder | 907 | 1.01 | .82–1.25 |
| Trauma | 1,412 | .52*** | .42–.64 |
| Anxiety disorder | 175 | .67 | .42–1.06 |
| Operational factors | | | |
| Index episode starting point | | | |
| Other (reference) | 7,354 | | |
| Mobile crisis | 1,848 | 1.21** | 1.06–1.38 |
| Index episode end point | | | |
| Crisis facility (reference) | 5,582 | | |
| Inpatient | 3,620 | 1.27*** | 1.12–1.45 |
| Legal status | | | |
| Voluntary throughout (reference) | 5,970 | | |
| Converted to involuntary | 367 | .86 | .65–1.14 |
| Involuntary throughout | 1,165 | .80* | .67–.95 |
| Converted to voluntary | 1,700 | .86* | .75–.99 |
TABLE 2. Adjusted odds ratios (AORs) for factors associated with crisis service reutilization within 30 days of the end of an index episode (N=9,202 index episodes)
Demographic factors.
We found significantly elevated odds of 30-day reutilization among men (vs. women; AOR=1.29), people ages 35–44 (vs. people ages 18–25; AOR=1.29); Black people (vs. White people; AOR=1.31), and people experiencing homelessness (AOR=2.00). Crisis episodes of people who were insured by AHCCCS Medicaid appeared to be associated with higher odds of 30-day reutilization, although interpretation of this finding is limited by payer policies in Arizona that may result in an undercount of inpatient and ED reutilization episodes among non-AHCCCS beneficiaries. There were no significant differences among people in older age groups, other racial or ethnic groups, or urban versus rural areas.
Clinical factors.
Significantly elevated odds of 30-day reutilization were seen for episodes that included a diagnosis of psychotic disorder (AOR=1.30) or stimulant use (AOR=1.27)—which primarily involved methamphetamine—and significantly lower odds of 30-day reutilization were seen for depression (AOR=0.74) and trauma (AOR=0.52). There were no statistically significant differences for anxiety, bipolar disorder, alcohol use disorder, opioid use disorder, or suicidality.
Operational factors.
Significantly elevated odds of 30-day reutilization were seen for episodes beginning with mobile crisis services (vs. any other starting point; AOR=1.21) and for episodes ending with inpatient care (AOR=1.27), compared with episodes with a crisis facility end point. We observed significantly lower odds of 30-day reutilization for episodes of people with an involuntary legal status throughout a crisis facility visit (AOR=0.80) and when legal status was converted from involuntary to voluntary (AOR=0.86), compared with episodes of people with a voluntary legal status throughout a crisis facility visit. There was no statistically significant difference between episodes of people whose legal status was changed from voluntary to involuntary compared with those of people whose status was voluntary throughout a crisis facility visit.
Discussion
In this study, we examined crisis services in one county within the Arizona crisis system, considered a model to inform crisis service development across the United States. We found that a majority of crisis episodes occurred in crisis settings rather than in the ED or inpatient settings. Most crisis episodes were not followed by service reutilization within 30 days; of those that were, most occurred in crisis settings rather than in the ED or inpatient settings. These findings are promising in that they illustrate the potential for crisis systems to divert people from more restrictive and costly levels of care, which has important implications for improving patient experience, ED overcrowding, and inpatient utilization. Furthermore, deployment of clinical mobile crisis teams provides an alternative to police responses and results in a more person-centered clinical service, decriminalizes mental illness, and allows law enforcement to focus resources elsewhere.
This study identified multiple factors that were statistically significantly correlated with 30-day reutilization after receipt of facility-based crisis services. Black race was the only racial-ethnic group identified as having significantly higher odds of 30-day reutilization. This finding is congruent with the social and structural inequities that contribute to poor mental health outcomes among Black people generally and underscores the need for crisis programs to invest in services that proactively provide outreach to Black populations and are culturally adapted to promote engagement (15, 16). Homelessness was also associated with higher odds of 30-day reutilization, which is unsurprising given that housing instability has been shown to negatively affect mental health and service use. This finding further highlights the need for structural solutions such as expanding affordable and permanent supportive housing (17).
Reutilization was associated with stimulant use, which in this study primarily constituted methamphetamine use. ED visits for methamphetamine use have steadily grown over the past decade (18, 19), and relapse rates are high (20). Once in the ED, these individuals are more likely to be restrained and have longer lengths of stay compared with other ED patients (21, 22). Individuals who use stimulants may have a better experience in a crisis facility that is designed and staffed to manage acute agitation and connect them to outpatient substance use disorder services—but even with these specialized resources, we found that these individuals have increased odds of 30-day reutilization, underscoring the difficulty in treating this population and the need for more effective interventions.
People with a diagnosis of psychotic disorder (which could include primary psychotic illnesses, substance-induced psychosis, or both) were found to have an increased likelihood of 30-day reutilization. Prior studies have shown that both schizophrenia and substance-induced psychosis are associated with increased ED utilization (23–25). The lower likelihood of 30-day reutilization after episodes involving depression and trauma-related disorders may reflect more effective treatments or better connection to outpatient resources in these groups.
Crisis episodes beginning with mobile crisis care had a higher risk for 30-day reutilization, which illustrates the complexity of interpreting crisis service reutilization as an outcome measure (26). Crisis services aim to develop a stabilization and aftercare plan in which the individual’s needs are met without the need for further crisis intervention. However, people in crisis should be encouraged to seek help when needed, with crisis services providing access to care in settings that are less restrictive and less costly than EDs and hospitals. Studies show that individuals and families prefer clinical mobile crisis teams to police responses (27), and our findings suggest that individuals who have received mobile crisis services are willing to seek these services again. Episodes that ended with inpatient care also had an increased risk for 30-day reutilization, which may reflect higher illness severity.
This study presents a novel approach to describing involuntary treatment, which is substantially understudied (28). Involuntary detention can be a controversial intervention because of the complex intersection of legal, clinical, and ethical concerns. Statutory differences across states make national tracking difficult, but some estimates suggest that there are as many as 1 million involuntary psychiatric detentions annually, with disproportionately higher use among Black individuals (28, 29). Crisis facilities are in a position to make determinations on whether an involuntary detention should be continued, and conversion to voluntary status has been recommended as an outcome measure for crisis services (26, 30). In this study, most episodes in which individuals began their crisis facility visit with an involuntary legal status ended with a conversion to voluntary status, and we observed a decreased likelihood of 30-day reutilization among both those who converted to voluntary status and those who had an involuntary status throughout a crisis facility visit. This finding may reflect effective evaluation and treatment of the involuntary population in the crisis setting, but further study is needed to investigate alternative explanations such as avoidance of future care seeking because of the overall experience of the involuntary detention process.
Our study had several limitations. Administrative data such as Medicaid claims are intrinsically limited by potential biases such as miscoding, the use of diagnoses to justify billing, underutilization of ICD-10 diagnosis codes for substance use disorders or Z codes for suicidality, and the inability to describe non-Medicaid services. For example, AHCCCS pays for the first 24–72 hours of crisis care regardless of a person’s type of insurance, but subsequent ED or inpatient services are billed to other payers, so it is possible that Medicaid beneficiaries are overrepresented in higher levels of care and 30-day reutilization episodes.
We used a mutually adjusted model because our primary objective was to provide an encompassing view of the patient flow through the crisis system, where factors often operate concurrently rather than in isolation. However, we recognize that demographic factors such as age, race-ethnicity, homelessness, and so forth intersect in complex ways and that a mutual adjustment may lead to a misleading measure of effects for each individual factor. In addition, in our analysis, we used a single outcome variable in which the use of any of the four services (mobile crisis, crisis facility, ED, or inpatient) counted as reutilization. It is likely that different factors are associated with the use of each type of service, and future studies exploring these differences would be worthwhile. We also did not include data on the use of outpatient services before or after a crisis episode. Such an analysis would further our understanding of the factors associated with crisis service utilization, including potential disparities in access to outpatient care, and should be explored in future studies. Other future analyses might examine interaction terms between variables of interest to obtain a further understanding of how these factors are associated with service reutilization. The inclusion of additional data to allow for the analysis of factors such as police involvement, ED and inpatient lengths of stay, episode costs, and outpatient utilization would also be of major interest.
The reutilization analysis included only individuals who had a crisis facility or inpatient claim at the CRC. Single-site EHR data can be limited by a lack of generalizability and selection bias. To investigate possible differences between populations discharged from other crisis facilities, we conducted a preliminary analysis comparing the CRC with the other crisis facility in Pima County and found lower 30-day reutilization among those who were discharged from the CRC (see the online supplement). However, it is difficult to fully interpret these findings without further analysis.
Finally, the results of our cross-sectional observational study describe how individuals flow through the crisis system and identify factors associated with 30-day reutilization, but we cannot establish a causative effect on these outcomes.
Conclusions
The Arizona crisis system serves a large proportion of individuals experiencing emergencies related to mental disorders or substance use disorders. The utilization of crisis services in lieu of more costly and restrictive levels of care has potential benefits such as reducing ED overcrowding, lessening demand for inpatient beds, and improving patient experience. The use of mobile crisis teams presents an alternative to law enforcement involvement, contributing to decriminalization of mental illness and allowing law enforcement to focus their resources elsewhere. Demographic, clinical, and operational factors that are associated with 30-day reutilization of crisis services have important implications for future program design and implementation, and they highlight the need for further research aimed at informing crisis system administrators and policy makers who are committed to increasing access to these critical safety-net services.
1. : Trends in Emergency Department Visits Involving Mental and Substance Use Disorders, 2006–2013. Healthcare Cost and Utilization Project Statistical Brief no 216. Rockville, MD, Agency for Healthcare Research and Quality, 2016. https://hcup-us.ahrq.gov/reports/statbriefs/sb216-Mental-Substance-Use-Disorder-ED-Visit-Trends.pdf Google Scholar
2. : Characteristics of adult psychiatric patients with stays of 24 hours or more in the emergency department. Psychiatr Serv 2012; 63:283–286Link, Google Scholar
3. : Disparities in care: the role of race on the utilization of physical restraints in the emergency setting. Acad Emerg Med 2020; 27:943–950Crossref, Medline, Google Scholar
4. : Deaths of people with mental illness during interactions with law enforcement. Int J Law Psychiatry 2018; 58:110–116Crossref, Medline, Google Scholar
5. National Guidelines for Behavioral Health Crisis Care—A Best Practice Toolkit. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2020. https://www.samhsa.gov/sites/default/files/national-guidelines-for-behavioral-health-crisis-care-02242020.pdf Google Scholar
6. : Roadmap to the Ideal Crisis System. Washington, DC, National Council for Mental Wellbeing, 2021. https://www.thenationalcouncil.org/wp-content/uploads/2022/02/042721_GAP_CrisisReport.pdf Google Scholar
7. : Effects of a dedicated regional psychiatric emergency service on boarding of psychiatric patients in area emergency departments. West J Emerg Med 2014; 15:1–6Crossref, Medline, Google Scholar
8. : The Banner Psychiatric Center: a model for providing psychiatric crisis care to the community while easing behavioral health holds in emergency departments. Perm J 2013; 17:45–49Crossref, Medline, Google Scholar
9. : A specialized crisis response site as a core element of police-based diversion programs. Psychiatr Serv 2001; 52:219–222Link, Google Scholar
10. : Cops, clinicians, or both? Collaborative approaches to responding to behavioral health emergencies. Psychiatr Serv 2022; 73:658–669Link, Google Scholar
11. AZ600 Statewide Dashboard. Tempe, AZ, Solari Crisis and Human Services, 2022. https://public.tableau.com/app/profile/crisis.network/viz/AZ600StatewideDashboard/AZ600StatewideDashboard. Accessed Oct 3, 2023 Google Scholar
12. Quick Facts: Pima County, Arizona. Washington, DC, US Census Bureau, 2023. https://www.census.gov/quickfacts/fact/table/pimacountyarizona. Accessed Oct 2, 2023 Google Scholar
13. Behavioral health crisis services and care coordination; in AHCCCS Medical Policy Manual. Phoenix, Arizona Health Care Cost Containment System, 2023. https://www.azahcccs.gov/shared/Downloads/MedicalPolicyManual/500/590.pdf Google Scholar
14. Funding 988 and the Arizona Crisis System. Phoenix, Arizona Health Care Cost Containment System, 2021. https://www.azahcccs.gov/AHCCCS/Downloads/Funding988AndArizonaCrisisSystem.pdf Google Scholar
15. : Effect of racial and ethnic composition of neighborhoods in San Francisco on rates of mental health–related 911 calls. Psychiatr Serv 2009; 60:1376–1378Link, Google Scholar
16. : Centering equity in mental health crisis services. World Psychiatry 2022; 21:243–244Crossref, Medline, Google Scholar
17. : Substance use, homelessness, mental illness and Medicaid coverage: a set-up for high emergency department utilization. West J Emerg Med 2018; 19:902–906Crossref, Medline, Google Scholar
18. Drug Abuse Warning Network, 2011: National Estimates of Drug-Related Emergency Department Visits. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2013. https://www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf Google Scholar
19. Drug Abuse Warning Network: Findings From Drug-Related Emergency Department Visits, 2021. Rockville, MD, Substance Abuse and Mental Health Services Administration, 2022. https://store.samhsa.gov/sites/default/files/pep22-07-03-002.pdf Google Scholar
20. : Time to relapse following treatment for methamphetamine use: a long-term perspective on patterns and predictors. Drug Alcohol Depend 2014; 139:18–25Crossref, Medline, Google Scholar
21. : High resource utilization of psychiatric emergency services by methamphetamine users. Hawaii J Med Public Health 2018; 77:312–314Medline, Google Scholar
22. : Rates and features of methamphetamine-related presentations to emergency departments: an integrative literature review. J Clin Nurs 2018; 27:2569–2582Crossref, Medline, Google Scholar
23. : Psychosis among individuals with methamphetamine use disorder is associated with elevated rates of hospitalizations and emergency department visits across an academic health care system. J Subst Use Addict Treat 2023; 151:209033Crossref, Medline, Google Scholar
24. : Serious mental illness and health-related factors associated with regional emergency department utilization. Popul Health Manag 2020; 23:430–437Crossref, Medline, Google Scholar
25. : What is the risk of returning to the emergency department within 30 days for patients diagnosed with substance-induced psychosis? CJEM 2022; 24:702–709Crossref, Medline, Google Scholar
26. Quality Measurement in Crisis Services. Washington, DC, National Council for Mental Wellbeing, 2023. https://www.thenationalcouncil.org/wp-content/uploads/2023/01/23.01.13_Quality-Measurement-in-Crisis-Services.pdf Google Scholar
27. : Crisis response model preferences of mental health care clients with prior misdemeanor arrests and of their family and friends. Psychiatr Serv 2023; 74:1163–1170Link, Google Scholar
28. : Taking an evidence-based approach to involuntary psychiatric hospitalization. Psychiatr Serv 2023; 74:431–433Link, Google Scholar
29. : Incidences of involuntary psychiatric detentions in 25 US states. Psychiatr Serv 2021; 72:61–68Link, Google Scholar
30. : Crisis Reliability Indicators Supporting Emergency Services (CRISES): a framework for developing performance measures for behavioral health crisis and psychiatric emergency programs. Community Ment Health J 2016; 52:1–9Crossref, Medline, Google Scholar