Legislation Extending Medicaid, Medicare Coverage to Disabled People Who Work Wins Approval in Congress
Legislation that allows persons with mental and physical disabilities to continue to receive Medicaid or Medicare coverage after they return to work was passed overwhelmingly by Congress shortly before it adjourned in November. Passage of such legislation was a major recommendation of the Presidential Task Force on Employment of Adults With Disabilities (see the February 1999 issue, page 279), and President Clinton included funding for it in his fiscal year 2000 budget proposal to Congress.
Titled the Ticket to Work and Work Incentives Improvement Act, the law permits states to increase the level of income that disabled persons can earn before they become ineligible for Medicaid coverage. It also extends the period during which disabled persons who are employed can continue to receive Medicare coverage and raises the level of income they can earn. The expanded coverage becomes effective October 1, 2000.
To extend Medicaid coverage, the law builds on a provision in the 1997 Balanced Budget Act that allows states to offer employed people with disabilities the opportunity to buy Medicaid coverage if they would be eligible for Supplemental Security Income (SSI) benefits except for their income.
States can set income limits and require cost-sharing for premiums, based on income, on a sliding scale up to the full premium amount. Individuals can earn income of more than 250 percent above the poverty level, the previous maximum allowed before becoming ineligible for coverage. However, those earning between 250 percent and 450 percent of the poverty level may be required to pay 100 percent of the Medicaid premium as long as the premiums do not exceed 7.5 percent of their total income.
States must require 100 percent payment for Medicaid premiums for individuals with adjusted gross incomes of more than $75,000 unless they choose to subsidize the premiums using their own funds. States may also cover people who continue to have a severe medical impairment but lose eligibility for disability benefits under the SSI and Social Security Disability Insurance (SSDI) programs because their medical condition improves.
The law extends Medicare coverage beyond the current four-year maximum and permits coverage for an additional four and a half years for disabled people who return to work and earn more than $700 a month, the maximum previously allowed for SSDI beneficiaries after a nine-month trial work period. Previously SSDI beneficiaries could continue to receive Medicare coverage for 39 weeks beyond the nine-month period, but afterward they had to pay the full Medicare premium.
The law also creates a Ticket to Work and Self-Sufficiency program to provide persons who are receiving SSDI or SSI with a "ticket" they may use to obtain vocational rehabilitation services of their choice from an employment network to enable them to enter the workforce. State vocational rehabilitation agencies have the option of participating in the program as an employment network or remaining in the current reimbursement system.
In addition, the law establishes an outreach program under the Social Security Administration (SSA) to provide information on work incentives to people with disabilities as well as an assistance program to help people gain access to work incentives. It authorizes up to $23 million annually through fiscal year 2004 to provide grants to states or private organizations for the outreach program. It also authorizes the SSA commissioner to make grants of up to $7 million annually through 2004 to advocacy organizations to provide information to help individuals obtain vocational rehabilitation and employment services.
The law also authorizes demonstration programs that gradually reduce cash benefits as earnings increase and that allow states to extend Medicaid coverage to workers who have a disability that, without health care, will become severe enough to qualify them for SSI or SSDI.
Disability groups have estimated that about two million of the eight million working-age adults who receive disability benefits will forgo those payments and take jobs as a result of the new law, the Washington Post reported. An aide to Senator Edward M. Kennedy (D.-Mass.), a sponsor of the legislation, told the Post that the estimated cost of the program would be recouped if only 70,000 people took jobs. If three times as many did so, the government could save $1 billion annually in disability payments.
Research Funds for Mental Illness and Substance Abuse Are Increased by 14 Percent
Federal funding for research on mental illness and substance abuse within the National Institutes of Health (NIH) will increase by almost 14 percent in fiscal year 2000 under an appropriations measure approved by Congress last November. Funding for programs operating under the Substance Abuse and Mental Health Services Administration (SAMHSA) will increase by almost 7 percent.
Like most other federal programs, the NIH and SAMHSA programs will be subject to a .38 percent across-the-board funding cut to be imposed later this year, a concession made by President Clinton to win Congress' approval of the bill. Agency directors will have the latitude to decide how the funding reduction will be applied to their programs. Some programs may receive no cuts, while others may be cut by more than .38 percent. However, in no case can a program's funding be cut by more than 15 percent.
Table 1 shows the level of funding for federal mental health and substance abuse programs for fiscal years 1999 and 2000. The additional funding for the three NIH institutes—the National Institute of Mental Health, the National Institute on Alcohol Abuse and Alcoholism, and the National Institute on Drug Abuse—followed funding increases of around 15 percent in fiscal year 1999. As a result, the budget of each of the research institutes has grown by around 30 percent over the two-year period. The fiscal 2000 funding levels greatly exceeded the 2.5 percent average increases proposed by President Clinton in the budget he presented to Congress.
SAMHSA's Center for Mental Health Services (CMHS) also received a significant influx of new funding in its Knowledge Development and Application Program and mental health block grant to states, increasing the total CMHS fiscal 2000 budget by almost 24 percent. Funds for the block grant were increased by more than $67 million, close to the amount requested by President Clinton to boost spending on community mental health services.
Funding for the CMHS Knowledge Development program was increased by more than $42 million, almost 44 percent above fiscal 1999. Congress doubled the funding for mental health services for school-age children as part of an effort to reduce school violence and specified that $80 million of the $139 million appropriation be used for the support and delivery of school-based and school-related mental health services for school-age youth.
SAMHSA's Center for Substance Abuse Treatment received a funding increase of almost $44 million in its Knowledge Development and Application program, almost 26 percent above the 1999 level. Congress requested that most of the additional funds be used to strengthen substance abuse treatment capacity in minority communities disproportionately affected by the HIV-AIDS epidemic.
The Knowledge Development and Application program of the Center for Substance Abuse Prevention received the only funding cut among the SAMHSA programs. The cut totaled almost $16 million but was substantially less than the $26 million requested by President Clinton.
APA Publishes Revised Practice Guideline for Treating Eating Disorders
A revised version of a practice guideline for treating patients who have eating disorders was published this month by the American Psychiatric Association (APA). The original guideline on eating disorders, published in 1993, was the first in APA's series of practice guidelines, which now number 11. The guideline focuses on the treatment of anorexia nervosa and bulimia nervosa.
According to the guideline, the lifetime prevalence of anorexia among women has been found to range between .5 percent and 3.7 percent. The rate for bulimia ranges between 1.1 percent and 4.2 percent. Although research evidence suggests that the prevalence of bulimia in the U.S. has decreased slightly in recent years, the guideline notes that eating disorders appear to be increasing in other countries, even in cultures in which the disorders are rare. Prevalence rates in Japan are comparable to U.S. rates, and rates are rising among Chinese women exposed to modernization in cities such as Hong Kong.
According to the guideline, psychiatric management has six major components. The psychiatrist should establish and maintain a therapeutic alliance; coordinate care and collaborate with other clinicians; assess and monitor symptoms and behaviors related to the eating disorder, the patient's general medical condition, and psychiatric status and safety; and provide family assessment and treatment. The guideline emphasizes that eating disorders are often long-term illnesses, requiring the psychiatrist to adapt and modify therapeutic strategies over time. It warns clinicians that the challenges presented by working with these patients often stir profound countertransference feelings, especially the feeling that the clinician has not done enough to alleviate the patient's plight.
The guideline reviews treatment principles for both disorders, including nutritional rehabilitation and counseling. Because comorbid depression occurs in 50 to 75 percent of patients with eating disorders, the use of antidepressants is reviewed. For anorexia, the guideline suggests a role for antidepressants after the patient gains weight and the psychological effects of malnutrition are resolving. For patients with bulimia nervosa, the guideline recommends antidepressants during initial treatment.
The new edition of the eating disorders guideline represents APA's efforts to ensure that the guidelines reflect current and effective practices. Each guideline is developed by an APA workgroup and is extensively reviewed by other psychiatrists and representatives of related fields. The revised guideline was approved in July 1999 by the APA board of trustees. It was published as a supplement to the January issue of the American Journal of Psychiatry.
NEWS BRIEFS
NAPHS move: Following up on a collaboration agreement signed early in 1999 by the National Association of Psychiatric Health Systems (NAPHS) and the American Hospital Association (AHA), on December 1 NAPHS moved its offices to the same building that houses the AHA offices in Washington, D.C. The new address is 325 Seventh Street, N.W., Suite 625, Washington, D.C. 20004. The phone number (202-393-6700) and fax number (202-783-6041) remain the same. The organizations have agreed to collaborate in several areas, including policy development, information and data resources, and quality of care.
Tobacco Use Research Centers: The National Cancer Institute (NCI) and the National Institute on Drug Abuse (NIDA) have awarded grants totaling $14.5 million to create the Transdisciplinary Tobacco Use Research Centers for studying tobacco use and new ways to combat it and its consequences. Together NCI and NIDA will spend about $70 million on the centers over five years, and the Robert Wood Johnson Foundation has committed an additional $14 million over that period. The centers will be located at the Brown University Center for Behavioral and Preventive Medicine at the Miriam Hospital in Providence, Rhode Island; the University of California at Irvine; the University of Southern California in Los Angeles; Georgetown University in Washington, D.C.; the University of Minnesota in Minneapolis; the University of Wisconsin Medical School in Madison; and Yale University in New Haven, Connecticut.
PEOPLE & PLACES
Awards: Robert Cancro, M.D., D.Sc., was presented with the 1999 Irving Blumberg Human Rights Award from the American Association of Psychosocial Rehabilitation at the association's meeting in New York City in November. Dr. Cancro is professor and chairman of the department of Psychiatry at New York University Medical Center and director of the Nathan S. Kline Institute for Psychiatric Research in Orangeburg, New York. At New York University, he established the first required residency training rotation in psychiatric rehabilitation.
The Deaf and Hard of Hearing Program of the South Carolina Department of Mental Health placed 11th overall in the 1999 Innovations in American Government Awards Program funded by the Ford Foundation and administered by the John F. Kennedy School of Government at Harvard University. More than 1,600 local, state, federal, and tribal government entities entered the 1999 competition. Barry Critchfield, Ph.D., is director of the program, which provides treatment to more than 400 clients annually.
Death: Jeanne M. Spurlock, M.D., 78, a child psychiatrist who served as deputy medical director and director of the office of minority-national affairs for the American Psychiatric Association from 1974 until her retirement in 1991, died November 25, 1999, in Washington, D.C., of surgical complications. Before joining the APA staff, Dr. Spurlock was chair of the department of psychiatry at Meharry Medical College in Nashville, Tennessee. She was the author, coauthor, or editor of more than 30 books. The most recent, Black Psychiatrists and American Psychiatry, was published in 1999.
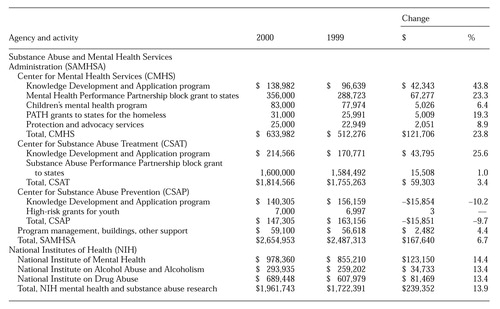 |
Table 1. Appropriations for federal mental health and substance abuse programs for fiscal 1999 and 2000 and change from fiscal 1999, in millions of dollars



