Involuntary First Admission of Patients With Schizophrenia as a Predictor of Future Admissions
Abstract
OBJECTIVE: The extent to which the legal status of a first psychiatric admission—voluntary or involuntary—predicted the legal status and number of future admissions was examined among patients with schizophrenia. METHODS: Data on all patients in Israel who had a nonforensic first admission between 1978 and 1992 and a diagnosis of schizophrenia (N=9,081) were extracted from the national psychiatric hospitalization case registry. Also obtained from the registry was information about the patients' subsequent hospitalizations through 1995, demographic data, and diagnosis. Analyses adjusted for time since first admission, age at first admission, country of origin, and religion. RESULTS: The first admission of 12.9 percent of the patients was involuntary. The legal status of the first admission was not related to the number of readmissions. However, female patients whose first admission was involuntary were 4.1 times more likely to have an involuntary second admission than female patients whose first admission was voluntary; these odds were 3.4 for males. Further analysis examined the percentage of involuntary admissions among all hospitalizations of the 3,420 patients who had four or more admissions (chronic patients). Among the chronic patients who had an involuntary first admission, 41 percent of subsequent admissions were involuntary. This figure was significantly lower among the chronic patients who had a voluntary first admission—13 percent. The percentage of involuntary admissions was not related to the number of admissions. CONCLUSIONS: The strong association of involuntary legal status at first admission with involuntary status at second admission and with the number of involuntary admissions over time suggests that involuntary first admission might be an important factor in assessing whether patients are likely to be readmitted involuntarily
Involuntary admission to a psychiatric hospital is an extreme life event. For persons with schizophrenia, whose illness is life long, the first encounter with the psychiatric system may be a crucial factor in their future psychiatric career. Previous studies have focused on the differences between patients admitted voluntarily and involuntarily (1,2). However, the extent to which involuntary first admission predicts future admissions has not been widely examined.
The one study that we were able to locate that addressed this issue did so by retrospectively examining data over an 11-year period on 53 first-admission patients with a diagnosis of schizophrenia (3). After the first admission, 12 percent of their total admissions during the 11 years were involuntary. Involuntary admissions were more frequent in the first half of the follow-up period and were more likely among patients with a previous involuntary admission.
The goal of the study reported here was to examine the extent to which the type of first psychiatric hospital admission for schizophrenia—either voluntary or involuntary—predicted the type and number of subsequent admissions.
Methods
The study used the Israel national psychiatric hospitalization case registry, which is a complete listing of all psychiatric admissions in Israel since 1950. All inpatient facilities are legally mandated to report psychiatric admissions to the registry, which is run by the Israel Ministry of Health. Data were obtained on all patients with first admissions between 1978 and 1992 who had a discharge diagnosis of schizophrenia.
The registry includes dates and legal status (voluntary or involuntary) of all inpatient admissions and discharges, as well as diagnosis and demographic data. For this study we excluded persons who emigrated to Israel after age 16, because they may have had psychiatric admissions before immigrating and those admissions would not appear in the registry. Patients were followed in the registry through the end of 1995.
Sample
The initial dataset extracted from the registry included data for 12,071 patients. From this total, we excluded data for 745 patients who died during the follow-up period and for 49 patients who were not discharged from their first admission. We excluded data for patients whose first admission was neither a civil commitment nor a voluntary commitment; these excluded data represented 559 patients whose commitments were court ordered, 1,323 patients for whom information about commitment status was missing, and 314 patients who had another type of noncivil commitment.
The final dataset included data on 9,081 patients, of whom 58.2 percent (N=5,287) were males, 87.7 percent (N=7,830) were Jewish, 75.6 percent (N=6,863) were born in Israel, and 24.7 percent (N=2,246) were married.
The mean±SD age at first admission of males was 25.33±7.70 years (median, 24 years), and for females it was 27.36±9.42 (median, 26 years). The mean±SD total number of hospitalizations per patient was 4.32±4.52 (median, three hospitalizations), and the mean number of involuntary hospitalizations was .73±1.32 (median, one hospitalization).
Over the study period, the 9,081 patients had a total of 39,228 admissions (including the first admission). Of this total, 16.9 percent (N=6,622) were involuntary admissions. The mean±SD length of follow-up (from first admission until the end of 1995) was 9.6±4.07 years (median, ten years).
Analysis
The analyses examined the extent to which the type of first admission (voluntary or involuntary) was associated with the number and type of subsequent admissions. The first round of analysis employed analysis of variance (ANOVA) to determine whether the type of first admission predicted the number of subsequent admissions. Chi square analysis was also used to examine the chance of readmission. Chi square analysis, risk statistics, and logistic regression were used to determine whether the type of second admission could be predicted from the type of first admission. Separate logistic regression models were estimated for males and females, controlling for age at first admission, number of years since first admission, immigrant versus nonimmigrant status, marital status, and religion.
The second round of analysis focused on chronic patients, or the 3,420 patients in the sample with four or more admissions (including the first admission). It examined the relationship between legal status at first admission and the percentage of total involuntary admissions [(the number of involuntary admissions/the number of admissions) x 100]. Data for patients with three admissions or fewer were excluded; 2,521 patients had only one admission (the first admission); 1,606 patients had two admissions; and 1,180 patients had three admissions. Also excluded were data for 354 patients whose second admission was neither a civil commitment nor a voluntary admission; 121 of these patients were court ordered, 72 had another type of noncivil commitment, and in 161 cases the legal status was unknown.
In the second round of data analysis, we used simple factorial ANOVA and controlled for sex, age at first admission, number of years since first admission, religion, and whether or not a patient was an immigrant. In addition, the correlation between the percentage of involuntary hospitalizations and the total number of hospitalizations was calculated to see if the percentage of involuntary admissions was related to the number of admissions.
To control for multiple comparisons, and the very large sample size, which inflates the statistical significance of small differences, significance levels for all analyses were set a priori at .005.
Results
In the sample of 9,081 patients, the first admission of 1,172 patients, or 12.9 percent, was involuntary. No significant difference was found in the number of total admissions between the 1,172 patients whose first admission was involuntary and the 7,909 patients whose first admission was voluntary (mean±SD number of admissions=4.2±4.17 and 4.34±4.57, respectively). This finding was further tested with a simple factorial ANOVA that controlled for gender, marital status, religion, immigrant versus nonimmigrant status, age at first admission, and time since first admission. This analysis found no significant main effect for type of first admission.
In addition, no significant difference was found between the groups with voluntary and involuntary first admissions in the percentage of patients who had no subsequent admissions. In the group of 7,909 patients who had a voluntary first admission, 2,211 patients, or 28 percent, had only one admission. Of the 1,172 patients who had an involuntary first admission, 310 patients, or 26.5 percent, had only one admission.
We examined the extent to which an involuntary first admission predicted an involuntary second admission. This analysis excluded data for the 2,521 of the 9,081 study patients who had no second admission. Of the remaining 6,560 patients, 345 whose second admission was neither a civil nor a voluntary commitment and 246 for whom legal status was unknown were excluded, leaving a total of 5,969 patients.
Of the 732 patients with an involuntary first admission who had a second admission, 232 (31.7 percent) had a second admission that was also involuntary. Of the 5,237 patients with a voluntary first admission who had a second admission, 541 (10.3 percent) had a second admission that was involuntary. Thus the odds of being hospitalized involuntarily on the second admission were 4.03 times greater for those hospitalized involuntarily on the first admission than for those hospitalized voluntarily on the first admission (95 percent confidence interval=3.37 to 4.82).
To test for potentially important control variables, bivariate analysis was done. It revealed that the legal status of the second admission of the 5,969 patients who had a second admission was not related to marital status or to being born in Israel as opposed to another country. On the other hand, males were more likely than females to have an involuntary second admission (OR=1.4, CI=1.15 to 1.59; (2=13.8, df=1, p<.001). Of the 3,470 patients who were male in the group of 5,969 patients, 472 patients, or 13.6 percent, had an involuntary second admission. Of the 2,499 patients who were female in this group, 260 patients, or 10.4 percent, had an involuntary second admission.
Jews were more likely than non-Jews to have an involuntary second admission (OR=1.69, CI=1.3 to 2.3; (2=12.3, df=1, p<.001). Of the 5,291 Jews with at least two admissions, 675, or 12.8 percent, had an involuntary second admission. Of the 641 non-Jews, 51, or 8 percent, had an involuntary second admission. In addition, those whose second admission was involuntary were older at the time of their first admission than those whose second admission was voluntary (mean±SD age of 27.0±8.3 years versus 25.3±8.15 years; F= 26.12, df=1, 5,964, p<.001).
As a multivariate test of the relationship between legal status of first and second admissions, separate logistic regression models were estimated for males and females. The models adjusted for time since first admission, age at first admission, and religion. The models revealed that females who were first admitted involuntarily were 4.1 times more likely than those admitted voluntarily to have a second admission that was involuntary (CI=3.0 to 5.6); for males these odds were 3.4 (CI=2.7 to 4.3).
Among 3,420 chronic patients, or those with at least four admissions (including the first admission), we tested the relationship between legal status of first admission and percentage of total involuntary admissions. Table 1 presents the results of a simple factorial ANOVA, which adjusted for sex, marital status, religion, age at first admission, and immigration status. Among the 421 chronic patients whose first admission was involuntary, 41 percent of subsequent admissions were involuntary. Of the 2,948 chronic patients whose first admission was voluntary, 13.3 percent of subsequent admissions were involuntary. No meaningful correlation was found between the total number of admissions and the percentage of involuntary admissions. We examined the percentage of involuntary admissions by the total number of admissions. In each subgroup composed of patients with up to 15 admissions (patients with five admissions, patients with six admissions, and so forth), involuntary admissions ranged from 16.9 percent to 18.1 percent with no identifiable pattern.
Discussion
The findings of this study indicate that patients with schizophrenia who have an involuntary first hospital admission are no more likely than those with a voluntary first admission to have a subsequent hospitalization. However, among patients in the study who were readmitted, the type of first admission predicted the type of future admissions, although it was by no means the only determinant of future admissions.
The positive association between involuntary first and second admissions remained strong after the analysis controlled for age, gender, education, and religion. The majority of patients whose first hospitalization was involuntary had a voluntary second hospitalization. Additional multivariate analysis showed that for patients whose first admission was involuntary, the percentage of total involuntary admissions over the follow-up period was greater than for those whose first admission was voluntary (41 percent versus 13 percent).
The percentage of involuntary admissions was not related to the total number of admissions. That is, patients with more admissions were not more likely to have a greater proportion of involuntary—or voluntary—admissions than other patients. For patients who were repeatedly hospitalized, the proportion of involuntary admissions did not decrease over time. Among patients in the study with four or more admissions, the percentage of involuntary admissions ranged from 16.9 percent to 18.1 percent, with no observed trend toward reduction of involuntary status over time.
The finding that a first involuntary admission predicted future involuntary hospitalization is in accordance with results of the Danish study described above of 53 first-admission patients with a diagnosis of schizophrenia (3). In that study, involuntary first admission was a strong predictor of future involuntary admissions. However, unlike in our study, the proportion of involuntary admissions decreased with each subsequent admission. For patients suffering from schizophrenia, the finding that involuntary hospitalizations do not tend to decrease over time is alarming.
We expected to find such a decrease because past research has suggested that the course of illness for patients with schizophrenia becomes less volatile over time, due to patients' less prominent positive symptoms (4) and their increased familiarity with the system. For example, Kane and associates (5), in a study of 35 patients hospitalized involuntarily, found that those who experienced symptom remission during their hospitalization and who had a positive attitude toward their current admission were more likely to have voluntary subsequent admissions.
One possible explanation for our finding that involuntary admissions did not decrease over time might be that, to some extent, admitting psychiatrists are more inclined to initiate civil commitment procedures and involuntarily admit patients who were previously admitted involuntarily. Past studies on admission decisions found that being previously hospitalized and being brought to the hospital involuntarily were important factors in admission decisions (1,6). However, none of these studies focused specifically on the decision to admit involuntarily as a function of previous involuntary hospitalization.
In the study reported here, the other variables associated with involuntary admission were similar to those found in previous studies. These cross-sectional studies found that involuntary admission was related to male gender, young age, low social class, and single marital status (7,8,9). Most previous studies, excluding the Danish one, focused on heterogeneous populations from different diagnostic groups and found the diagnosis of schizophrenia to be significantly overrepresented among patients with involuntary admissions. Because our sample included only patients with schizophrenia, diagnosis was not a variable to be considered.
Marital status in our sample was not associated with subsequent involuntary hospitalization. This finding might reflect the complexity of the process of involuntary admission. Patients with schizophrenia who are married might suffer from a less severe form of the illness. On the other hand, living with a spouse and children might lower the threshold for involuntary hospitalization because danger to others might be amplified.
One strength of this study is the use of a cohort of all first admissions from a national population. Its limitations are the use of the diagnosis listed in the registry and the limited number of variables examined. For example, we lacked data on the characteristics of the illness, dangerousness, and suicidality. However, use of a cohort of first-admission patients with multiple admissions and a diagnosis of schizophrenia at the time of last discharge somewhat makes up for having to use the registry diagnosis. Previous studies have found that the diagnosis of schizophrenia recorded in the registry was very consistent between admissions (10) and was in moderate agreement with diagnoses made independently by applying DSM-III criteria to abstracted records (11). Furthermore, Kirkby and colleagues (12), who used the revised version of the Structured Clinical Interview for DSM-III to make definitive diagnoses for a patient group, showed that the diagnoses they arrived at through longitudinal diagnostic profiling of case registry data for the same patients were more accurate than cross-sectional clinical diagnoses in the patients' charts.
Conclusions
To the best of our knowledge, the study reported here is the first to examine the association between legal status at first admission and future admissions among patients with schizophrenia in a national population. The strong association of involuntary legal status at first admission with involuntary status at second admission and with the number of involuntary admissions over time suggests that involuntary first admission might be an important factor in assessing whether patients are likely to be readmitted involuntarily. Future research should examine the relationship between involuntary admission and characteristics of illness, as well as system variables and a fuller array of demographic variables such as socioeconomic status.
Dr. Shmuel Fennig is director of outpatient services at Shalvata Mental Health Center, P.O. Box 94, Hod Hasharon, Israel (e-mail, [email protected]). He is also senior lecturer at the Sackler School of Medicine at Tel Aviv University. Dr. Rabinowitz is professor and chairman-elect of the School of Social Work at Bar Ilan University in Ramat Gan, Israel. Dr. Silvana Fennig is director of the psychiatric child and adolescent unit at the Dr. E. Richard Feinberg department of child and adolescent psychiatry at Schneider Children's Medical Center of Israel in Petah Tikva.
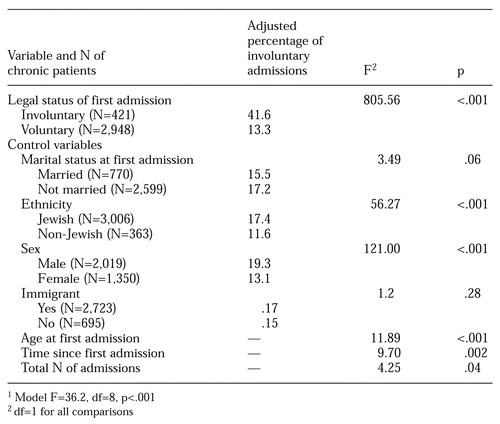 |
Table 1. Simple factorial analysis of variance of the percentage of involuntary admissions among all admissions of 3,420 psychiatric patients who had four or more psychiatric hospitalizations (chronic patients)1
1. Rabinowitz J, Slyuzberg M, Salamon I, et al: Differential use of admission status in a psychiatric emergency room. Bulletin of the American Academy of Psychiatry and the Law 23:595-606, 1995Medline, Google Scholar
2. Slagg NB: Characteristics of emergency room patients that predict hospitalization or disposition to alternative treatments. Hospital and Community Psychiatry 43:397-399, 1992Medline, Google Scholar
3. Munk-Jorgensen P, Mortensen PB, Machon RA: Hospitalization patterns in schizophrenia: a 13-year follow-up. Schizophrenia Research 4:1-9, 1991Crossref, Medline, Google Scholar
4. Biehl H, Maurer K, Schubart C, et al: Prediction of outcome and utilization of medical services in a prospective study of first-onset schizophrenics: results of a prospective 5-year follow-up study. European Archives of Psychiatry and Neurological Sciences 236:139-147, 1986Crossref, Medline, Google Scholar
5. Kane JM, Quitkin F, Rifkin A, et al: Attitudinal changes of involuntarily committed patients following treatment. Archives of General Psychiatry 40:374-377, 1983Crossref, Medline, Google Scholar
6. Rabinowitz J, Massad A, Fennig S: Factors influencing disposition decisions for patients seen in a psychiatric emergency service. Psychiatric Services 46:712-718, 1995Link, Google Scholar
7. Sprengler A: Factors influencing assignment of patients to compulsory admission. Social Psychiatry 21:113-122, 1986Crossref, Medline, Google Scholar
8. Reicher A, Rossler W, Loffler W, et al: Factors influencing compulsory admission of psychiatric patients. Psychological Medicine 21:197-208, 1991Crossref, Medline, Google Scholar
9. Sanguineti VR, Samuel SE, Schwartz SL, et al: Retrospective study of involuntary psychiatric admissions and readmissions. American Journal of Psychiatry 153:392-396, 1996Link, Google Scholar
10. Rabinowitz J, Slyuzberg M, Ritsner M, et al: Changes in diagnosis in a nine-year national longitudinal sample. Comprehensive Psychiatry 35:1-6, 1994Crossref, Google Scholar
11. Goodman AB, Rahav M, Popper M, et al: The reliability of psychiatric diagnosis in Israel's psychiatric case register. Acta Psychiatrica Scandinavica 69:391-397, 1984Crossref, Medline, Google Scholar
12. Kirkby KC, Hay DA, Daniels BA, et al: Comparison between register and structured interview diagnoses of schizophrenia: a case for longitudinal diagnostic profiles. Australian and New Zealand Journal of Psychiatry 32:410-414, 1998Crossref, Medline, Google Scholar



