The Cost of Treating Substance Abuse Patients With and Without Comorbid Psychiatric Disorders
Abstract
OBJECTIVE: Data from a national sample of patients with a primary diagnosis of a substance use disorder were analyzed to examine whether having a comorbid psychiatric diagnosis—a dual diagnosis—was associated with increased costs of health services over a six-year period and whether dually diagnosed patients used particular types of services more frequently. METHODS: A national sample of substance abuse patients being treated in Veterans Affairs (VA) facilities were classified into two groups—those with a dual diagnosis (N=3,069) and those with a single diagnosis of a substance use disorder (N=9,538). The sample was identified from two sources during a two-week period in 1990: outpatients in specialty substance abuse clinics and inpatients discharged with a substance-related diagnosis. Administrative data were used to track VA health care utilization and costs between 1991 and 1996. RESULTS: Dual diagnosis was associated with a significantly increased total cost of care over the six years, which was primarily explained by increased utilization of outpatient psychiatric and substance abuse services. Costs for both groups decreased over time, but they decreased faster among dually diagnosed patients. CONCLUSIONS: Having a comorbid psychiatric diagnosis appears to consistently increase the cost and utilization of services among patients with a primary diagnosis of a substance use disorder. These results are consistent with previous findings for dually diagnosed patients with a primary psychiatric diagnosis. The increased cost may simply reflect the greater severity of illness among dually diagnosed patients, but it may also indicate fragmented and inefficient service delivery.
The clinical and psychosocial problems associated with comorbid psychiatric and substance use disorders have been well documented. Patients with both types of disorders have poorer functioning and poorer clinical outcomes than those with only one disorder (1,2,3), as well as greater difficulty gaining access to health services (4). In addition, many substance abuse treatment programs will not admit patients who have comorbid disorders (5), and patients in psychiatric treatment programs who also have substance use disorders tend to leave treatment earlier than other patients (6,7).
Research on dual diagnosis has typically centered on the additional effect of substance abuse and dependence on the course and cost of psychiatric illness. However, it is also important to understand the additional effect of a psychiatric illness on the course and cost of care for patients who are receiving treatment primarily for substance use disorders. Psychiatric disorders can affect how substance abuse patients respond to both pharmacological treatment (8) and psychosocial treatment (9), exacerbating the course of both substance abuse and psychiatric illness.
As mental health systems find themselves operating under increasing financial strain, data on patients with dual diagnoses are particularly important to study. In response to this strain, many systems have reduced or eliminated services, especially inpatient substance abuse services. However, it is unclear what effect these shifts may have on populations such as patients with dual diagnoses. Some researchers have found that these changes have a negative impact on patients with severe mental illness (10), while others have not (11,12). However, patients who are dually diagnosed are increasingly faced with a decline in service availability from already-fragmented mental health systems.
This study examined the effect of a comorbid psychiatric disorder on health care costs in a national sample of patients being treated for substance use disorders in the Veterans Health Administration of the Department of Veterans Affairs (VA). The VA system offers several advantages for this type of research. First, data are available on a national level, reducing the problems of small sample sizes and variations in programs and geographic regions. Second, VA mental health and substance abuse patients are clinically and demographically similar to patients served by other public mental health systems such as state mental health agencies (13), except that VA primarily serves men and offers services for war-related trauma. Third, VA offers a range of services that closely mirror those offered by state mental health agencies, thus making it more plausible to generalize findings to public systems that offer similar services (14).
Studies that have examined the cost impact of dual diagnosis have found conflicting results. Data from VA and from large state mental health systems indicate that the cost of care is substantially higher for dually diagnosed outpatients than for other psychiatric outpatients (15,16), that studies of inpatient samples find fewer differences between dually diagnosed patients and other patients (15,17), and that the differences in cost of care between dually diagnosed patients and other psychiatric patients appear to decrease over time (15). However, other studies, conducted in private systems of care such as managed care settings and general hospitals, have found that dually diagnosed patients with a primary diagnosis of a substance use disorder have significantly lower rates of use of all types of care, including general medical and psychiatric care, than patients with a single diagnosis of substance abuse disorder (18,19).
One source of the conflicting results may be differences in systems of care. In public systems of care such as VA and state-funded mental health programs, access to high levels of intensive mental health and substance abuse services may be easier to achieve than in private systems, where managed care rewards providers for offering multiple episodes of crisis-oriented care to dually diagnosed patients without addressing the underlying illnesses (16). In studies of costs related to mental illness, it has been estimated that as much as 40 percent of the cost of mental health services in public systems is for services that would not typically be covered by private insurance plans. These services include vocational services, day treatment, and psychosocial treatment (20).
Several hypotheses could be offered to predict that the cost of treating patients with dual diagnoses would be substantial for patients whose primary problem is substance abuse. Such patients typically have higher relapse and readmission rates than other patients (6,7), they are more frequently discharged for noncompliance with treatment (9), and because of their mental illness they are often refused access to services that might prevent future hospitalization (4).
This study used data from a representative national sample of VA patients who were receiving substance abuse treatment. Using administrative data, we followed the sample over a six-year period to examine several questions. What characteristics are associated with being dually diagnosed with a primary substance use disorder and a secondary psychiatric disorder? Is the cost of care higher for dually diagnosed patients than for patients with a substance use disorder alone? Are differences in the cost of treating dually diagnosed patients accounted for by certain types of care (psychiatric, substance abuse, medical, or surgical care) or by care settings (inpatient or outpatient)?
Methods
Study design
The sample consisted of two groups of patients identified during a two-week period at the start of fiscal year 1991 (October 15 to 26, 1990). The two groups were patients being treated for substance abuse in an outpatient VA setting and patients being treated in an inpatient substance abuse program. The total sample (N=12,607) was divided into those who had a single diagnosis of a substance use disorder (N=3,069) and those who were dually diagnosed with a substance use disorder and a psychiatric disorder (N=9,538).
All patients in the sample were followed for six years, and their annual VA utilization and corresponding costs of care were recorded for each of the six years. Analyses were conducted to compare the cost of care between singly and dually diagnosed patients.
Sources of data
Data for these analyses came from four sources. First, a cross-sectional sample of outpatients was identified as part of a national survey of all patients treated in VA mental health clinics during the two-week period in October 1990. Mental health clinicians in all VA mental health programs filled out data sheets on each outpatient clinical encounter that occurred during those weeks. Clinicians recorded diagnoses, demographic characteristics, and functional status.
The cohort used in these analyses was restricted to those in the cross-sectional sample whose recorded Social Security number was valid (as determined by a merge with VA administrative databases), whose clinical diagnosis indicated they were substance abuse patients, and whose primary source of outpatient care was substance abuse specialty clinics. A total of 7,751 outpatients met these criteria.
The second source of data was the patient treatment file (PTF), a discharge abstract file of all completed episodes of inpatient care in VA facilities. From the PTF we identified patients with a diagnosis of a substance use disorder who had occupied a VA substance abuse treatment bed during any portion of the same two-week period as the outpatient survey. A total of 4,845 inpatients were included in these analyses. Patients receiving both inpatient and outpatient treatment (N=1,094) in the two-week period were included in the inpatient group and excluded from the outpatient group.
The third source of data was two longitudinal service use files—the PTF for inpatient care and the outpatient care file for outpatient care—which together record all hospital and outpatient services provided by VA. These administrative databases were used to develop measures of each veteran's use of VA inpatient and outpatient psychiatric, substance abuse, and medical-surgical services from the beginning of fiscal year 1991 (October 1, 1990) through the end of fiscal year 1996 (September 30, 1996).
The final source of data was the cost account from VA's cost distribution report (CDR) (21), which was used to estimate unit costs for VA health care services. The CDR is a comprehensive account that identifies total expenditures associated with all VA inpatient and outpatient health care services. Through the use of accounting procedures standardized across the entire VA, both direct and indirect health care costs are identified and distributed over each major type of health care service. (Indirect costs include construction and maintenance costs, depreciation, and so forth.) When combined with utilization data, the CDR provides a single unit cost for each type of outpatient visit and each type of inpatient care.
Independent variables
All independent variables were calculated from either survey or administrative data at baseline and were held constant throughout the six-year follow-up. The primary independent variable of interest was dual diagnosis (coded 1 for a dual diagnosis and 0 for a single diagnosis). Among outpatients this variable was constructed using the diagnostic checklist filled out by clinicians. Among inpatients ICD-9 discharge diagnoses were used. Patients were categorized as dually diagnosed if they had concomitant diagnoses of a psychiatric and a substance use disorder.
Other independent variables of interest included age, race, gender, and whether the patient received VA disability compensation. All of these factors have been found to be determinants of utilization of VA services both cross-sectionally and over time (22,23).
Other information on psychiatric status included the total number of reported psychiatric diagnoses, as well as dummy-coded dichotomous variables indicating the specific substance use disorder, alcohol or drug. The total number of psychiatric diagnoses was used as one indicator of overall severity of psychiatric illness. Another indicator of severity of illness was whether the patient was an inpatient or outpatient when the sample was identified.
Dependent variables
The outcome variable of primary interest was the annual cost of VA care. Costs were also calculated for seven subtypes of VA care—outpatient psychiatric, substance abuse, and medical and surgical care and inpatient psychiatric, substance abuse, medical, and surgical care. Outpatient utilization was measured as number of visits, and inpatient utilization was measured as the number of bed-days of care. Service use was measured for each fiscal year from 1991 to 1996.
Costs were calculated by multiplying the number of units of service by the average national unit cost for that service as derived from the CDR. All costs were calculated in 1991 dollars to control for inflation. Outpatient medical and surgical costs were collapsed because the CDR allocates the same cost for medical and surgical outpatient procedures, whereas they are assigned different costs when delivered in an inpatient setting.
Analysis
Data analysis proceeded in several steps. First, characteristics of dually diagnosed patients and those with a single diagnosis were compared. Second, total annual health care costs were determined for each group. Repeated-measures analysis of variance was then used to determine whether being dually diagnosed was associated with higher cost over the entire six-year period (a main effect for dual diagnosis), whether cost increased or decreased over time (a main effect for time), and whether the difference in cost between dually diagnosed patients and those without a dual diagnosis changed over time (an interaction between dual diagnosis and time).
For the third step in the analysis, an additional set of analyses was conducted to determine which particular services accounted for differences in cost between dually diagnosed patients and those with a single diagnosis. Repeated-measures analysis of variance was again used to examine the cost of inpatient and outpatient psychiatric, substance abuse, and medical care over the six-year follow-up. Repeated-measures analyses were conducted in SAS using the MIXED procedure. The covariance structure used in these models was assumed to follow a pattern such that time 1 was correlated with time 2, time 2 with time 3, and so forth (24). Due to the large number of models fit to the same data, alpha levels for statistical significance were set at .006.
Results
Table 1 presents cross-sectional differences at the beginning of the study period (October 1990) between the 3,069 patients with a dual diagnosis and the 9,538 patients with a single diagnosis. No gender or age differences were found in the likelihood of being dually diagnosed. However, race was significantly associated with having a dual diagnosis. White and Hispanic patients were more likely to be dually diagnosed, while black patients and those in the category "other" were less likely to be dually diagnosed.
The dually diagnosed patients, all of whom had a primary diagnosis of a substance use disorder, were more likely to have a service-connected disability. This finding is likely attributable to receipt of disability benefits for the comorbid psychiatric disorder, because by statute veterans cannot receive VA compensation for disability associated with substance use disorders. Compared with the patients with a single diagnosis, the dually diagnosed patients were more likely to be abusing drugs other than alcohol.
Psychiatric comorbidity in this sample consisted primarily of serious and persistent mental illness. Among the 3,069 dually diagnosed patients, 24 percent had a diagnosis of schizophrenia or bipolar illness, 24.8 percent had a diagnosis of posttraumatic stress disorder (PTSD), 12.9 percent had major depression, and 41.8 percent had another psychiatric disorder. (Some patients had more than one comorbid diagnosis.)
Figure 1 shows the mean unadjusted annual cost of care for patients with a dual diagnosis and a single diagnosis. Two patterns emerged. First, dually diagnosed patients consistently had higher costs of care than patients with a single diagnosis. Second, although the cost for both groups decreased over time, the costs for dually diagnosed patients decreased slightly more rapidly.
To statistically test these patterns while adjusting for other determinants of service utilization and cost, we fit a series of models to both total cost and cost associated with individual types of mental health and medical services. Table 2 presents the results of these models. The top row of the table presents the total annual cost of care. At each time point, the cost was significantly higher for the dually diagnosed patients. For example, in 1991 the mean cost for dually diagnosed patients was $3,000 more, or 31 percent more, than the cost for the patients with a single diagnosis.
Also, costs for both groups decreased significantly over time. However, between 1991 and 1996, costs decreased more rapidly among dually diagnosed patients than among patients with a single diagnosis—decreases of $6,924 and $5,528, respectively. It should also be noted that overall costs were significantly higher (p<.001) for those who were inpatients when the sample was identified than for those who were outpatients (data not shown).
Table 2 also presents data addressing the question of whether any particular type of care accounted for significantly increased cost among the patients with a dual diagnosis. For the dually diagnosed patients, costs were significantly higher for inpatient, outpatient, and substance abuse care. However, for other types of care, differences between the dually and singly diagnosed groups depended on the year of follow-up. For example, costs for outpatient medical-surgical services were significantly higher among dually diagnosed patients in the first three years of follow-up, but costs for the two groups were not significantly different in subsequent years. In addition, costs associated with inpatient substance abuse care were similar for the two groups in the first three years of follow-up, but they were significantly higher among the dually diagnosed patients in years 4 through 6.
Discussion and conclusions
Overview
In this study we used a national sample of VA substance abuse patients to examine differences in the cost of VA health services between dually diagnosed patients with a primary substance use disorder and patients with a single diagnosis of a substance use disorder. Several conclusions are warranted. First, costs of care for the dually diagnosed patients were persistently and substantially higher. Second, the increased costs were mostly attributable to greater use of psychiatric and substance abuse care. However, dually diagnosed patients also utilized significantly more outpatient medical and surgical care in the first three years of follow-up, and significantly more inpatient substance abuse services in the last three years.
These results are similar to those of previous analyses of the cost of care in the VA system for psychiatric patients with a secondary diagnosis of a substance use disorder (15). That study found that the dually diagnosed patients had significantly higher costs of care than other psychiatric patients, that costs for both groups decreased over time, and that costs decreased faster among the dually diagnosed patients. Taken together, these studies suggest that the coexistence of psychiatric and substance use disorders increases service utilization and cost regardless of which diagnosis is the primary disorder.
Limitations
Before discussing these findings in more detail, several limitations of the data should be addressed. First, diagnostic data used in this study were derived from a simple diagnostic checklist among outpatients and from recorded discharge diagnoses among inpatients. Classification of patients as having a substance use disorder and as having a dual diagnosis was thus vulnerable to errors related to both clinical assessment procedures and compliance with administrative documentation procedures. However, these potential biases are likely to result in conservative estimates of cost differences because misclassification of diagnoses would likely result in underidentification of dual diagnoses. Assuming that dually diagnosed patients are likely to be more severely ill and use more health services than other patients, underidentification would lead to underestimation of cost differentials.
A second limitation of these data is that administrative data from VA do not account for the use of non-VA health services. This limitation particularly restricts our ability to generalize findings about the use of inpatient mental health services, because not all VA hospitals offer such services. It is possible that if use of non-VA services were included in these models, a greater difference in inpatient utilization would have been found between the two groups. However, the majority of VA facilities offer inpatient mental health services, and recent data indicate that use of non-VA facilities by VA patients is low (11 to 13 percent) (25), so the effect of this limitation is probably minimal.
Finally, dually diagnosed patients had significantly lower dropout rates than those with a single diagnosis. Of the dually diagnosed patients treated in 1990, 35 percent did not receive any VA services in 1996, compared with 48 percent of patients with a single diagnosis of a substance use disorder. Patients with a single diagnosis of a substance use disorder may decide not to receive any mental health services or may choose non-VA care, neither of which can be documented with these data. The lower dropout rate among dually diagnosed patients could be one explanation for their increased costs of care. However, when data for those who dropped out of care were removed from the analyses and the models were replicated, the dually diagnosed group still incurred higher total costs than the singly diagnosed group.
Implications for clinical care
Dually diagnosed patients with a primary substance use disorder incurred higher overall health care costs than patients with a single diagnosis of a substance use disorder. The increased cost of care is partly a reflection of the severity of impairment. However, the increased cost could also be a reflection of either inefficiency of care or pressures to provide a certain intensity of services in order to keep treatment beds or slots funded.
One of the difficulties in treating dually diagnosed patients is that the values underlying psychiatric and substance abuse care have historically been in conflict. For example, psychiatric treatment that addresses psychosocial functioning has been viewed by some as enabling substance abuse, while confrontational methods of substance abuse treatment have been viewed as too destabilizing for seriously mentally ill patients. Because of these conflicts, dually diagnosed patients tend to find themselves receiving treatment separately for psychiatric illness and substance abuse, with several potential results. Similar types of services, such as medication management, may be duplicated in both treatment programs, programs may treat one problem as if the other did not exist, and few attempts may be made to integrate services that address underlying issues common to both problems.
One possible solution for such a fragmented and potentially inefficient system would be to develop integrated service delivery programs for dually diagnosed patients. The nature of the most efficient type of program could differ depending on whether patients are high users of inpatient services or more stable outpatients. For example, a treatment model aimed at high inpatient users with a dual diagnosis has been developed by Drake and associates (4). This new treatment model modifies the assertive community treatment team approach and is designed to address problems specific to the risk for relapse to substance abuse, such as housing and entitlement problems, medication compliance, and psychosocial support, without enabling continued substance abuse. The model has been shown to be effective at improving functioning and maintaining abstinence for a significant proportion of patients (5); it also has been shown to have long-term cost-saving impact (26).
The results presented here reflect the traditional approach of keeping outpatient psychiatric treatment separate from substance abuse treatment. However, rather than eliminating needed services, systems interested in reducing the cost of treating dually diagnosed patients in outpatient settings have the opportunity to integrate services by training primary providers to treat both problems. Specialized and integrated services may be more expensive than traditional mental health and substance abuse services and may not necessarily produce better functional outcomes for patients. However, they may be more cost-effective in the longer term by reducing replication of services and the need for expensive crisis-oriented care.
The data presented here draw attention to the potential inefficiency of fragmented mental health and substance abuse care. However, they also leave unanswered many research questions about the best way to provide effective treatment in an era of downsizing and cost cutting.
Future research on dual diagnosis should focus on replicating these results in other populations (for example, in state mental health agencies), investigating whether specialized treatment programs reduce long-term cost and increase efficiency over time, and investigating which treatment approaches are most clinically effective.
The authors are affiliated with the Veterans Affairs Connecticut-Massachusetts Mental Illness Research, Education, and Clinical Care Center in West Haven and Yale University School of Medicine in New Haven, Connecticut. Address correspondence to Dr. Hoff at the Northeast Program Evaluation Center (182), West Haven VA Medical Center, 950 Campbell Avenue, West Haven, Connecticut 06516 (e-mail, [email protected]).
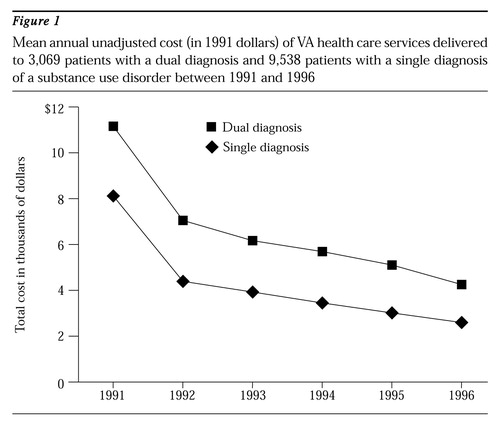
figure 1. Mean annual unadjusted cost (in 1991 dollars) of VA health care services delivered to 3,069 patients with a dual diagnosis and 9,538 patients with a single diagnosis of a substance use disorder between 1991 and 1996
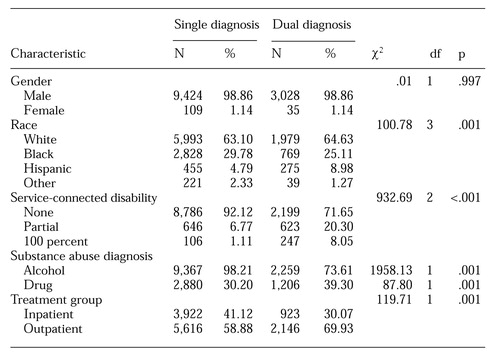 |
Table 1. Characteristics of 9,538 patients with a single diagnosis of a substance use disorder and 3,069 patients with a dual diagnosis in treatment in Veterans Affairs facilities in 1990
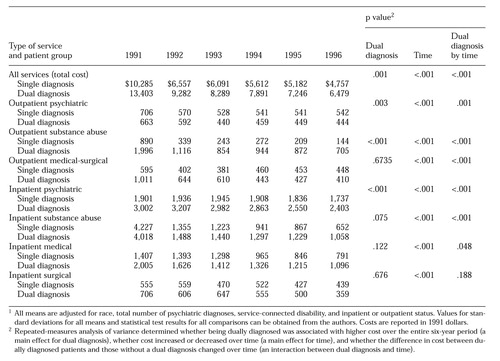 |
Table 2. Adjusted mean annual costs for 3,069 dual diagnosis patients with a single diagnosis of a substance use disorder, by type of service from 1991 to 19961
1. Bartels SJ, Drake RE, Wallach MA: Long-term course of substance use disorders among patients with severe mental illness. Psychiatric Services 46:248-251, 1995Link, Google Scholar
2. Swindle RW, Phibbs CS, Paradise MJ, et al: Inpatient treatment for substance abuse patients with psychiatric disorders: a national study of determinants of readmission. Journal of Substance Abuse 7:79-97, 1995Medline, Google Scholar
3. Rousaville BJ, Dolinsky ZS, Babor TF, et al: Psychopathology as a predictor of treatment outcome in alcoholics. Archives of General Psychiatry 44:505-513, 1987Crossref, Medline, Google Scholar
4. Drake RE, Yovetich NA, Bebout RR, et al: Integrated treatment for dually diagnosed homeless adults. Journal of Nervous and Mental Disease 185:298-305, 1997Crossref, Medline, Google Scholar
5. Drake RE, McHugo GJ, Noordsy DL: Treatment of alcoholism among schizophrenic outpatients:4-year outcomes. American Journal of Psychiatry 150:328-329, 1993Google Scholar
6. Leon SC, Lyons JS, Christopher NJ, et al: Psychiatric hospital outcomes of dual diagnosis patients under managed care. American Journal on Addictions 7:81-86, 1998Crossref, Medline, Google Scholar
7. Greenfield SF, Weiss RD, Tohen M: Substance abuse and the chronically mentally ill: a description of dual diagnosis treatment services in a psychiatric hospital. Community Mental Health Journal 31:265-277, 1995Crossref, Medline, Google Scholar
8. Ziedonis DM, Kosten TR: Depression as a prognostic factor for pharmacologic treatment of cocaine dependence. Psychopharmacology Bulletin 27:337-343, 1991Medline, Google Scholar
9. McLellan AT, Luborsky L, Woody GE, et al: Predicting response to alcohol and drug abuse treatments: role of psychiatric severity. Archives of General Psychiatry 40:620-625, 1983Crossref, Medline, Google Scholar
10. Popkin MK, Lurie M, Manning W, et al: Changes in process of care for Medicaid patients with schizophrenia in Utah's prepaid mental health plan. Psychiatric Services 49:518-523, 1998Link, Google Scholar
11. Dickey B, Norton E, Normand SL, et al: Managed mental health experience in Massachusetts. New Directions for Mental Health Services, no 78:115-122, 1998Google Scholar
12. Hausman JW, Wallace N, Bloom JR: Managed mental health experience in Colorado. New Directions for Mental Health Services, no 78:107-114, 1998Google Scholar
13. Mental Health, United States, 1990. Rockville, Md, National Institute of Mental Health, 1991Google Scholar
14. Hoff RA, Rosenheck RA, Sernyak M, et al: A comparison of VA to public sector mental health patients: the Connecticut outcomes study (abstract). Proceedings of the 1999 Annual Meeting of Veterans Affairs Health Services Research and Development. Washington, DC, Department of Veterans Affairs, 1999Google Scholar
15. Hoff RA, Rosenheck RA: Long-term patterns of service use and cost among patients with both psychiatric and substance abuse disorders. Medical Care 36:835-843, 1998Crossref, Medline, Google Scholar
16. Dickey B, Azeni H: Persons with dual diagnosis of substance abuse and major mental illness: their excess costs of psychiatric care. American Journal of Public Health 86:973-977, 1996Crossref, Medline, Google Scholar
17. Bradley CJ, Zarkin GA: Inpatient stays for patients diagnosed with severe psychiatric disorders and substance abuse. Health Services Research 31:387-408, 1996Medline, Google Scholar
18. Lyons JS, McGovern MP: Use of mental health services by dually diagnosed patients. Hospital and Community Psychiatry 40:1067-1069, 1989Abstract, Google Scholar
19. Pirzada SR, Ries R, LoGerfo JP: Cost of comorbid alcohol and drug problems. American Journal on Addictions 6:193-204, 1997Crossref, Medline, Google Scholar
20. Hollingsworth EJ, Sweeney JK: Mental health expenditures for services for people with severe mental illnesses. Psychiatric Services 48:485-490, 1997Link, Google Scholar
21. Cost Distribution Report, 1990. Washington, DC, Department of Veterans Affairs, 1990Google Scholar
22. Hoff RA, Rosenheck RA: Female veterans' use of VA health care services. Medical Care 36:1114-1119, 1998Crossref, Medline, Google Scholar
23. Hoff RA, Rosenheck RA: The use of VA and non-VA mental health services by female veterans. Medical Care 36:1524-1533, 1998Crossref, Medline, Google Scholar
24. Agresti A, Finlay B: Statistical Methods for the Social Sciences. San Francisco, Dellen, 1986Google Scholar
25. Rosenheck RA, Rothbard A, Azarian K, et al: Cross-system use of VA and non-VA services in Philadelphia (abstract). Proceedings of the 1998 Annual Meeting of Veterans Affairs Health Services Research and Development. Washington, DC, Department of Veterans Affairs, 1998Google Scholar
26. Clark RE, Teague GB, Ricketts SK, et al: Cost-effectiveness of assertive community treatment versus standard case management for persons with co-occurring severe mental illness and substance use disorders. Health Services Research 33:1283-1306, 1998Google Scholar



