Differential Access to Care for Children With ADHD in Special Education Programs
Abstract
Access to treatment for children with attention-deficit hyperactivity disorder (ADHD) was examined in the general health, specialty mental health, and informal care sectors. Special education students in a Florida school district were screened for ADHD, and high-risk children and their parents completed diagnostic and services assessment interviews. Female gender, minority status, and rural residence lowered the probability of ADHD service use in the general health sector. Use of services in the mental health and informal sectors was predicted by a child's need for services. Further study is needed to identify barriers to service use at the parental or gatekeeper level for this common disorder among children.
Effective treatment for children with attention-deficit hyperactivity disorder (ADHD), one of the most common psychiatric disorders among children (1), often combines psychopharmacologic, behavioral, and educational interventions. The majority of ADHD treatment for children is delivered in the general health care sector, and a smaller proportion is provided by mental health specialists and schools. Services provided in the informal care sector, such as family support groups and advocacy, have also played an increasingly important role.
Controversy surrounds the appropriate identification of affected children, with concerns about overidentification countered by indications that a sizable proportion of affected children may remain untreated (1,2). However, few studies investigating access to care have focused on children with ADHD.
This study examined treatment for ADHD in different health care sectors among students in special education programs, a population with a disproportionately high number of children with ADHD. Using Andersen's model of access to care (3), this study determined lifetime and past-year use of mental health services in general health, specialty mental health, and informal care sectors of the health services delivery system. In addition, we investigated how predisposing characteristics (the child's gender and ethnicity), enabling characteristics (place of residence, socioeconomic status, and type of health insurance type), and need characteristics (symptoms, impairment, and family burden) were related to a child's likelihood of receiving treatment for ADHD. We hypothesized that after we controlled for other predictors, children with greater needs would be more likely to receive care from mental health specialists and more likely to use services in the informal care sector than children with less severe or complicated ADHD.
Methods
In 1995, using a two-stage design, we first screened for ADHD an entire Florida school district population of second-through-fourth-grade special education students with learning disabilities or emotional handicaps. Children who scored in the clinical range on two questionnaires (a T score above 64 on the Abbreviated Symptom Questionnaire [4] and a ranking below the 11th percentile on the Attention Deficit Disorder Evaluation Scale [5]) or who had ever received treatment for ADHD were identified as being at high risk. A follow-up individual interview with the parent was conducted for high-risk children. Methods and instruments are described in detail elsewhere (2)
Of 722 eligible students, 499 (69 percent) were successfully screened, and 41 percent (N=207) of the screened participants met criteria for high risk of ADHD. Sixty-nine percent (N=143) of the parents of high-risk children completed personal interviews and were included in this analysis. Eighty-eight percent (N= 126) of the children of these parents met diagnostic criteria for ADHD.
Socioeconomic status was divided into five levels using the Hollingshead four-factor index. Diagnoses for ADHD and comorbid oppositional disorder and conduct disorder were made using the Diagnostic Interview Schedule for Children, version 3.0. Child impairment was measured using the Columbia Impairment Scale, and family burden was assessed using the Child and Adolescent Burden Assessment. Reliability and validity of these instruments have been found acceptable (6,7,8).
Use of mental health services was evaluated with the Service Use for Children and Adolescents Parent Interview (SCA-PI), which was developed by the National Institute of Mental Health. The SCA-PI was modified to include inquiry into lifetime and past-year service use.
Mental health services delivered by a pediatrician, family practitioner, or general nurse practitioner were defined as those received in the general care sector. Specialty mental health services were defined as services delivered by a psychiatrist, psychologist, psychiatric nurse, or social worker. Use of parent support and education groups or the child's participation in a summer camp program for children with ADHD were classified as services in the informal care sector.
Bivariate analysis was conducted using a chi square test of proportions for discrete variables and analysis of variance procedures for continuous variables. Multiple logistic regression analyses were used to determine the independent contribution of predictors of use of services in the respective sectors. Two alternative procedures were used to select predictors: a full model containing all variables identified as potential predictors and a stepwise regression procedure that retained predictors with logistic regression p values of less than .10. The odds ratios and statistical significance associated with predictor variables from these two procedures were very similar; hence, results for the full model are presented. The statistical analyses were performed using SAS.
Results
More than half of the 143 children with ADHD had received mental health services in the general health care sector—91 children (64 percent) in their lifetime and 75 children (52 percent) in the past year, as Table 1 shows. In the specialty mental health care sector, 81 children (57 percent) had received treatment in their lifetime and 51 children (36 percent) in the past year.
Sixteen of the 143 families (11 percent) had either lifetime or past-year use of services in the informal care sector. Higher rates of mental health service use in the general health sector were observed for boys, white children, and urban residents. Both lifetime and past-year use of the specialty mental health sector was associated with need variables, and lifetime use was associated with ethnicity and with residence. Higher use of informal services was related to the absence of oppositional disorder or conduct disorder and to the child's higher impairment. Further details about service use by sector and its independent predictors are described in Table 1.
Discussion and conclusions
As hypothesized, past-year use of the specialty mental health care sector and use of informal care was predicted by a child's need. However, lifetime use of mental health specialists also differed by ethnicity, a finding that merits further study to explore variation in detection of need and referral patterns by primary care providers for minority children. Previous reports suggest that girls and minorities with ADHD are more likely to remain untreated, and in this sample, both of these groups had greater rates of unmet need for ADHD treatment (2).
Service use in the general health care sector, the most common provider of mental health services for this study population, varied by gender, ethnicity, and residence. Even after the analysis controlled for other access predictors, girls and minority children were less likely to receive mental health services from a primary care provider. This finding raises special concerns because generalists increasingly function as gatekeepers for specialty mental health services, yet they may not detect service needs of girls and minority children with ADHD. Further, rural residence was associated with less use of primary care providers and mental health specialists, findings that may indicate that rural families represented in this study have difficulty getting ADHD treatment for their children.
The main limitations of this study are the relatively high nonparticipation rate in the initial screening and use of a special education sample, rendering the results preliminary and not representative of children in the general population. Rates of use of specialty mental health services were higher than those in community samples (9), which may reflect parents' greater awareness of their children's problems due to the special education qualification process. Furthermore, parental reports of treatment were not compared with information from providers or in medical records. However, previous studies indicate that parents can provide valid treatment histories if reasonable time frames are selected (10). Finally, the study could not address how parents' help-seeking and providers' failure to detect ADHD or refer children to specialty care specifically contributed to the differential access to care. To ensure equitable access to care, further studies are needed to improve our understanding of the mechanisms that underlie children's access to ADHD treatment.
Acknowledgments
This research was supported by grants K12-MH00990 and R24-MH51846 from the National Institute of Mental Health. The authors thank Paul Bycott, Ph.D., for assistance with the statistical analysis; Kenneth B. Wells, M.D., M.P.H., for his mentorship; Amy Perwien, B.A., Elena Schuhmann, B.A., and Kathy McNaughton, B.A., for research assistance; and Peter Jensen, M.D., for permission to use the SCA-PI.
Dr. Bussing is associate professor in the departments of psychiatry and health policy and epidemiology at the University of Florida, Box 100177 UFHC, Gainesville, Florida 32610-0177 (e-mail, [email protected]). Dr. Zima and Dr. Belin are assistant professors in the department of psychiatry and biobehavioral sciences at the University of California, Los Angeles (UCLA). Dr. Belin is also assistant professor in the department of biostatistics at UCLA.
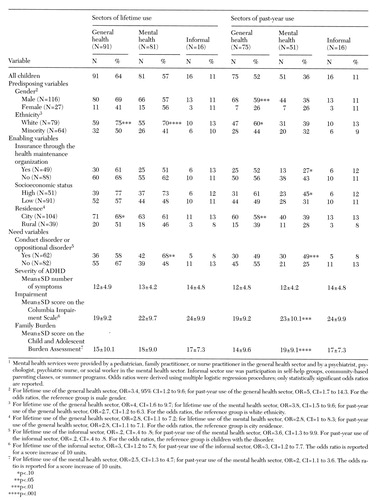 |
Table 1. Predictors of lifetime and past-year use of mental health services in different sectors in a school district population of special education students at high risk for ADHD1
1. Szatmari P, Offord DR, Boyle MH: Correlates, associated impairments, and patterns of service utilization of children with attention deficit disorder: findings from the Ontario Child Health Study. Journal of Child Psychology and Psychiatry 30:205-217, 1989Crossref, Medline, Google Scholar
2. Bussing R, Zima BT, Perwien AR, et al: Children in special education programs: attention deficit hyperactivity disorder, use of services, and unmet need. American Journal of Public Health 88:880-886, 1998Crossref, Medline, Google Scholar
3. Andersen RM: Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36:1-10, 1995Google Scholar
4. Conners KC: Conners' Abbreviated Symptom Questionnaire Manual. North Tonawanda, NY, Multi-Health Systems, 1990Google Scholar
5. McCarney SB: Attention Deficit Disorder Evaluation Scale—Home Version. Columbia, Mo, Hawthorne Educational Services, 1989Google Scholar
6. Jensen P, Roper M, Fisher P, et al: Test-retest reliability of the Diagnostic Interview Schedule for Children (DISC 2.1): parent, child, and combined algorithms. Archives of General Psychiatry 52:61-71, 1995Crossref, Medline, Google Scholar
7. Messer SC, Angold A, Costello EJ, et al: The Child and Adolescent Burden Assessment (CABA): measuring the family impact of emotional and behavioral problems. International Journal of Methods in Psychiatric Research 6:261-284, 1996Crossref, Google Scholar
8. Bird HR, Shaffer D, Fisher P, et al: The Columbia Impairment Scale (CIS): pilot findings on a measure of global impairment for children and adolescents. International Journal of Methods in Psychiatric Research 3:167-176, 1993Google Scholar
9. Burns BJ, Costello EJ, Angold A, et al: Children's mental health services use across service sectors. Health Affairs 14(3):147-159,1995Google Scholar
10. Burns BJ, Angold A, Costello EJ: Measuring child, adolescent, and family services use, in Evaluating Mental Health Services for Children. Edited by Bickman LB, Rog DJ. San Francisco, Jossey-Bass, 1992Google Scholar



