Homelessness and Mental Illness in a Professional- and Peer-Led Cocaine Treatment Clinic
Abstract
The combined problems of substance abuse, mental illness, and homelessness among the urban poor represent a major public health issue. The study evaluated 340 patients attending a cocaine day treatment program that integrates peer leadership and professional supervision. Thirty-six percent of the sample had a major mental illness, and 39 percent were homeless. Sixty-nine percent achieved an acceptable final urine toxicology status, and the median number of program visits was 46. Homelessness, a longer history of cocaine use, and a diagnosis of schizophrenia were associated with positive treatment outcomes. The results support the feasibility of a cocaine abuse treatment model combining professional and peer leadership.
In recent years, the problem of combined substance dependence and mental illness among the urban poor has been greatly aggravated by the widespread use of crack cocaine (1,2). Peer-led approaches have been commonly used with substance abusers without other diagnoses in 12-step programs and drug-free therapeutic communities.
To apply this approach with patients who have multiple risk factors, we developed an innovative cocaine day treatment program in which patients colead treatment with professional staff. Other well-established modalities, including community reinforcement (3), relapse prevention (4), psychiatric diagnostic assessment, and pharmacotherapy, are also incorporated. This demonstration program was given the Gold Award by the American Psychiatric Association in 1993, "in recognition of its effective use of the limited resources of a public hospital for substance abuse treatment”(5). The objective of the study reported here was to evaluate whether homelessness, chronicity of substance use problems, and mental illness are associated with treatment outcomes for patients in our treatment program.
Methods
The program, Recovery Cocaine Clinic, is a component of the Bellevue Hospital Center and is staffed by a part-time psychiatrist, a social worker, two counselors, and a nurse. The clinic operates five days a week and is organized along the lines of a modified drug-free therapeutic community (6) and adapted from a day program implemented by De Leon and associates (7) for methadone-maintained patients. Acute relapses in mental functioning are managed by referrals for brief inpatient treatment followed by return to the ambulatory program. The median length of stay in the program is four months.
Assessments were conducted by the psychiatrist using DSM-III-R criteria, and additional information on demographic characteristics, length of drug use, previous substance abuse treatment, arrests, and homelessness was obtained by social work staff using a modification of the Addiction Severity Index (8). Urinalyses for drugs of abuse were randomly obtained two or three times weekly. When patients were discharged from the program or dropped out, results of the last three sequential urine toxicology tests were tabulated for each patient who attended at least seven days (one five-day week plus two additional days) and who therefore provided at least three urine specimens. Patients with negative results on all three tests were considered to have an acceptable outcome. Data for these patients were compared with data for patients who had at least one positive urinalysis among the final three, which was considered an unacceptable outcome. Clinic attendance was measured as the total number of visits.
Results
Of 387 patients consecutively admitted to the clinic between 1990 and 1995, a total of 88 percent (N=340) had at least three urine toxicology tests. Compared with patients who did not complete three tests, they were more likely to be male (60 percent versus 40 percent; c2=6.27, df=1, p<.05) and undomiciled (39 percent versus 23 percent; c2=12.56, df=2, p<.01) and to have received previous treatment for substance abuse (72 percent versus 45 percent; c2=14.8, df=1, p<.001). The two groups did not differ on any other variable assessed. Data are provided on the cohort of 340 unless otherwise indicated.
A total of 203 patients (60 percent) were male; 230 (68 percent) were black, 68 (20 percent) were Hispanic, and 42 (12 percent) were white. Eighty of the patients (24 percent) had not completed high school, 84 (25 percent) had completed high school, and 75 (22 percent) had attended college. Of the 328 patients for whom data on arrests were available, 228 (70 percent) had an arrest history. Thirty-four of the 326 patients for whom data were available (10 percent) were mandated into treatment by the criminal justice system.
A total of 246 of 327 patients with available data (75 percent) had previously received substance abuse treatment. Diagnostic information was available for 315 patients, of whom 186 (59 percent) had non-substance-related diagnoses. They included 52 patients (17 percent) with schizophrenia or other psychosis, 59 (19 percent) with major affective disorders, and 75 (24 percent) with a personality disorder. A total of 112 of the 331 patients for whom data were available (34 percent) were taking psychiatric medications at intake.
Excluding 75 patients admitted directly from institutional settings, 133 of the remaining 265 patients (50 percent) were currently homeless. As Table 1 shows, homeless patients were more often male and black, were either never or previously married, and had used crack cocaine for more than a year. None of the other variables assessed were significantly associated with homelessness.
Of the 340 patients in the sample, 237 (69 percent) had an acceptable outcome, three negative toxicology tests at discharge. The median number of clinic visits for the sample was 46 (mean±SD=92.8±105). Patients with an axis I disorder (N=111) did not differ from other patients (N= 204) in either an acceptable outcome or attendance.
Bivariate analyses assessing relationships between treatment outcome and all sociodemographic, drug, and psychiatric status variables indicated that patients with an acceptable outcome were more likely to be homeless or to have been institutionalized (for example, in hospitals or in prisons) before entering the program (c2=9.13, df=2, p<.01), to have used crack cocaine for more years (t=3.76, df=263, p<.001), and to have made more visits to the clinic (t=4.78, df=259, p<.001). In a logistic regression analysis in which two variables—years of crack cocaine use and domiciled status—were entered as predictors of treatment outcome, both variables retained significance (p<.01; for years of cocaine use, adjusted odds ratio=1.065, 95 percent confidence interval=1.03 to 1.11; for domiciled status, OR=.480, CI=.30 to .78). The number of clinic visits was not entered into the analysis due to its inherent redundancy with toxicology test results.
Positive correlates of attendance (number of clinic visits) included college education (t=2.15, df=337, p<.05), current prescribed psychiatric medication (t=3.35, df=169, p<.001), and a diagnosis of schizophrenia (F=8.76, df=2,312, p<.001; Newman Keuls tests, p<.05). In a multiple linear regression analysis testing the effects of current psychiatric medication, a diagnosis of schizophrenia, and college education, all three variables retained significance (beta=.159, .158, and .133, respectively; F=9.28, df=3,301, p<.001, R2=.085).
Discussion and conclusions
This study evaluated a professional- and peer-led ambulatory treatment approach to engage cocaine abusers with multiple psychiatric and social problems. Our assessment of a sample of patients who remained in treatment for at least two weeks showed the majority to be from minority ethnic groups and to have a history of arrests. In addition, a majority who entered the program from ambulatory status—that is, not from institutions—were homeless on admission.
Despite characteristics suggestive of a high risk of failure, the patients made a substantial number of visits to the program, and most had an acceptable outcome at discharge, defined as three sequential negative toxicology tests. In fact, homelessness and a longer history of cocaine use were predictive of a more positive outcome as measured by urine toxicology tests. Perhaps this finding reflects patients’ “bottoming out”(9,10), that is, reaching an unacceptable level of compromised circumstances before moving toward improvement.
Furthermore, a diagnosis of schizophrenia and an arrest history might be thought to have an adverse impact on patients' adjustment to treatment. However, these variables were not associated with poorer outcome on urine toxicology tests or in attendance. Attendance was instead positively associated with variables that may reflect institutional affiliation, namely, a diagnosis of schizophrenia, current psychiatric medication, and college experience.
It was not possible to comprehensively assess treatment outcomes within the framework of this study. For example, a patient's total number of visits was used as a measure of retention, although some patients attended irregularly and missed more intervening visits than others. An algorithm fully accounting for visit density and length of stay in treatment reflecting continuity would be difficult to define. In addition, many patients tested positive for substances early in their treatment; however, to obtain a uniform measure of their status at termination, we chose to evaluate the outcome of the last three urinalyses.
While our findings suggest the viability of the combined professional- and peer-led approach described here, changes in patients' general psychiatric symptoms, as assessed by objective measures, and their course after treatment have yet to be determined. A follow-up study along these lines to fully evaluate this treatment approach is under way.
Nonetheless, this study and others on related approaches suggest that peer-leadership techniques combined with professional supervision can be applied to a variety of multiply disadvantaged populations. Furthermore, our findings suggest that psychiatric and social disability may not hinder the application of this treatment in the ambulatory setting. In fact, patients who are homeless, have more severe drug use, and require psychiatric medications may do better than less disabled ones in settings with medical and social services targeted to their needs. Further research into peer-led modalities with limited professional staffing may be warranted, even for patients perceived to be highly disadvantaged.
Acknowledgments
This project was supported by grants TI00424 from the Center for Substance Abuse Treatment and H86-SP03626 from the Center for Substance Abuse Prevention.
The authors are affiliated with the division of alcoholism and drug abuse of the department of psychiatry at New York University Medical Center and with the Nathan Kline Institute. Send correspondence to Dr. Galanter at the Division of Alcoholism and Drug Abuse, NYU Medical Center, 550 First Avenue, New York, New York 10016 (e-mail, marcgalanter @nyu.edu).
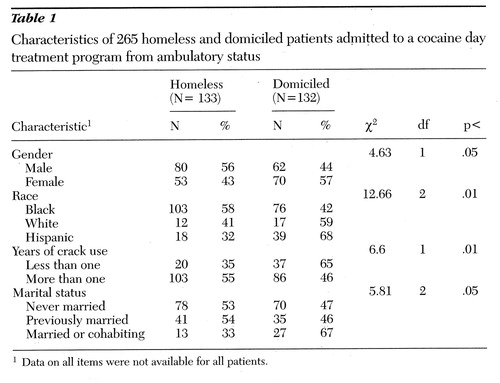 |
Table 1. Characteristics of 265 homeless and domiciled patients admitted to a cocaine day treatment program from ambulatory status
1Data on all items were not available for all patients.
1. Bunt G, Galanter M, Lifshutz H, et al: Cocaine/ “crack” dependence among psychiatric inpatients. American Journal of Psychiatry 147:1542-1546, 1990Link, Google Scholar
2. Rahav M, Rivera JJ, Nuttbrock L, et al: Characteristics and treatment of homeless, mentally ill, chemical-abusing men. Journal of Psychoactive Drugs 27:93-103, 1995Crossref, Medline, Google Scholar
3. Hunt GN, Azrin NH: A community reinforcement approach to alcoholism. Behavior Research and Therapy 11:91-104, 1973Crossref, Medline, Google Scholar
4. Marlatt GA, Gordon J: Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York, Guilford, 1985Google Scholar
5. Gold Award: Comprehensive clinical services for substance abuse treatment in an inner-city general hospital. Hospital and Community Psychiatry 44:991-994, 1993Medline, Google Scholar
6. De Leon G, Ziegenfuss JT Jr (eds): Therapeutic Communities for Addictions: Readings in Theory, Research, and Practice. Springfield, Ill, Thomas, 1986Google Scholar
7. De Leon G, Staines G, Perlis PE, et al: Therapeutic community methods in methadone maintenance (Passages): an open clinical trial. Journal of Drug and Alcohol Dependence 37:45-57, 1995Crossref, Medline, Google Scholar
8. Galanter M, Egelko S, De Leon G, et al: Crack/cocaine abusers in the general hospital: assessment and initiation of care. American Journal of Psychiatry 149:810-815, 1992Link, Google Scholar
9. Cunningham JA, Sobell LC, Sobell MB, et al: Alcohol and drug abusers' reasons for seeking treatment. Addictive Behaviors 19:691-696, 1994Crossref, Medline, Google Scholar
10. Cunningham JA, Sobell LC, Sobell MB, et al: Resolution from alcohol treatment problems with and without treatment: reasons for change. Journal of Substance Abuse 7:365-372, 1995Crossref, Medline, Google Scholar



