Intensity and Duration of Intensive Case Management Services
Abstract
OBJECTIVE: Two policy issues related to intensive case management programs were examined: limiting caseload size to ensure that services are intensive and providing intensive services to the same clients in perpetuity. METHOD: The Denver Acuity Scale, which indicates need for services on a 5-point scale, was used for determining the service intensity needed by consumers and for increasing case managers' efficiency when caseload size varied. The acuity ratings of individuals in the Denver intensive case management program were examined to evaluate the effects of service duration on decompensation. Each consumer was rated at every service contact. The percentage of individuals readmitted to the program after they graduated was calculated, and the trajectories of 87 individuals who continued to be served by the program after they attained the highest rating of functioning were examined. RESULTS: Of the 112 individuals who graduated from the program in the 29-month study period, four (4 percent) were readmitted. More than half of the 87 consumers who achieved the highest functioning level did not deviate from that level for the remainder of the study period. Nearly a fifth showed some deterioration shortly after achieving that level but then improved. Slightly more than a fourth continued to deteriorate, but many never reached the lowest levels of functioning. CONCLUSIONS: To increase efficiency and ensure appropriate service levels, service intensity should be based on individual consumers' functioning levels. Most consumers are unlikely to need intensive case management in perpetuity. Providing more intensive services than needed or providing services longer than needed is inefficient and may even impede consumer recovery.
Two fundamental tenets underlie many intensive case management programs. The first is that caseload size is a useful index of service intensity. The second is that intensive case management services need to be provided to a consumer in perpetuity because termination of services results in a high rate of decompensation. This study examined these assumptions and their implications for program operation and consumer recovery.
Considering the appropriate intensity and duration of case management is becoming increasingly important. Initially, intensive case management programs were praised as less costly than hospitalization. But managed care and pressures to increase efficiency are causing some to question the need for consumers' lifetime participation, especially in programs with fixed small caseloads (1,2,3). This issue is part of the debate about what constitutes medically necessary services and the need to match level of care to level of need (4,5). Cost containment pressures seem likely to result in policies aimed at increasing efficiency by controlling the intensity and duration of case management services (6).
Small caseload size is often considered to be a determinant of the fidelity of intensive case management to the original program model (1,7,8,9), but it is important to distinguish between the capacity to provide intensive services and the actual intensity of services provided. The literature contains numerous examples in which no clear empirical relationship was found between caseload size and actual service intensity (9,10,11).
Fixing caseload sizes at low numbers (for example, fewer than 20 persons) is based on the notion that it is impossible for a case manager to provide intensive services for more than about 20 persons. This assumption is generally true, but only for relatively brief periods of time. It is likely to be true when consumers begin to receive services, but it continues to be tenable only if one assumes that consumers do not improve and will continuously require the same level of service intensity. However, it has become clear that people with serious mental illnesses can and do recover (12,13) and that improvement is possible if not common in many case management programs, especially if reduced hospitalization is seen as a marker of improvement (14,15,16).
The potential for recovery suggests that fixing caseloads at low levels and providing case management in perpetuity is often unnecessary. Indeed, one must question whether such policies meant to ensure continuity of care may actually impede recovery by promoting dependency. No consensus exists about whether "in perpetuity" or "lifelong" is the same as "time unlimited." Time unlimited can be construed as lifelong. It may also mean that the duration of program involvement is individualized.
An analogy is the concept of mastery learning. Time to achieve mastery varies, but the desired level of mastery is constant. Thus graduation from a case management program is determined by meeting criteria for when services are no longer needed rather than by time limits. A lifetime approach combined with fixed, small caseloads will result in increased costs and may even impede consumer recovery.
An early attempt to systematically match levels of care to levels of need occurred in an intensive case management program that operated in Denver in the late 1980s. The program, which has been described elsewhere (17,18,19,20), was aimed at consumers designated as most in need. It was staffed by approximately 20 case managers, most of whom held bachelor's degrees. Case managers were split into two teams each reporting to a master's-level supervisor, but the model emphasized individual, rather than team, responsibility. An on-staff psychiatrist provided consultation. Consumers were never seen in the program's office. The program provided coverage 24 hours a day, seven days a week. It incorporated both assertive case management and service brokerage to a community mental health center for ongoing mental health care.
This program was the first in the country to hire persons with serious mental illness as case management aides (19). The program was also notable for its use of the Denver Acuity Scale (see Table 1) as a method for determining the intensity of case management needed. The rows in Table 1 reflect the program's goals for participants and were key determinants of service intensity. The columns represent a 5-point scaling of each goal. By reading down a column, one can obtain a description of the key characteristics of persons receiving a particular acuity rating, assuming that ratings across the dimensions fall within a column.
Minimum intensity levels of service for consumers at each acuity level (see Table 2) were established using an expert panel's judgments of vignettes that had been developed to reflect the column descriptions in Table 1. Experts judged how frequently each consumer needed to be seen face-to-face to ensure a reasonable level of comfort with regard to the consumer's and others' safety and well-being.
Program staff were trained to arrive at a global acuity rating by circling the appropriate acuity level for each row (Table 1) and then picking the column with the greatest frequency of circled cells. If two columns had the same frequency of circled values, staff used the higher of the two as the global rating. Other programs adapting this technique went to elaborate lengths to define weights and formulas to derive global acuity values. Our experience in Denver with the acuity ratings showed little dispersion across the columns, supporting the decision to base the global value on a simple visual inspection of the ratings.
A computerized management information system supported program decision making (17), using acuity ratings recorded for every service event. Monthly caseload reports flagged persons who were not seen frequently enough. Our concern was controlling for underutilization, as the Denver program was perceived as a high-risk operation. Obviously, the same system would support identification of persons being overserved.
The intensity levels developed for this program highlight the futility of setting fixed caseloads to ensure service intensity. We developed three hypothetical caseloads, constraining the time required to serve each to 95 hours a month. This constraint was based on program data indicating that case managers spent about 60 percent of their time in face-to-face contacts plus travel to the place of contact, with the remaining 40 percent spent in activities such as team meetings, training, telephone and paperwork, off-hours coverage, sick leave, and vacation. The constraint was also based on the average contact plus travel time of 50 minutes.
From a staffing perspective, the three hypothetical caseloads were identical; each one required the same amount of time to provide the expected level of service. However, the sizes of the caseloads varied from nine to 22 to 40. The three caseloads can be thought of as the same case manager's caseload at three points in time corresponding to start-up, three months later, and nine months later. A caseload of 20 persons exceeds the capacity of a case manager to deliver intensive services if all cases are newly assigned and the case manager is expected to pick them up simultaneously. In contrast, nine months later when the majority of consumers are at acuity levels of 1 and 2, 40 recipients are needed to meet productivity and intensity standards.
If caseload sizes are fixed at 20 and the productivity standard is enforced (60 percent of time in face-to-face services), consumers must be overserved to meet the standard. If the productivity standard is not enforced, considerable resources are wasted because only a small percentage of time is required to provide the level of service needed and there is no incentive to spend the remaining time in productive activities. In short, the acuity of the case mix and the number of cases jointly determine the time required to serve the caseload.
If resources are wasted when caseloads are fixed and services are considered lifelong, then determining an appropriate criterion for program graduation becomes important. The Denver program used the acuity scale to define when someone was ready for graduation. The rather conservative criterion was six consecutive months at an acuity level of 1 (see Table 1). In this study we examined 29 months of program data to determine the percentage of graduates who later decompensated and the subsequent trajectories of people who achieved an acuity rating of 1. The trajectory issue provides an empirical basis for program planners seeking to establish graduation criteria.
Methods
We identified the number of people who graduated between November 1986 and April 1989 and then counted those who were readmitted to the program; consumers were readmitted only if they decompensated. This assessment of postgraduation decompensation is limited because consumers who decompensated may not have returned to the program; for example, they may have moved.
Another way to assess postgraduation decompensation is to examine change in acuity ratings for individuals who continued to be served after attaining an acuity rating of 1. We call the point at which this occurred the index event, defined as the receipt of two ratings of 1 for two successive service events on different dates (consumers in the program were rated at every service event). We rejected more lenient definitions (for example, a single acuity rating of 1) because they resulted in false positive indicators of a high level of functioning due to keying errors and initial impressions that quickly changed. Some consumers were in the program a long time before the index event occurred; others had faster improvement. The mean±SD time spent in the program for those who graduated was 14.6± 4.7 months. Factors related to length of program participation have been discussed elsewhere (18).
We examined data for 87 consumers for whom ratings were recorded after the index event. People who had fewer than two ratings recorded after the index event were excluded. Having fewer than two ratings could occur because the data set included events up to a cutoff date, truncating some persons' data. Also, some consumers moved out of the area, others suddenly refused services, and some could not be located. Still others may have been imprisoned or placed in a long-term-care facility; some may have died. More information about discharge has been reported elsewhere (20).
To assess the magnitude and direction of change for each consumer, we averaged the acuity ratings in each 30-day interval after the index event. The mean acuity ratings were then regressed on the interval number; that is, the first 30 days was the first interval, 30 days thereafter was the second interval, and so forth. This procedure yielded a slope for each consumer indexing the average linear change in acuity per interval (18). A slope of 0, for example, readily identified someone whose acuity rating did not change after attaining two successive acuity ratings of 1 (the index event), whereas a large positive value indicated someone whose condition worsened considerably.
Note that the same analysis could have been performed using number of days, rather than the 30-day interval, as the predictor. We did the analysis both ways and obtained similar results. We focus on 30-day intervals because it seems conceptually more useful to consider change in functioning over a 30-day interval rather than change in functioning per day.
Finally, we evaluated the impact of seven graduation criteria by counting the number of people who met each criterion but later had an acuity rating of 3 or more (see Table 1). A rating of 3 was considered indicative of decompensation severe enough to warrant intensive case management. The seven graduation criteria were two acuity ratings of 1 on two successive dates following the index event, and maintenance of an acuity rating of 1 for one, two, three, four, and five consecutive intervals thereafter. Intervals with no acuity rating were considered not to have an acuity of 1. For example, someone with postindex acuity ratings of 1, 1, and blank would not meet the graduation criterion of three postindex acuity ratings of 1. An interval could be blank because the previous interval contained the last event recorded for that person—that is, the person graduated or was discharged for an administrative reason. An interval could also be blank because of missing data or because subsequent service events for that individual fell beyond the cutoff date for the data set.
Results
During the 29 months for which data were available, 112 people were discharged, having met the graduation requirement of an acuity rating of 1 for six consecutive months. Four of these people (4 percent) were readmitted.
For 46 of the 87 consumers for whom ratings were recorded after the index event (53 percent), slopes were equal to zero, indicating that they maintained a high level of functioning after the index event—that is, their acuity ratings never deviated from 1. For 17 consumers (20 percent) the slopes were negative, indicating that shortly after the index event their level of functioning decreased but then gradually improved again. Of the 17 consumers, 14 (82 percent) had an acuity rating of 1 by the end of the period for which data were available, and six (35 percent) had graduated. One of the 17 was discharged from the program after admission to a long-term care facility, and two were discharged because they could not be located.
For 24 consumers (28 percent) slopes were positive, indicating decreasing levels of functioning after the index event. However, even this group had relatively low acuity ratings by the end of the period for which data were available. Half had acuity ratings of 1 or 2; only 4 had acuity ratings greater than 3. One consumer in this group had graduated; however, four others were in long-term-care facilities (nursing homes or hospitals), and one was in prison.
The mean±SD number of days to reach the index event for persons in the negative, positive, and zero slope groups were 264.6±150.7, 236.2± 155.25, and 315±162.9, respectively. Differences between these means were not statistically significant.
Finally, Table 3 shows the number of persons who met each of seven potential graduation criteria—that is, an acuity rating of 1 on two successive dates following the index event and maintenance of a rating of 1 for one, two, three, four, five, and six consecutive intervals thereafter. The number of consumers for whom data were available varied considerably across intervals. As noted above, an interval could be blank for one of three reasons. First, the previous interval may have contained the last event recorded for that person: 43 consumers (49 percent) graduated and 11 (13 percent) were discharged for administrative reasons (one went to jail, one moved, five entered long-term-care facilities, two could not be located, and one refused all services). Second, some cases were active but no event with an acuity rating was recorded during the interval. Third, some cases were still active, but subsequent service events fell beyond the cutoff date for the data set (33 consumers, or 38 percent).
Discussion and conclusions
During the 29-month study period, 112 people graduated from the Denver case management program, and only four (4 percent) decompensated and were readmitted. This low rate must be interpreted within the context of the program's operating characteristics. In addition to case management provided directly by the Denver program, with a few exceptions consumers simultaneously received the typical array of outpatient services provided by community mental health centers in the late 1980s. Graduation thus did not result in a consumer's being cut off from services or having to form new relationships with treatment staff. Given the ongoing relationships with community mental health centers, consumers who met the criterion of having an acuity level of 1 for six consecutive months should have been able to maintain their gains in the more traditional office-based approach (3).
The decompensation rate is also based on variable periods of time and includes only persons whose cases were reopened. No doubt some graduates decompensated but were not referred back to the program because they were incarcerated. Others may have moved or died, but we have no way of knowing how many because data were available only through the 29th month of program operation.
For the vast majority of people who attained two successive acuity ratings of 1 (the index event), subsequent trajectories were also more stable than might have been expected. Approximately 46 of the 87 persons (53 percent) achieving this goal never deviated from an acuity level of 1. For these individuals, the Denver program's graduation criterion of six consecutive months at an acuity level of 1 was probably too conservative. Of the 17 persons (20 percent) whose conditions worsened shortly after they attained two successive acuity ratings of 1 but later improved again, only five (29 percent) had an acuity value of 3 or more during the six months after the index event. Even for the 24 people (28 percent of the 87 people) whose conditions increasingly worsened, ten (42 percent) never had an acuity value greater than 3 during the subsequent six-month period.
If a program were to adopt the index acuity event as a graduation criterion—that is, two consecutive ratings of 1—the data in Table 3 indicate that a little more than a third of the consumers would have graduated, later decompensating to the point of needing to be readmitted. This prediction assumes that an acuity rating of 3 or more indicates decompensation requiring intensive case management. The readmission rate decreases to less than 5 percent if the graduation criterion is set to five consecutive months at an acuity rating of 1. It is important to remember that a consumer had to have successfully achieved stability in each domain for more than three months to be given a rating of 1 (see Table 1). Thus a three-month cushion is already built into the scale.
Because of managed care pressures, programs have experimented with different graduation criteria. Studies to date have focused on estimating the deleterious effects of what some may consider premature graduation. No studies, to our knowledge, have examined at what point continued membership in an intensive case management program impedes the recovery process. The optimal graduation criterion would seem to be one that both promotes recovery and minimizes the probability of decompensation after graduation.
If one puts the issue of impediment to recovery aside, there may be no downside to ultraconservative graduation criteria that are essentially equivalent to lifelong participation in case management programs. Extended involvement in intensive case management may be considered inefficient only if caseload size is not allowed to increase according to case mix or if no standards are set for how frequently someone needs to be seen.
Recently, efforts to identify the key ingredients in intensive case management programs have increased (21) so that positive effects can be maximized and costs reduced. For the same reasons, efforts must also increase to determine the appropriate intensity and duration of case management. One issue that warrants investigation is the factors that predict who is likely to decompensate if a lenient graduation criterion is adopted. Such knowledge would help reduce the negative effects of such a criterion. It may also allow more accurate prediction of the duration of services needed and thus provide the ability to set more appropriate caseload sizes.
Dr. Sherman is president of Resources for Human Service Managers, Inc., and associate clinical professor of psychiatry at the University of Colorado Health Sciences Center. Dr. Ryan is assistant professor of psychology in the department of psychology at the University of Pittsburgh, Pittsburgh, Pennsylvania 15260 (e-mail, [email protected]). Send correspondence to Dr. Ryan.
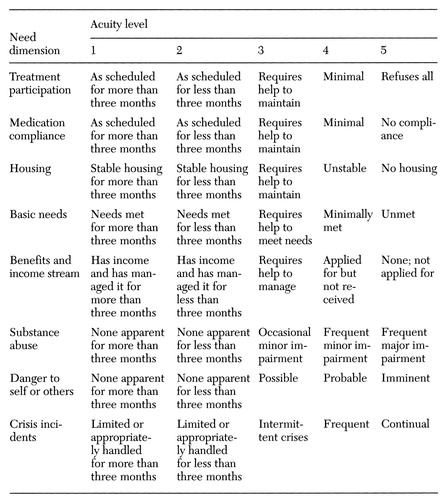 |
Table 1. The Denver Acuity Scale
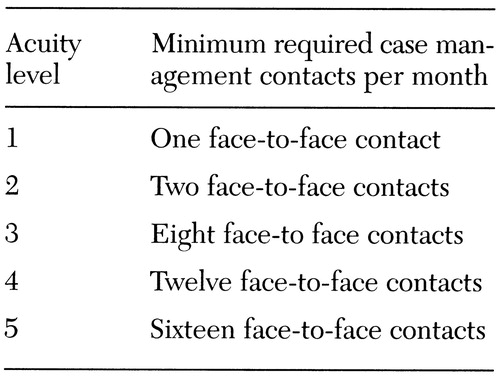 |
Table 2. Standards for frequency of contact with consumers in a case management program based on their global acuity rating
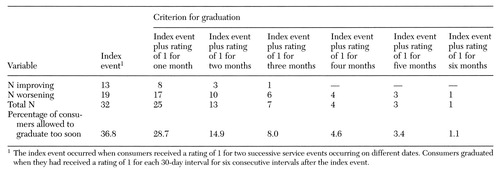 |
Table 3. Consumers in a case management program who would have been readmitted to the program after graduation at the indicated criterion for graduation
1. Desi PA, Santos AB, Hiott W, et al: Dissemination of assertive community treatment programs. Psychiatric Services 46:676-678, 1995Link, Google Scholar
2. Dixon LB, Krauss N, Kerman E, et al: Modifying the PACT model to serve homeless persons with severe mental illness. Psychiatric Services 46:684-688, 1995Link, Google Scholar
3. McRae J, Higgins RN, Lycan C, et al: What happens to patients after five years of intensive case management stops? Hospital and Community Psychiatry 41:175-179, 1990Google Scholar
4. Smukler M, Sherman P, Srebnik D, et al: Developing local service standards for managed mental health services. Journal of Administration and Policy in Mental Health 24:101-116, 1996Crossref, Google Scholar
5. Uehara E, Smukler M, Newman FN: Linking resource use to consumer level of need: field test of the LONCA method. Journal of Consulting and Clinical Psychology 62:695-709, 1994Medline, Google Scholar
6. Sherman PS, Dahlquist B: Accountability in managed care. NAMI Advocate, July-Aug 1996, pp 4-6Google Scholar
7. McGrew JH, Bond GR, Dietzen, L, et al: Measuring the fidelity of implementation of a mental health program model. Journal of Consulting and Clinical Psychology 62:670-678, 1994Crossref, Medline, Google Scholar
8. Breckke JH, Test MA: A model for measuring the implementation of community support programs: results from three sites. Community Mental Health Journal 28:227-247, 1992Crossref, Medline, Google Scholar
9. Teague GB, Drake RE, Ackerson TH: Evaluating use of continuous treatment teams for persons with mental illness and substance abuse. Psychiatric Services 46:689-695, 1995Link, Google Scholar
10. Dietzen LL, Bond GR: Relationship between case manager contact and outcome for frequently hospitalized psychiatric clients. Hospital and Community Psychiatry 44:839-843, 1993Abstract, Google Scholar
11. Durbin J, Goering P, Wasylenki D, et al: Who gets how much of what? A description of intensive case management. Psychiatric Rehabilitation Journal 20(3):49-56, 1997Google Scholar
12. Harding CM, Brooks GW, Takamaru A, et al: The Vermont longitudinal study of persons with severe mental illness: II. long-term outcome of subjects who retrospectively met DSM-III criteria for schizophrenia. American Journal of Psychiatry 144:727-735, 1987Link, Google Scholar
13. Anthony WA: Recovery from mental illness: the guiding vision of the mental health service system in the 1990's. Psychosocial Rehabilitation Journal 16(4):11-23, 1993Google Scholar
14. Solomon P: The efficacy of case management services for severely mentally disturbed clients. Community Mental Health Journal 28:163-180, 1992Crossref, Medline, Google Scholar
15. Burns BJ, Santos AB: Assertive community treatment: an update of randomized trials. Psychiatric Services 46:669-675, 1995Link, Google Scholar
16. McGrew JH, Bond GR, Dietzen L, et al: A multisite study of client outcomes in assertive community treatment. Psychiatric Services 46:696-701, 1995Link, Google Scholar
17. Sherman PS: A micro-based decision support system for managing aggressive case management programs for treatment resistant consumers, in State Management Information Systems in the West: Trends and Developments. Edited by Greenhalgh J. Boulder, Colo, Western Interstate Commission for Higher Education, 1988Google Scholar
18. Ryan CS, Sherman PS, Bogart LM: Patterns of services and consumer outcome in an intensive case management program. Journal of Consulting and Clinical Psychology 65:485-493, 1997Crossref, Medline, Google Scholar
19. Sherman PS, Porter R: Mental health consumers as case management aides. Hospital and Community Psychiatry 42:494-498, 1991Abstract, Google Scholar
20. Ryan CS, Sherman PS, Judd CM: Accounting for case manager effects in the evaluation of mental health services. Journal of Consulting and Clinical Psychology 62:965-974, 1994Crossref, Medline, Google Scholar
21. McGrew JH, Bond GR: Critical ingredients of assertive community treatment: judgments of the experts. Journal of Mental Health Administration 22:113-125, 1995Crossref, Medline, Google Scholar



