Datapoints: Psychotropic Drug Utilization Among Elderly Nursing Home Residents in the United States
Psychotropic drug use has been a concern because of extensive misuse of these agents in nursing homes. The Omnibus Budget Reconciliation Act of 1987 made a significant impact on the use and monitoring of psychotropic agents in nursing homes ( 1 ). However, limited recent data exist regarding overall psychotropic drug use patterns in nursing homes. The objective of this national study was to examine overall psychotropic drug use patterns among elderly nursing home residents.
This study involved a cross-sectional analysis of the 2004 National Nursing Home Survey (NNHS), a nationally representative sample survey that includes detailed prescription utilization data of medications administered in the 24 hours before the interview and those taken by the residents on a regular basis for the past month ( 2 ). The study sample included elderly nursing home residents aged 65 years or older. Descriptive weighted analysis, including 95% confidence intervals (CIs), was used to examine prevalence patterns of psychotropic use.
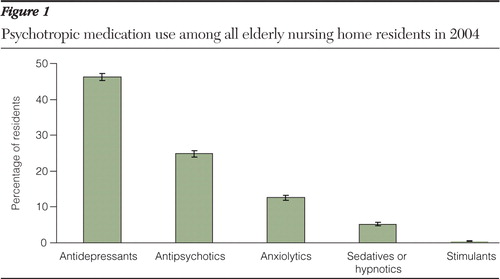
According to the 2004 NNHS, an estimated .83 million (CI=.82–.85) elderly nursing home residents received at least one psychotropic medication, for an overall prevalence of 63.2% (CI=62.2%–64.2%). As reported in Figure 1 , antidepressant agents were the most prescribed psychotropic class (46.2% of all elderly nursing home residents), followed by antipsychotics (24.8%) and anxiolytics (12.6%).
Selective serotonin reuptake inhibitors (SSRIs) were the most commonly prescribed antidepressant agents (31.1% of residents). Second-generation antipsychotic agents were used by 23.5% of residents. With respect to anxiolytics and sedatives, short-acting benzodiazepines were the most highly prescribed agents (8.1% of residents). Long-acting benzodiazepines were given to 3.4% of residents.
The study found that nearly two-thirds of elderly nursing home residents received psychotropic medications. The high psychotropic drug use can be attributed to use of SSRIs and second-generation antipsychotics. With increasing concerns about inappropriate psychotropic use, there is a strong need to monitor their usage in nursing homes. The recent regulations in nursing homes could be instrumental in improving the quality of geriatric care ( 1 ).
Acknowledgments and disclosures
The authors report no competing interests.
1. Hughes CM, Lapane KL: Administrative initiatives for reducing inappropriate prescribing of psychotropic drugs in nursing homes: how successful have they been? Drugs and Aging 22:339–351, 2005Google Scholar
2. National Nursing Home Survey Documentation. Atlanta, Ga, Centers for Disease Control and Prevention, 2004. Available at ftp://ftp.cdc.gov/pub/Health_Statistics/NHS/Dataset_Documentation/NNHS/nnh04 Google Scholar



