Mental Health Service Use and Outcomes After the Enschede Fireworks Disaster: A Naturalistic Follow-Up Study
On the afternoon of May 13, 2000, a fireworks deposit situated in a residential area exploded, killing 22 people and injuring about 1,000 in the center of Enschede, a town in the east of the Netherlands. As a result approximately 1,500 houses were damaged, of which 498 had to be demolished, leading to displacement of 4,163 inhabitants ( 1 ). An estimated 17,000 individuals were probably exposed in one way or another to this disaster ( 1 ). The event was immediately declared a national disaster. In response, a nationwide support effort was launched and funds were allocated for research to document health consequences of this disaster. As a result, data about health, well-being, and medical service use have been systematically collected since the early days after this event ( 2 , 3 , 4 , 5 ).
In contrast to the wealth of publications about the epidemiology of mental health problems after a disaster ( 6 , 7 ), there are only few studies that describe help-seeking behavior for these problems in a population stricken by disaster, or the outcomes of interventions. In this article we present the results of a chart study and interviews in early and later phases of treatment of adults who sought help from mental health services for disaster-related problems. The aim of the study was to evaluate mental health service delivery to persons affected by the fireworks disaster in Enschede during the period from May 2000 to May 2005. This study documented the number of people seeking help for disaster-related psychological problems, their sociodemographic and diagnostic characteristics, the interventions that they received, and some results of these interventions. To our knowledge this is the first systematic investigation of all adults seeking specialized mental health care in a disaster-stricken area.
Methods
Treatment settings
In the first week after the explosion, the regional mental health care institute, which has a catchment area of 390,000 and about 6,000 referrals a year, organized a special outpatient team to provide evidence-based therapies for people who experienced disaster-related mental health problems. Apart from supportive counseling, no specific early interventions, such as critical incident debriefing, were offered ( 8 ). No other specialized disaster-related mental health services were available in the region. As far as could be ascertained, approximately 95% of all people who sought help for disaster-related mental health problems, other than in primary care, did so from the specialized fireworks disaster team ( 2 ). The central element in the protocol consisted of brief eclectic psychotherapy for posttraumatic stress disorder (PTSD), which consisted of psychoeducation, imaginary exposure, writing assignments, and a closing ritual ( 9 ). In addition, cognitive-behavioral treatment (CBT) ( 10 ), eye movement desensitization and reprocessing (EMDR) ( 11 ), general supportive counseling, and pharmacological treatment were available. An algorithm was formulated to guide choice of treatment during a dialogue with the patient. If disorders other than those directly related to the disaster, such as psychosis or addiction, were on the forefront, these were treated first.
Data collection
Two methods of data collection were used. The first was routine registration of all service contacts on a monthly basis and the systematic coding of data from the medical charts of all patients who came to the disaster relief service between May 13, 2000, and June 1, 2004. All relevant medical information was recorded in the charts according to a prescribed format. The end of the follow-up period was May 1, 2005. The following data were extracted from the medical charts: demographic information, medical history, material or financial damage as a result of the disaster, initial complaints, clinical diagnosis, duration of treatment and number of contacts, number of unfulfilled appointments, number of treatment episodes (a new episode was documented when more than three months passed between two contacts), type of treatment (psychotherapy according to the protocol, supportive psychotherapy, or medication), and recovery as assessed by the clinician. Clinical diagnoses based on DSM-IV criteria were determined in consensus meetings by experienced clinicians on the basis of semistructured data gathered at intake. "Recovery" was coded if the therapist explicitly reported in the chart or in a letter to the family physician that complaints observed at onset were in remission at discharge.
The second method of data collection consisted of a structured diagnostic interview and a number of self-report questionnaires. The aim of this part of the study was to evaluate diagnoses and outcomes of the treatment protocol more systematically. All patients who completed a minimum of eight sessions of treatment and were still in treatment after May 1, 2001—or entered treatment after this date—were asked to provide informed consent for the interview study by their therapist. The cutoff of eight sessions was based on previous disaster studies ( 12 ), which showed that if individuals are asked to participate in a research project too early the response rate is low. This part of the study started in May 2001 and included patients until June 1, 2004. The end of the follow-up was April 1, 2005.
For eligible adult patients who consented to participate in the interview study, the Dutch 12-month version of the Composite International Diagnostic Interview (CIDI) ( 13 ) was administered by experienced research assistants trained in the instrument. Overall severity of psychological complaints was measured with the Symptom Checklist-90 (SCL-90), with a cutoff of >170 for men and >204 for women to indicate high levels of distress ( 14 ). Severity of experienced posttraumatic stress was measured with the Self-Rating Scale for PTSD (SRS-PTSD) ( 15 ). Social span of activities was measured with the 36-item Short-Form Health Survey (SF-36) ( 16 ), with a cutoff of <40 to indicate poor quality of life.
The CIDI and the questionnaires were first administered around the eighth treatment session, which was a mean±SD of 3.0±1.3 months after treatment started (in one case administration was at six months). Nine months after treatment ended, a follow-up interview was conducted. Patients who stayed in treatment for more than two years received a final examination at the end of the two-year period. "Healthy" in the interview study was defined as scores at the last assessment that were below the cutoff scores for the SCL-90 and SRS-PTSD or above the cutoff score for the SF-36. The study was approved by the ethics committees of the general and psychiatric hospital of the city of Enschede, and all interviewed participants gave written informed consent.
Analyses
Absolute numbers of disaster-related referrals from May 2000 until June 2004 were used as numerators to calculate four-year cumulative incidence of referrals, with the estimated total number of probably exposed persons as the denominator ( 1 ). All further analyses were based on data from patients who underwent the intake procedure and for whom sufficient information was available for analysis. Differences in counts within various subpopulations were tested with chi square analysis or Student's t test. For the SCL-90, SRS-PTSD, and SF-36, values were replaced by a casewise series mean when less than 20% of data were missing in a subscale.
Results
Between May 13, 2000, and June 1, 2004, there were 1,906 referrals to the specialized disaster team, consisting of 1,659 persons, including adults and children. On average, disaster-related referrals constituted 5.7% of the total number of referrals to the mental health care institute over the five-year period. The peak of disaster-related referrals occurred in the second year after the disaster (N=543, or 7.9% of all institute referrals). It is interesting that the overall number of referrals during the first year after the disaster dropped by nearly 20% compared with the previous year (1999), only to rise above baseline numbers in the second and third year. Especially high numbers of referrals were seen in month 24 (N=55) and month 32 (N=46) after the disaster. The first peak coincided with a claim procedure that started at month 24 after the disaster. The second peak occurred after an advertising campaign was launched to inform the general public that psychological support was available.
On the basis of the 1,659 referred persons and an estimate of 17,000 probably exposed inhabitants ( 1 ), which included the 4,163 displaced persons, the four-year cumulative referral-incidence was 98 persons per 1,000 of the total exposed population (95% confidence interval=94–102). Of the 460 persons who initially accompanied an individual seeking treatment, 228 also received some form of treatment themselves, either in partner-relationship therapy (N=162) or individually (N=66). This group was not further examined in this study. Also not included were the 315 children who were referred to the service, 235 of whom (75%) received treatment, and 73 adults who were referred but who did not visit the center. This left a sample of 811 adult patients. [A flowchart showing the various groups is available as a supplement to this article at ps.psychiatryonline.org .]
Of these 811 adult patients, 148 (18%) underwent only part of the intake procedure and did not enter treatment. A total of 663 adults entered treatment. Of the 663 patients, 211 (32%) dropped out very soon after intake; thus 452 adults (68%) entered the active treatment phase. In 95% of these cases (N=627), adequate information about the treatments provided could be extracted from the medical charts. For 548 patients (83%) the treatment algorithm was completed, and for 524 patients (79%) the chart information was sufficient to encode treatment outcome. In the assessment window between May 1, 2001, and June 1, 2004, a total of 394 persons completed eight or more sessions. Of these, 271 participated in the interview study (69%).
Table 1 provides data on demographic and diagnostic characteristics of and treatments provided to the 663 adult patients who entered treatment, as well as the 271 who participated in the interview study and the 392 who did not.
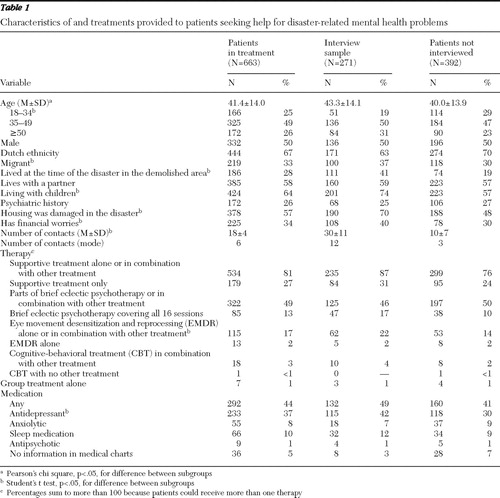 |
Compared with the group of patients who did not participate in the interview study, the interview group had fewer persons aged 18 to 34 years ( χ2 =8.8, df=3, p<.025); in addition, the interview group had more migrants ( χ2 =17.6, df=1, p<.001), more persons from the demolished area ( χ2 =25.3, df=1, p<.001) or with demolished houses ( χ2 =47.6, df=1, p<0.001), more persons living with children ( χ2 =30.9, df=1, p<.001), and more persons with financial worries ( χ2 =15.6, df=1, p<.001). Persons in the interview group were somewhat older (t=2.7, df=661, p<.05) and received far more treatment sessions (t=28.9, df=661, p<.001).
Supportive treatment, often in combination with other types of treatment, was the most common type of treatment used. Brief eclectic psychotherapy was the most common type of psychotherapy offered, which was the intent of the protocol. However, the protocol (that is, brief eclectic psychotherapy in 16 sessions) was completed with only 13% of the patients, and often it was combined with supportive treatment. Overall, two-thirds of the 663 patients received some form of psychotherapy—that is brief eclectic psychotherapy, CBT, or EMDR. Forty-four percent received medication. In most cases, the medications were selective serotonin reuptake inhibitors or other antidepressants (37%) or sleep medication (10%). For the variables shown in Table 1 , the proportions in the interview group were generally similar to those in the entire sample. However, a greater proportion of patients in the interview group than in the group that was not interviewed received EMDR ( χ2 =21.3, df=1, p<.001) and antidepressants ( χ2 =26.3, df=1, p<.001).
Table 2 shows the clinical diagnoses for the total sample and the interview group. For the latter, CIDI diagnoses are also reported. A CIDI was completed for 228 of the 271 interviewed patients (84%). In the total sample, PTSD was by far the most common clinical diagnosis (53%, with 47% having PTSD as the main diagnosis), followed by adjustment disorders (23%, with 17% as the main diagnosis) and depressive disorders (19%, with 8% as the main diagnosis). Sixteen percent of the patients did not meet criteria for any clinical diagnosis. For 3% of the patients, insufficient information was available in the chart. For the interview sample the picture was similar. Of interest, however, on the basis of the CIDI diagnoses, depressive disorder was the most common disorder (58%), followed by PTSD (40%). The largest discrepancies between the clinical and standardized diagnosis were seen for somatoform disorder (4% and 35%), anxiety disorders (9% and 37%), and substance use disorders (2% and 27%), indicating these diagnoses may have been missed.
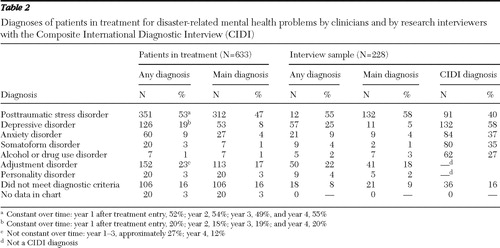 |
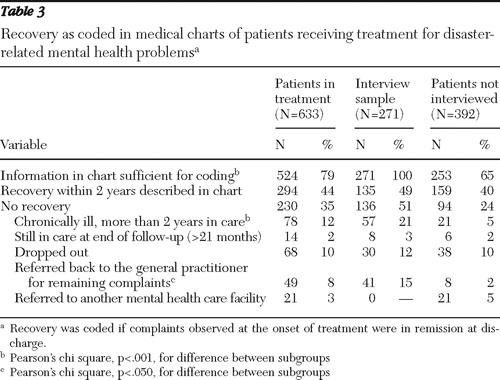
Table 3 presents information on recovery as recorded in the medical charts by clinicians. According to clinicians' chart notes, 294 of 524 patients recovered (56%, or 44% of the entire group). Of this entire group, 12% remained in care for more than two years, 8% were referred back to their family doctor, and 3% were referred to some other mental health program. In the interview group, clinically assessed improvement was reported for half of the patients (49%). Twenty-one percent continued after completion of the study, 15% were referred back to their family doctor, and 12% dropped out of treatment. Table 4 presents information on patients judged "healthy" on the basis of questionnaire scores. On the basis of questionnaire data, most patients (between 56% and 76%) had a "healthy" score at last assessment on all items except physical mobility and social role impairment. On the SCL-90, patients showed statistically significant improvement on all measured outcomes except for the hostility and somatic complaints subscales.
 |
 |
Discussion
The purpose of this study was to describe all persons who sought help at a specialized service for disaster-related mental health problems during four years after the devastating explosion of a fireworks deposit located in the center of Enschede, the Netherlands. To our knowledge few studies have documented the surplus incidence of psychopathology seen at mental health services after disasters. It is important to note that in the Netherlands these services are comprehensively covered by national insurance, and there were thus no financial barriers for anyone to visit the service. Other than primary care, no other services dealt with disaster-related problems, and other mental health services in the area directed people with these problems to the specialized service. The study thus provides a quite complete picture of all persons who sought help from mental health services for disaster-related problems in an affected region and describes the efficacy of mental health interventions in the real world under such circumstances.
This study is a relevant addition to the literature, which almost exclusively reports morbidity rates in the population at large ( 2 , 3 , 4 , 5 , 6 , 7 ) and results from treatment studies conducted under controlled conditions ( 10 , 11 ). This study showed that the extra influx of persons with mental health problems resulting from the disaster was limited in size; we found a four-year cumulative referral incidence of approximately 10% among the stricken population and an influx of disaster-related cases to the mental health services of 6% on average in the first five years after the event. This is a strikingly low figure compared with the estimations of 40% psychological morbidity in studies of disaster-stricken populations ( 6 , 7 ) and the estimated 30% in the Enschede population ( 2 ). Apparently, help-seeking behavior and referrals by general practitioners to mental health services for disaster-related mental health problems were relatively low ( 5 , 6 , 7 , 8 , 9 ).
We observed a recovery rate of approximately 50% on the basis of clinicians' reports, between 69% and 76% in symptoms, and between 39% and 60% in social and physical functioning on the basis of "healthy" scores at the final assessment. Even though these changes were all statistically significant, arguably the differences in scores between first and last measurement are modest. Recovery in terms of improved social function and physical mobility appears to have been less robust.
The study has several shortcomings. First, very little information is available about the persons who were seeking care in the first few months immediately after the disaster. During this period the registration system was not yet fully operational, and we have incomplete information about those who came to the service at that time. There is evidence that in the early days after the disaster many victims contacted their general practitioner ( 3 , 5 ).
A second shortcoming is the fact that only clinical information based on case notes is available for most of the patients. This source of information is notoriously incomplete and inconsistent at times. We were able to gather more in-depth material using standardized methods for only a much smaller group of patients—that is, those who received substantial treatment for disaster-related pathology. This limitation resulted from a decision made early in the study that provision of treatment should prevail over research interests and that patients would probably be more willing to participate in research once they had started actual treatment. Our response rate for the interview study was 69%, which is considerably higher than the 54% reported by Weisaeth ( 12 ). As a result of this decision the interviewed sample differed in several demographic and clinical characteristics. Also, the fairly high percentages of "healthy" scores at the onset of the questionnaire study and the relatively small difference in scores between first and last measurements are probably the result of late first assessments.
It should be noted, however, that the interview sample did not differ substantially from the total group of patients in clinical diagnoses, received treatments, and overall clinical outcomes. We believe, therefore, that the combination of case notes and questionnaires provided a fairly complete picture of service involvement in the aftermath of the disaster. The added value of the standardized assessment in the interview study is particularly clear for the diagnostic information; CIDI diagnoses indicated that disorders other than PTSD were quite common—and far more common than clinician diagnoses indicated. However, it must be noted that the CIDI interview took place several weeks after the clinical interview. Despite late assessment, the extent of the differences in our results seems to indicate that clinicians in this specialized service may have been focusing too much on PTSD and may have overlooked the presence of depression, anxiety, substance use disorders, and somatoform disorders. As a consequence, treatments were also largely oriented toward PTSD. It seems reasonable to assume that with a more accurate diagnosis and adequate treatment based on this diagnosis, better overall treatment results could have been achieved.
Conclusions
The study showed that apart from persons who sought support during the first few weeks after a disaster, the largest influx of patients with disaster-related mental health problems was noted after about a year. This delay gives services time to design an effective program for the treatment of expected psychological problems. On the basis of our experiences, an additional influx of 5% to 10% can be expected in comparable situations. The study demonstrated that most patients experienced a modest but significant positive effect from the interventions provided. Outcomes may be further improved if disaster mental health services focus less exclusively on PTSD and its treatment and take other common mental health problems into account.
Acknowledgments and disclosures
This study was financially supported by the Netherlands Ministry of Health and Welfare and by Mediant Institute for Mental Health Care, Enschede, the Netherlands. The authors thank C. J. Yzermans, M.Sc., Ph.D., for comments on the manuscript.
The authors report no competing interests.
1. Oosting M, Beckers-de Bruin MCB, Enthoven MEE, et al: National Committee Study Fireworks Disaster Final Report [in Dutch]. Dutch Ministry of Internal Affairs, DeN Haag, 2001. Available at www.rijksoverheid.nl/documenten-en-publicaties/publicaties-pb51/rapport-commissie-oosting-amp-apos-van-specifiek-naar-generiek-amp-apos.html Google Scholar
2. Van der Velden PG, Grievink L, Kleber RJ, et al: Post-disaster mental health problems and the utilization of mental health services: a four-year longitudinal comparative study. Administration and Policy in Mental Health 33:279–288, 2006Google Scholar
3. Yzermans CJ, Donker GA, Kerssens JJ, et al: Health problems of victims before and after disaster: a longitudinal study in general practice. International Journal of Epidemiology 34:820–826, 2005Google Scholar
4. Den Ouden DJ, Dirkzwager AJ, Yzermans CJ: Health problems presented in general practice by survivors before and after a fireworks disaster: associations with mental health care. Scandinavian Journal of Primary Health Care 23:137–141, 2005Google Scholar
5. Van der Meijden PA, Roorda J, Yzermans CJ, et al: Health Monitoring in the Exposed Population of the Enschede Fireworks Disaster [in Dutch]. Enschede, the Netherlands, Municipal Health Service Region Twente, 2006.Google Scholar
6. Norris FH, Freedman MJ, Watson PJ, et al: 60,000 disaster victims speak: part 1. an empirical review of the empirical literature, 1981–2001. Psychiatry 65:207–239, 2002Google Scholar
7. Norris FH, Freedman MJ, Watson PJ: 60,000 disaster victims speak: part 2. summary and implications of the disaster mental health research. Psychiatry 65:240–260, 2002Google Scholar
8. Rose S, Bisson J, Wessely S: A systematic review of single-session psychological interventions ("debriefing") following trauma. Psychotherapy and Psychosomatics 72:176–184, 2003Google Scholar
9. Gersons BPR, Carlier IVE (eds): Treatment Strategies in Post Traumatic Stress Disorders [in Dutch]. Houten, the Netherlands, Bohn, Stafleu, and van Lochem, 2000Google Scholar
10. Welch SS, Rothbaum BO: Emerging treatments for PTSD; in Handbook of PTSD: Science and Practice. Edited by Friedman MJ, Keane TM, Resick PA. New York, Guilford, 2007Google Scholar
11. Seidler G, Wagner F: Comparing the efficacy of EMDR and trauma-focused cognitive-behavioural therapy in the treatment of PTSD: a meta-analytic study. Psychological Medicine 36:1515–1522, 2006Google Scholar
12. Weisaeth L: Importance of high response rates in traumatic stress research. Acta Psychiatrica Scandinavica 80(suppl s355):131–137, 1989Google Scholar
13. Andrews G, Peters L: The psychometric properties of the Composite International Diagnostic Interview. Social Psychiatry and Psychiatric Epidemiology 33:80–88, 1998Google Scholar
14. Derogatis LR, Savitz KL: The SCL-90-R, Brief Symptom Inventory, and Matching Clinical Rating Scales; in The Use of Psychological Testing for Treatment Planning and Outcomes Assessment, 2nd ed. Edited by Maruish ME. New York, Erlbaum, 1999Google Scholar
15. Carlier IV, Lamberts RD, Van Uchelen AJ, et al: Clinical utility of a brief diagnostic test for posttraumatic stress disorder. Psychosomatic Medicine 60:42–47, 1998Google Scholar
16. Ware JE, Sherbourne CD: The MOS 36-item Short-Form Health Survey (SF-36): I. conceptual framework and item selection. Medical Care 30:473–483, 1992Google Scholar



