Unmet Need for Treatment of Major Depression in the United States
Studies throughout the 1980s and 1990s showed that a large proportion of individuals with major depression do not seek treatment ( 1 , 2 , 3 , 4 , 5 , 6 ). Although some studies found that low levels of perceived need for treatment and negative attitudes toward mental health treatments were more significant barriers to treatment seeking than system-level barriers ( 7 , 8 , 9 ), others found that characteristics of the health care system in general, and financial barriers in particular, were more prominent in this patient population ( 10 ).
More recent data suggest that the rate of treatment of depression in the community has increased ( 11 , 12 ). However, there are indications that the increased demand for treatment has coincided with a greater perception of financial barriers ( 13 )—a trend that is likely associated with the increased out-of-pocket cost of mental health care in recent years ( 14 , 15 , 16 ).
A better understanding of the extent of perceived unmet need for care among individuals with major depression, as well as its predictors and the reasons for unmet need, would have important implications for understanding the barriers to mental health treatment seeking and for designing programs to improve access to mental health care.
The study reported here used data from a large and nationally representative sample of U.S. adults to examine the extent and correlates of perceived unmet need for treatment among persons with major depression. More specifically, the study used regression models to examine sociodemographic, access, and clinical correlates of perceived unmet need for treatment among depressed adults whether or not they had had any mental health treatment contacts in the past year. The study also explored the reasons for not seeking needed treatment among those who perceived an unmet need for treatment.
Methods
Sample
The sample for the study was drawn from participants in the 2005 and 2006 National Survey on Drug Use and Health (NSDUH) ( 17 , 18 ). Overall, 74,192 adults were interviewed in these two surveys. (The response rates for the 2005 and 2006 survey were 76% and 74%, respectively.) Of the 73,583 participants who completed the questionnaire about major depressive episodes in 2005 or 2006, a total of 6,531 (7.1% weighted) met criteria for a major depressive episode in the past 12 months; 6,510 of these participants also responded to questions about treatment seeking and perceived unmet need and constituted the sample for this study.
Assessment
The presence of a major depressive episode in the past 12 months was assessed by using a structured interview based on DSM-IV criteria ( 19 ). Questions were adapted from the depression section of the National Comorbidity Survey Replication ( 20 ) and administered by using computer-assisted interviewing methods.
Perceived unmet need for mental health treatment was assessed with one question: "During the past 12 months, was there any time when you needed mental health treatment or counseling for yourself but didn't get it?" A positive response to this question was rated as perceived unmet need for treatment. This question was asked of all participants whether or not they had sought treatment in the past year. (Respondents were not asked specifically about unmet need for treatment of depression.)
Reasons for not seeking treatment were assessed for those who reported an unmet need. Participants were presented with a series of statements about why they did not get needed mental health treatment or counseling. The reasons included inability to afford the cost, concern about opinions of neighbors or the community, concern about the effect of treatment seeking on the person's job, lack of health insurance coverage, inadequate health insurance coverage, lack of knowledge about where to go for services, concern about confidentiality, fear of being committed to a psychiatric hospital or having to take medicine, the person's belief that he or she could handle the problem without treatment, a belief that treatment would not help, lack of time, a desire not to have others find out, lack of transportation, too great a distance to treatment or inconvenient hours, and other reasons. For these analyses, lack of insurance and inadequate insurance coverage were combined, as were concerns about opinions of neighbors and community and not wanting others to find out.
Treatment seeking was assessed by a series of questions. Participants were asked whether at any time in the past 12 months they had seen or talked to a medical doctor or other professional about their depressive symptoms. Participants who responded positively to this question were presented with a list of professionals and asked to identify the professional or professionals whom they had seen or talked to about their depressive symptoms. The list included nonpsychiatrist physicians, psychiatrists, psychologists, social workers, counselors, and other health professionals (for example, nurses and occupational therapists). Religious helpers and nontraditional helpers (for example, herbalists, chiropractors, and acupuncturists) were also included.
The extent of outpatient service use was ascertained by asking participants about the number of visits over the past year. Consistent with past research ( 21 , 22 ), the variable was dichotomized into fewer than four visits and four or more visits in the past 12 months.
Participants were asked whether in the past 12 months they had taken any medication that was prescribed for their mood symptoms. Participants were also asked about inpatient hospitalizations for mental health reasons in the past 12 months.
Impairment in role functioning associated with depression was assessed by four questions from the Sheehan Disability Scale (SDS) ( 20 , 23 ), a measure of the impact of depression on a person's daily activities in four domains of life. Participants were asked to think about the time in the past 12 months when problems with mood were the worst and to rate the degree of impairment in "chores at home," "ability to do well at school or work," "ability to get along with family," and "social life" on a scale from 0 to 10 (0, no impairment; 1 to 3, mild impairment; 4 to 6, moderate impairment; 7 to 9, severe impairment; and 10, very severe impairment). An overall role impairment score is defined as the highest level of severity of impairment reported in any of the four domains. In addition, the total number of lifetime depressive episodes was ascertained, and on the basis of the median split, the variable was dichotomized as fewer than five episodes and five or more episodes.
Severity and level of distress were also measured by using K6 ( 24 , 25 ), a six-item screening instrument for nonspecific psychological distress during the worst month in the past 12 months. Possible scores on K6 range from 0 to 24. A score of 13 or higher has been found to correspond to clinician-rated measures of serious mental illness as ascertained by a semistructured interview instrument ( 25 ).
In addition, participants' age, gender, family income, insurance type, and the extent of insurance coverage in the past year were ascertained. Coverage was dichotomized as coverage throughout the year and any period without coverage in the past year.
Statistical analyses
Analyses were conducted in two stages. First examined was the association between perceived unmet need for treatment and specific sociodemographic, access, service use, and clinical characteristics among adults who reported a major depressive episode. These analyses used bivariate and multivariate logistic regression models. The analyses were conducted separately for participants who did or did not seek treatment in the past 12 months.
Second, the percentage of participants who reported different reasons for not seeking treatment when they needed it was examined. These analyses were limited to those who reported unmet need for treatment. The analyses were conducted for the entire group of adults with a major depressive episode and then separately for individuals who did or did not seek treatment in the past 12 months.
Analyses were conducted using Stata 10, which adjusts for the complex sampling design of the NSDUH. All percentages were weighted by sampling weights, and only weighted percentages are reported here. A significance level of <.05 was used.
Results
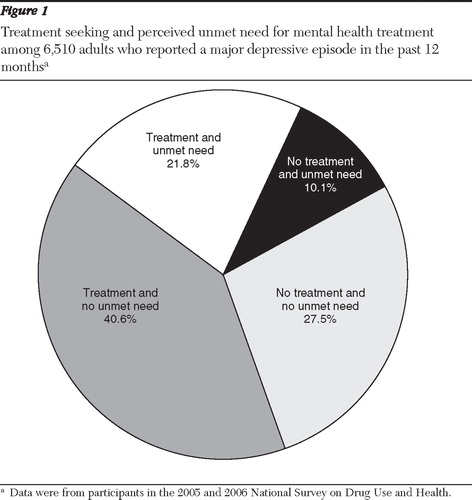
Of the 6,510 participants who reported a 12-month major depressive episode in the 2005 and 2006 NSDUH surveys, 3,568 (62.4%) reported seeking mental health treatment in the past 12 months and 2,942 (37.6%) reported that they did not seek treatment. Furthermore, 2,354 (31.9%) reported an unmet need for treatment, and 4,156 (68.1%) did not report an unmet need. Overall, 72.5% of this sample of adults with a major depressive episode either sought treatment, perceived an unmet need for treatment, or both ( Figure 1 ).
Correlates of perceived unmet need
Among the 3,568 adults with a 12-month major depressive episode who sought treatment, 1,432 (34.9%) reported an unmet need for treatment. Among the 2,942 who did not seek treatment, 922 (26.8%) reported an unmet need.
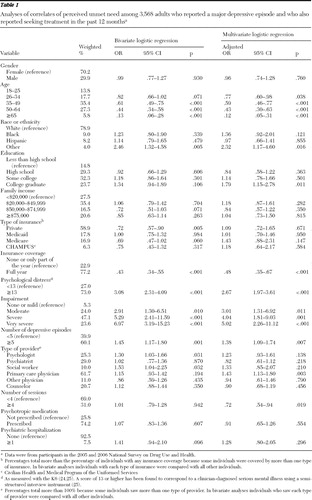
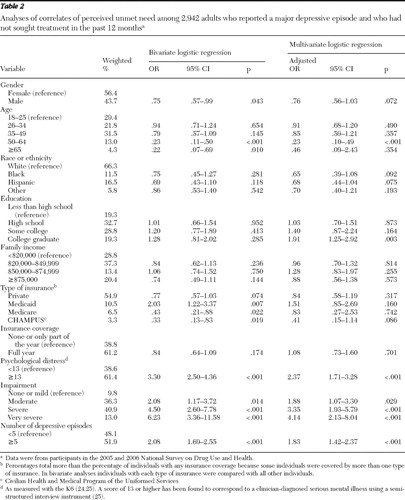
Sociodemographic, access, and clinical variables that were correlated with perceived unmet need among participants who sought treatment are presented in Table 1 . Table 2 presents these correlates among participants who did not seek treatment.
 |
 |
The bivariate analyses indicated that among participants who sought treatment in the past 12 months, age, racial-ethnic group, type of insurance, extent of insurance coverage, psychological distress, impairment in role functioning, number of depressive episodes, and type of provider were associated with perceived unmet need ( Table 1 ). Variables that remained significant in the multivariate model were age, racial-ethnic group, the extent of insurance coverage, psychological distress, impairment, number of depressive episodes, and type of provider ( Table 1 ). In addition, education and number of outpatient sessions in the past year became significant in the multivariate model. Participants who were older than 25 years, those with full-year insurance coverage, and those who had had more than four outpatient mental health visits were significantly less likely to report an unmet need, whereas participants from the "other" racial-ethnic group, college graduates, those with more distress or impairment, those with a greater number of depressive episodes, and those who had seen a primary care physician for their mental health problems were more likely than other participants to report an unmet need ( Table 1 ).
Among participants who did not seek treatment, gender, age, type of health insurance, psychological distress, impairment in role functioning, and number of depressive episodes were associated with perceived unmet need in bivariate analyses ( Table 2 ). Variables that remained significant in the multivariate model were age, distress, impairment, and number of depressive episodes. Participants in the 50- to 64-year age group were less likely than those in the 18- to 25-year group to perceive an unmet need, whereas participants with a greater level of distress or impairment in role functioning and those with a greater number of depressive episodes were more likely to perceive an unmet need. In addition, having a college education was significantly associated in the multivariate model with perceiving an unmet need ( Table 2 ).
Reasons for not seeking treatment
Across both groups of participants with a major depressive episode who did and did not seek treatment, concerns about cost were the major reason for perceived unmet need; this reason was reported by 46.0% of the total group ( Figure 2 ). The percentage of participants who reported cost concerns was larger among those who did not seek treatment than among those who did (53.9% compared with 42.4%; design-based F=12.23, df=1 and 60, p<.001).
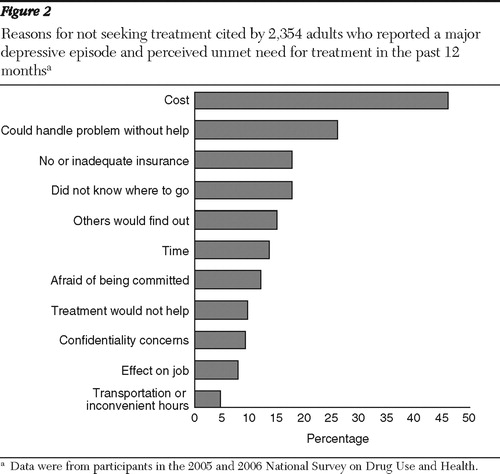
Participants who did not seek treatment were also more likely than those who did to report concerns about confidentiality (12.2% compared with 8.0%; design-based F=5.40, df=1 and 60, p=.024) and concerns about neighbors or other people finding out (18.7% compared with 13.2%; design-based F=5.70, df=1 and 60, p=.020). Participants who sought treatment were more likely than those who did not to report concerns about transportation or inconvenience (5.8% compared with 2.9%; design-based F=4.16, df=1 and 60, p=.046). The percentages of participants who reported that they believed they could handle the problem on their own were similar in the groups with and without a history of treatment seeking (25.6% and 26.5%, respectively); the percentages reporting that treatment would not help were the same in both groups (9.6%), as were the percentages of participants who reported other reasons for not seeking treatment.
Discussion
The results of this study should be viewed in the context of its limitations and the limitations of the NSDUH data. First, this study did not examine correlates of treatment seeking for depression per se. Such a study would likely have revealed significant differences in gender, racial-ethnic group, and other sociodemographic characteristics between persons with depression who did and did not seek treatment. These differences have been explored extensively in past research ( 12 , 20 , 26 ). Instead the study sought to examine the correlates of perceived unmet need for treatment within groups of participants with major depression who had or had not sought mental health treatment. Second, the study focused on major depression, which is among the most disabling and severe mental health conditions. Barriers to seeking mental health treatment might vary according to severity of mental health conditions. Third, treatment seeking is not equivalent to having received adequate treatment ( 27 ). Unfortunately, NSDUH does not provide data beyond number of visits to assess the quality or intensity of mental health treatments received. Fourth, the NSDUH data are cross-sectional and do not cover timing of events. Therefore, causal relationships cannot be established in these data. Thus, for example, the association of number of outpatient visits with perceived unmet need may be a result of early drop-out from treatment among participants who believed that treatment did not meet their needs, or fewer visits may be a cause of perceived unmet need. Fifth, perceived unmet need is not equivalent to objectively assessed unmet need. However, among persons who seek treatment, perceived unmet need constitutes an important dimension of their views of adequacy and quality of treatments, and among those who have not yet sought treatment, it provides important information about demand for services. Furthermore, perceived unmet need for treatment was strongly correlated with level of distress and impairment in role functioning in this study, and similar correlations have been found in past research ( 28 ).
In the context of these limitations, the data presented provide useful information on correlates of perceived unmet need and barriers to treatment in a sample of persons with a major depressive episode from one of the largest mental health surveys of the U.S. general population. This study had three main findings. First, almost three-fourths of adults who reported a major depressive episode in the past year either sought mental health treatment or perceived an unmet need for such treatment. This rate is higher than those in previous community studies ( 29 , 30 ) and indicates an increase in the perceived need for care and in treatment seeking in the U.S. population, at least among individuals with depression. This trend is consistent with other time-trend studies of mental health treatment seeking for depression ( 11 ) and other common mental health problems ( 13 , 31 ). The trend may be attributable to increased knowledge about mental disorders ( 32 ), reduced stigma associated with mental health treatment seeking ( 33 ), or increased demand for and supply of psychiatric medications ( 34 ). It is notable that among participants with major depressive episodes who reported any mental health treatment seeking, 74.2% reported receipt of a prescription for a psychotropic medication ( Table 1 ).
Although increased rates of mental health treatment seeking are encouraging, it is notable that a large majority of persons who sought any treatment made fewer than four outpatient visits in the past year—which is generally considered the minimum number of visits required for adequate management of depression in outpatient settings ( 21 , 22 ). In addition, most sought treatment from primary care physicians. In the analyses, both these factors were associated with higher perceived unmet need for treatment ( Table 1 ).
Past research has generally found that compared with psychiatrists, general medical providers are less accurate in diagnosing mental disorders and tend to provide treatments with lower intensity than required by evidence-based standards ( 35 , 36 , 37 ). However, provision of mental health treatment by general medical providers expands available services in the community and increases the number of individuals who receive treatment. Future research should examine the impact of the expansion of mental health treatments in the general medical sector on outcomes of common psychiatric disorders in the community.
The second finding of the study was that a large percentage of participants with a major depressive episode reported an unmet need for mental health treatment, whether they received treatment or not. More than one-fourth of participants who did not seek any treatment and one-third of those who sought treatment reported an unmet need for treatment. In both groups, participants with a college education, more distress and impairment, and a greater number of past depressive episodes were more likely to perceive an unmet need. Although the association with distress, impairment, and number of depressive episodes likely reflects severity of depressive illness, the association with higher education may reflect more favorable attitudes toward receiving treatment and, among participants who sought treatment, a demand for more or better treatments.
There were also differences between the groups who did and did not seek treatment with regard to correlates of perceived unmet need. Among participants who sought treatment, those from the "other" racial-ethnic group were more likely to perceive an unmet need, whereas those with health insurance coverage for the full year were less likely to perceive an unmet need. Most past studies of racial-ethnic differences in receipt of mental health treatment have found differences between blacks and Hispanics compared with the white majority group ( 38 , 39 , 40 , 41 , 42 , 43 ). The study reported here found no such differences in the extent of perceived unmet need for treatment. Some studies have also found disparities in quality of and satisfaction with treatment between racial-ethnic groups categorized as "other" and the white majority group ( 44 , 45 ). The heterogeneous composition of the "other" racial-ethnic group in the study reported here further complicates interpretation of the findings. Future studies with even larger samples of persons with depression from "other" minority groups are needed to further explore their treatment experiences.
The association of perceived unmet need with the extent of insurance coverage among participants who sought treatment highlights the impact of financial barriers on the receipt of mental health care. An association between insurance coverage and treatment seeking has been consistently noted over the years ( 46 , 47 ). Health insurance coverage is likely a more critical factor in access to appropriate health care among persons with disabilities and persons who are poor because both groups have fewer available resources ( 48 ). Furthermore, with the growing cost of mental health care, lack of adequate health insurance coverage will likely feature even more prominently in coming years as a barrier to accessing mental health treatment.
The bivariate analyses also indicated variations across different types of insurance. Among participants who sought any treatment in the past year, those with private insurance were less likely to report an unmet need. Also, among individuals with a major depressive episode who did not seek care, those with Medicaid were more likely to report an unmet need than participants with other types of coverage, and those with Medicare or CHAMPUS were less likely to report an unmet need than others.
Differences in quality of treatments have been noted among individuals with different insurance types. For example, in some studies, persons with depression who had public insurance were less likely than those with private insurance to receive psychotherapy or continuous medication treatment ( 49 ). It is notable, however, that differences in insurance type did not persist in the multivariate analyses in the study reported here. Thus many of the differences between these groups may be attributable to differences in the sociodemographic or clinical characteristics of persons with different insurance types.
The third finding of the study was the prominent place of cost concerns as barriers to seeking mental health treatment among participants who reported an unmet need for such treatment. Cost concerns were reported by about half of all participants and were more prominent among participants who had not sought any mental health treatment. A far greater number of participants cited cost as a barrier than any other barrier. This finding is in contrast with results of some research from the 1990s in which attitudinal barriers to mental health treatment seeking were judged to be more prominent than cost barriers or to be on par ( 7 , 8 , 9 ). However, an increase in cost barriers in tandem with increased demand for mental treatments in recent years has been noted ( 13 ). This finding is also consistent with other data on trends in out-of-pocket costs of mental health care in recent years ( 14 ). Furthermore, perceived barriers to treatment seeking may vary according to severity of mental health conditions, and attitudinal factors may play a more prominent role among less severely distressed individuals.
If the trends of the recent past continue in the near future, both the demand for mental health treatments and the cost of such treatments will continue to grow. Barring dramatic expansion of mental health insurance coverage and reduction in out-of-pocket costs, the number of individuals with depression who will experience cost as a barrier to receiving needed treatment will likely continue to grow as well. Reducing the impact of cost barriers and improving the quality of mental health treatments in general medical settings remain important challenges for future efforts to reduce the burden of depression in the community.
Conclusions
This study found that despite the increased prevalence of treatment seeking for major depression in recent years, many individuals with this disabling condition continue to experience an unmet need for treatment. Even among individuals who seek treatment, a large percentage report an unmet need for mental health treatment. Concern about treatment costs is the largest single barrier to seeking needed treatment among these individuals.
Acknowledgments and disclosures
Dr. Mojtabai has received research funding and consultant fees from Bristol-Myers Squibb.
1. Fawcett J: The morbidity and mortality of clinical depression. International Journal of Clinical Psychopharmacology 8:217–220, 1993Google Scholar
2. Goldberg D, Bridges K, Duncan-Jones P, et al: Detecting anxiety and depression in general medical settings. British Medical Journal 297:897–899, 1988Google Scholar
3. Regier DA, Burke JD, Burke KC: Comorbidity of affective and anxiety disorders in the NIMH Epidemiologic Catchment Area program, in Comorbidity of Mood and Anxiety Disorders. Edited by Master JD, Cloninger CR. Washington, DC, American Psychiatric Press, 1990Google Scholar
4. Tiemens BG, Ormel J, Simon GE: Occurrence, recognition, and outcome of psychological disorders in primary care. American Journal of Psychiatry 153:636–644, 1996Google Scholar
5. Wells KB, Burnam MA, Rogers W, et al: The course of depression in adult outpatients: results from the Medical Outcomes Study. Archives of General Psychiatry 49:788–794, 1992Google Scholar
6. Messias E, Eaton W, Nestadt G, et al: Psychiatrists' ascertained treatment needs for mental disorders in a population-based sample. Psychiatric Services 58:373–377, 2007Google Scholar
7. Sareen J, Jagdeo A, Cox BJ, et al: Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric Services 58:357–364, 2007Google Scholar
8. Goldstein RB, Olfson M, Martens EG, et al: Subjective unmet need for mental health services in depressed children grown up. Administration and Policy in Mental Health 33:666–673, 2006Google Scholar
9. Goering P, Lin E, Campbell D, et al: Psychiatric disability in Ontario. Canadian Journal of Psychiatry 41:564–571, 1996Google Scholar
10. Simon GE, Fleck M, Lucas R, et al: Prevalence and predictors of depression treatment in an international primary care study. American Journal of Psychiatry 161:1626–1634, 2004Google Scholar
11. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:203–209, 2002Google Scholar
12. Bristow K, Patten S: Treatment-seeking rates and associated mediating factors among individuals with depression. Canadian Journal of Psychiatry 47:660–665, 2002Google Scholar
13. Mojtabai R: Trends in contacts with mental health professionals and cost barriers to mental health care among adults with significant psychological distress in the United States: 1997–2002. American Journal of Public Health 95:2009–2014, 2005Google Scholar
14. Tu HT: Rising Health Costs, Medical Debt and Chronic Conditions. Issue brief 88. Washington, DC, Center for Studying Health System Change, Sept 2004Google Scholar
15. McDevitt R, Gabel J, Gandolfo L, et al: Financial protection afforded by employer-sponsored health insurance: current plan designs and high-deductible health plans. Medical Care Research and Review 64:212–228, 2007Google Scholar
16. Neuman P, Cubanski J, Desmond KA, et al: How much "skin in the game" do Medicare beneficiaries have? The increasing financial burden of health care spending, 1997–2003. Health Affairs 26:1692–1701, 2007Google Scholar
17. Results From the 2005 National Survey on Drug Use and Health: National Findings. NSDUH series H-30, DHHS pub no SMA-06-4194. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2006Google Scholar
18. Results From the 2006 National Survey on Drug Use and Health: National Findings. NSDUH series H-32, DHHS pub no SMA-07-4293. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2007Google Scholar
19. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
20. Kessler RC, Berglund P, Demler O, et al: The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289:3095–3105, 2003Google Scholar
21. Katz SJ, Kessler RC, Lin E, et al: Medication management of depression in the United States and Ontario. Journal of General Internal Medicine 13:77–85, 1998Google Scholar
22. Wang PS, Lane M, Olfson M, et al: Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry 62:629–640, 2005Google Scholar
23. Sheehan DV, Harnett-Sheehan K, Raj BA: The measurement of disability. International Clinical Psychopharmacology 11 (suppl 3):89–95, 1996Google Scholar
24. Kessler RC, Andrews G, Colpe LJ, et al: Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine 32:959–976, 2002Google Scholar
25. Kessler RC, Barker PR, Colpe LJ, et al: Screening for serious mental illness in the general population. Archives of General Psychiatry 60:184–189, 2003Google Scholar
26. Mojtabai R, Olfson M: Treatment seeking for depression in Canada and the United States. Psychiatric Services 57:631–639, 2006Google Scholar
27. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55–61, 2001Google Scholar
28. Meadows G, Burgess P, Bobevski I, et al: Perceived need for mental health care: influences of diagnosis, demography and disability. Psychological Medicine 32:299–309, 2002Google Scholar
29. Mojtabai R, Olfson M, Mechanic D: Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry 59:77–84, 2002Google Scholar
30. Edlund MJ, Unützer J, Curran GM: Perceived need for alcohol, drug, and mental health treatment. Social Psychiatry and Psychiatric Epidemiology 41:480–487, 2006Google Scholar
31. Kessler RC, Demler O, Frank RG, et al: Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine 352:2515–2523, 2005Google Scholar
32. Jorm AF, Christensen H, Griffiths KM: Changes in depression awareness and attitudes in Australia: the impact of beyondblue: the national depression initiative. Australian and New Zealand Journal of Psychiatry 40:42–46, 2006Google Scholar
33. Mojtabai R: Americans' attitudes toward mental health treatment seeking: 1990–2003. Psychiatric Services 58:642–651, 2007Google Scholar
34. Mojtabai R: Increase in antidepressant medication in the US adult population between 1990 and 2003. Psychotherapy and Psychosomatics 77:83–92, 2008Google Scholar
35. Kerr MP: Antidepressant prescribing: a comparison between general practitioners and psychiatrists. British Journal of General Practice 44:275–276, 1994Google Scholar
36. Croghan TW, Melfi CA, Dobrez DG, et al: Effect of mental health specialty care on antidepressant length of therapy. Medical Care 37(4 suppl Lilly):AS20–AS3, 1999Google Scholar
37. Mojtabai R, Olfson M: National patterns in antidepressant treatment by psychiatrists and general medical providers: results from the National Comorbidity Survey Replication. Journal of Clinical Psychiatry 69:1064–1074, 2008Google Scholar
38. Schraufnagel TJ, Wagner AW, Miranda J, et al: Treating minority patients with depression and anxiety: what does the evidence tell us? General Hospital Psychiatry 28:27–36, 2006Google Scholar
39. Diala C, Muntaner C, Walrath C, et al: Racial differences in attitudes toward professional mental health care and in the use of services. American Journal of Orthopsychiatry 70:455–464, 2000Google Scholar
40. Kilbourne AM, Bauer MS, Han X, et al: Racial differences in the treatment of veterans with bipolar disorder. Psychiatric Services 56:1549–1555, 2005Google Scholar
41. Kuno E, Rothbard AB: The effect of income and race on quality of psychiatric care in community mental health centers. Community Mental Health Journal 41:613–622, 2005Google Scholar
42. Richardson J, Anderson T, Flaherty J, et al: The quality of mental health care for African Americans. Culture, Medicine and Psychiatry 27:487–498, 2003Google Scholar
43. Charbonneau A, Rosen AK, Ash AS, et al: Measuring the quality of depression care in a large integrated health system. Medical Care 41:669–680, 2003Google Scholar
44. Anders RL, Olson T, Bader J: Assessment of acutely mentally ill patients' satisfaction of care: there is a difference among ethnic groups. Issues in Mental Health Nursing 28:297–308, 2007Google Scholar
45. Ngo-Metzger Q, Legedza AT, Phillips RS: Asian Americans' reports of their health care experiences: results of a national survey. Journal of General Internal Medicine 19:111–119, 2004Google Scholar
46. Keeler EB, Wells KB, Manning WG, et al: The Demand for Episodes of Mental Health Services. Santa Monica, Calif, RAND Corp, 1986Google Scholar
47. Sharfstein SS: The role of private insurance in financing treatment for depression. Social Psychiatry and Psychiatric Epidemiology 30:236–239, 1995Google Scholar
48. Harman JS, Hall AG, Zhang J: Changes in health care use and costs after a break in Medicaid coverage among persons with depression. Psychiatric Services 58:49–54, 2007Google Scholar
49. Melfi CA, Croghan TW, Hanna MP: Access to treatment for depression in a Medicaid population. Journal of Health Care for the Poor and Underserved 10:201–215, 1999Google Scholar



