Patterns of Psychiatric Hospitalization Among Ethiopian and Former Soviet Union Immigrants and Persons Born in Israel
Immigration has been repeatedly shown to be a risk factor for mental disorders and psychological distress ( 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 ). This seems to hold true even when conditions of immigration are particularly favorable, as they are in Israel. Immigration to Israel is viewed as a return to the homeland, and upon their arrival to Israel, immigrants become citizens and are entitled to a broad range of support from the government ( 2 , 13 , 14 ).
Despite higher rates of emotional distress among immigrants than among nonimmigrants, there is no evidence that immigrant populations have a higher use of mental health services ( 15 , 16 ). This situation may be especially acute for immigrants from non-Western countries, such as African countries, who are unfamiliar with mental health services in host societies ( 17 ). Also, there are differences in the pattern of mental health service use between immigrants and those who are native born, especially regarding hospitalization. For example, in a study of persons who emigrated from the Caribbean Islands to London, Takei and colleagues ( 18 ) showed that compared with the native-born population, immigrants tended to be hospitalized for longer periods and the hospitalizations were more likely to be involuntary.
Understanding these variations in service use among immigrants might be facilitated by comparing immigrant populations that have cultural differences ( 6 , 19 , 20 ). In Israel there is a unique opportunity for such a comparison. One advantage is the existence of a cumulative national register of psychiatric hospitalizations ( 21 ). In addition, Israel is a country of immigrants who come from countries with vast cultural differences. Between 1984 and 1995, Israel absorbed 803,000 immigrants ( 22 ), most of them from the Former Soviet Union (FSU) and Ethiopia. The mass immigration from the FSU began in 1989, and between 1990 and 1995, more than half a million immigrants arrived in Israel from the FSU ( 22 ). The Ethiopian wave of immigrants was much smaller: the current estimate of the number of Ethiopian Jews in Israel is about 105,500, including those who were born in Israel ( 23 ). Most of the Ethiopian Jews arrived in Israel in two dramatic waves: Operation Moses included about 7,400 adults and children who arrived between mid-November 1984 and April 1985; Operation Solomon included over 14,000 people who arrived from Addis Ababa on May 24–25, 1991 ( 24 ). It is important to mention that the two groups came under very different circumstances: the Jewish Ethiopians who came with Operation Moses in the 1980s fled from Ethiopia to Sudan and waited for a long period to be rescued from refugee camps there. In contrast, the Operation Solomon group was airlifted to Israel directly from Addis Ababa. The rest of the Ethiopian Jews arrived individually or in small groups, according to the policy of the Israeli government. A final advantage is that, in the case of immigration from both Ethiopia and the FSU, it was a mass immigration, and thus the self-selection factors played a less significant role than they would in most other studies.
The aim of the study was to explore the frequency and pattern of psychiatric hospitalization of two immigrant groups in Israel—immigrants from the FSU and immigrants from Ethiopia—that have different cultural backgrounds. Most of the latter group are at a low level of acculturation and belong to the lowest socioeconomic class ( 24 ). This study sought to disentangle the effect of immigration from that of cultural differences. Comparison of the frequency and pattern of psychiatric hospitalization among immigrants from Ethiopia and the FSU allowed for the estimation of the effect of cultural differences, while the effect of immigration itself was studied by a comparison of persons born in Israel and immigrants from the FSU.
Methods
Study population
The study analyzed six population groups—three groups of new immigrants and two Israel-born Jewish groups (which served as comparisons) plus one of the immigrant groups ten years after immigration. The three groups of new immigrants were Operation Moses 1980s immigrants (from Ethiopia between January 1, 1980, and August 31, 1985), Operation Solomon 1990s immigrants (from Ethiopia in 1990 and 1991), and FSU 1990s immigrants (from the FSU in 1990 and 1991). The two Israel-born Jewish groups were those with at least one psychiatric hospitalization between January 1, 1980, and August 31, 1985 (Israel born 1980s) and those with at least one such hospitalization between 1990 and 1994 (Israel born 1980s). The Operation Moses immigrant group that was followed up ten years later is labeled Operation Moses immigrants in the 1990s.
The study involved immigrants with at least one psychiatric hospitalization during the five years after immigration for Operation Moses 1980s immigrants, Operation Solomon 1990s immigrants, and FSU 1990s immigrants and immigrants with at least one psychiatric hospitalization during the ten to 14 years after their immigration for Operation Moses immigrants in the 1990s. Only hospitalizations for persons aged 18 or older were considered.
For each person, the first hospitalization in the years of the study is called the key hospitalization. It occurred in the 1990s for four groups and in the 1980s for two groups. The study of the patterns of psychiatric hospitalization was based on an individual follow-up of four years from the date of the key hospitalization admission.
Data collection
The total population in each of the groups was obtained from the Israel Central Bureau of Statistics. Unidentified demographic and clinical data on psychiatric hospitalizations were extracted from the Israel Psychiatric Case Register, which contains cumulative data on psychiatric hospitalizations reported by all 36 psychiatric inpatient units throughout the country since 1950.
Outcome measures
The outcome measures were incidence rates of psychiatric hospitalization and pattern of psychiatric hospitalization—that is, length of the key hospitalization, time between discharge from the key hospitalization and rehospitalization (time until rehospitalization), cumulative length of stay in the hospital during follow-up, and diagnosis upon discharge from the key hospitalization.
Statistical analysis
When we compared the annual incidence rates of psychiatric hospitalization in the six different population groups, we calculated age-specific rates (because the rates are age-dependent and the age distribution is different in the different groups) and, as a summary measure, age- and gender-adjusted rates. Because each population group has people who immigrated to Israel, died, or left Israel in the period during which we looked for key hospitalizations, the denominator for calculating rates in each population group was the number of person-years in the given period. For instance, for Operation Moses 1980s immigrants, we calculated the number of person-years of the immigrants from Ethiopia who immigrated between January 1, 1980, and August 31, 1985, aged 18 and older during the five years after date of immigration. In each population group, the data by age and sex were obtained from the Central Bureau of Statistics. We made direct adjustment—that is, the adjusted rates were based on the actual age-specific rates within each group applied to the same standard population—in our case, the Israel-born Jewish population on January 1, 1990.
Because the psychiatric diagnoses might not be reliable, they were grouped into four broad diagnostic categories according to the ICD-10 ( 25 ): schizophrenia or other psychoses, including schizophrenic disorders, paranoid states, and other nonorganic psychoses; affective disorders, including manic episodes, bipolar affective disorders, depressive episodes, recurrent depressive disorders, persistent mood disorders, other mood disorders, and unspecified mood disorders; neurotic or personality disorders, including anxiety disorders, obsessive-compulsive disorder, reaction to severe stress and adjustment disorders, dissociative disorders, somatoform disorders and other neurotic disorders, physiological malfunction arising from mental factors, acute reaction to stress, posttraumatic stress disorder, adjustment reaction and depressive disorder not elsewhere classified, personality disorders, sexual deviations and disorders, alcohol dependence syndrome, drug dependence, nondependent abuse of drugs, and disturbance of conduct not elsewhere classified; and Z codes, a "diagnosis" that is given mainly to persons hospitalized for evaluation and examination.
Because the distribution of the length of hospitalization was not close to a normal distribution, the length of hospitalization was measured by a survival analysis (Kaplan-Meier method). The same method was used for time until rehospitalization and cumulative length of stay in the hospital during follow-up. The significance of the difference between the different population groups concerning the distribution of each of these three variables was evaluated with a logrank test. Comparison of the six population groups regarding these three variables was also done after controlling for age, sex, diagnosis, and legal status of the psychiatric hospitalization (Cox regression analysis). The analysis was done with SPSS, version 15.
Results
A total of 178 Operation Moses 1980s immigrants had a psychiatric hospitalization, as did 194 Operation Moses immigrants in the 1990s, 184 Operation Solomon 1990s immigrants, 2,082 FSU 1990s immigrants, 10,120 Israel born 1980s, and 11,241 Israel born 1990s.
When we compared the annual incidence rate of psychiatric hospitalization in the six population groups, we found that the rates were significantly higher among Ethiopian Jews during the five years after immigration than they were among immigrants from the FSU or among those in the Israel-born group—Operation Moses 1980s immigrants versus Israel born 1980s, p<.001; Operation Solomon 1990s immigrants versus FSU 1990s immigrants, p<.001; and Operation Solomon 1990s immigrants versus Israel born 1990s, p<.001. Compared with the other five groups, Operation Moses 1980s immigrants had the highest annual incidence rate of psychiatric hospitalization ( Table 1 ). However, the rate in this population group ten years after immigration (Operation Moses immigrants in the 1990s) became similar to the rate among the Israel born 1990s. A decrease in the hospitalization rate was observed in the Israel-born group between the 1980s and the 1990s, but the decrease was much smaller (21.2%) than that found among Ethiopians during the same period (47.3%).
 |
In order to further explore the effects of immigration and cultural differences on psychiatric hospitalization, we compared the pattern of psychiatric hospitalization in the four years after the key hospitalization in the six population groups ( Table 2 ). In the Israel-born groups, the length of hospitalization was significantly shorter (p<.001) in the 1990s than it was in the 1980s. This corresponds to the general policy of decreasing the duration of hospitalization. However, the length of hospitalization among Operation Moses immigrants was similar in the 1990s and in the 1980s, which, in view of the trend described above in the Israel-born groups, indicates a relative increase in length of hospitalization. In the 1990s the length of hospitalization in the Israel-born group was similar to that of the Operation Solomon immigrants and significantly shorter than that of the Operation Moses immigrants (p=.004) and immigrants from the FSU (p<.001). No significant difference was found between immigrants from the FSU and Operation Moses immigrants in the 1990s.
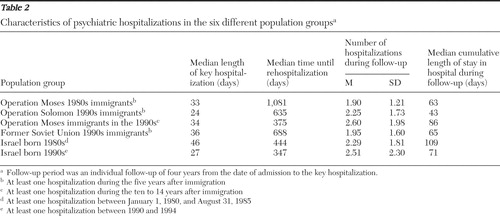 |
We also calculated the time until rehospitalization in the different population groups ( Table 2 ). We found that Operation Moses 1980s immigrants had a significantly longer time until rehospitalization than the Israel born 1980s (median of 1,081 versus 444 days) (p<.001). However, in the 1990s there was no significant difference between Operation Moses immigrants in the 1990s and the Israel born 1990s (median of 375 versus 347 days). The Operation Solomon 1990s immigrants had a significantly longer time until rehospitalization compared with the Israel born 1990s (median of 635 versus 347 days) (p=.020). FSU immigrants had a significantly longer time until rehospitalization than the other groups in the same years—versus Operation Solomon immigrants in the 1990s, p=.018; and versus Israel born 1990s, p<.001. We also calculated the mean number of hospitalizations during the follow-up period ( Table 2 ). The longer the time until rehospitalization, the smaller the number of hospitalizations. The results were similar for both analyses (time until rehospitalization and number of hospitalizations).
We also examined the cumulative length of stay in a hospital during the four years of follow-up ( Table 2 ). Because of the decrease in length and number of hospitalizations in Israel between the 1980s and the 1990s, the cumulative length of stay for the Israel-born group was significantly shorter (p<.001) in the 1990s than it was in the 1980s. In contrast, the cumulative length of stay for Operation Moses immigrants was significantly longer (p=.010) in the 1990s than in the 1980s. In the 1990s, the immigrants from Ethiopia (Operation Solomon 1990s immigrants) had a significantly shorter cumulative length of stay than the other groups.
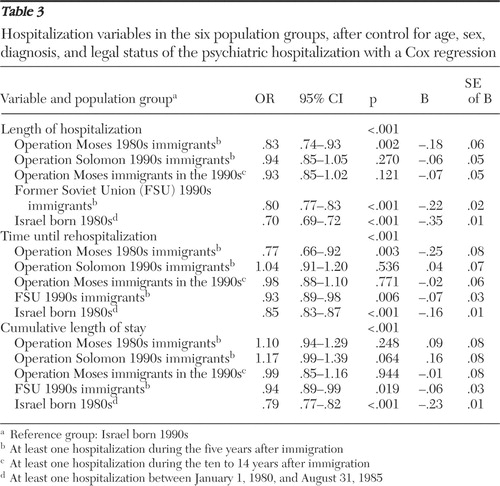
Preliminary analyses showed that length of the key hospitalization, time until rehospitalization, and cumulative length of stay during follow-up were associated with demographic and clinical factors, such as age, sex, diagnosis, and legal status of the psychiatric hospitalization, and there were differences in the distribution of these variables in the six different population groups. We therefore compared the three dependent variables in these population groups after controlling for these variables (Cox regression). As shown in Table 3 , the results were similar to those of the analyses that did not control for these variables.
 |
We then compared the distribution of the patients in the different groups by diagnosis given upon discharge from the key hospitalization ( Table 4 ). In the three population groups of recent immigrants, 45%–47% were diagnosed as having schizophrenia or other psychotic disorder. However, among the Operation Moses immigrants in the 1990s, whose key hospitalization occurred ten to 15 years after immigration, the percentage was 72%, which was significantly higher than in all other population groups.
 |
However, when we looked at only the first psychiatric hospitalization in Israel for Operation Moses immigrants in the 1990s (that is, Operation Moses immigrants in the 1990s who did not have a hospitalization in the 1980s), the percentage of patients with schizophrenia or other psychosis was only slightly higher among the Operation Moses immigrants in the 1990s than in the other groups (54% versus approximately 45% in the other groups). In this analysis, the differences between the population groups were not statistically significant.
The key hospitalization for the groups that recently immigrated is also the first hospitalization in Israel (except for the few cases with a previous hospitalization in Israel under the age of 18 years). For these groups, the key hospitalization was considered to be the first lifetime hospitalization because data were not available about what happened before immigration. To examine diagnoses after the first lifetime hospitalization, we gathered data for all hospitalizations in the follow-up period. The percentage of patients in this group with schizophrenia or other psychosis upon discharge from a rehospitalization was 83% among Operation Moses immigrants in the 1990s, compared with 64% for Operation Moses 1980s immigrants, 61% for Operation Solomon 1990s immigrants, 59% for FSU 1990s immigrants, 71% for the Israel born 1980s, and 73% for the Israel born 1990s.
Table 4 also shows that the proportion of patients with a diagnosis of neurosis or personality disorder was highest among Operation Moses 1980s immigrants, and lowest in the same population ten years later (Operation Moses immigrants in the 1990s). Another salient finding is the very high prevalence of the Z codes among both Operation Moses 1980s immigrants and Operation Solomon 1990s immigrants.
Discussion
Significant differences in rates and patterns of psychiatric hospitalization in Israel were found between Ethiopian immigrants, FSU immigrants, and people born in Israel. The strength of the study resides in the fact that a mass immigration (reducing the role of self-selection factors) of two very different populations took place in Israel, that Israel has a cumulative national registry of psychiatric hospitalizations, and that denominator data are available on population groups by place of birth, age, and period of immigration.
A weakness of the study is that the prevalence rate of psychopathology in the different population groups was unknown and therefore could not be taken into account when comparing hospitalization rates. Also, although psychiatric diagnoses were recorded, their severity was not, nor was the type of care.
New immigrants—Operation Moses 1980s immigrants, Operation Solomon 1990s immigrants, and FSU 1990s immigrants—went through the trauma of leaving their former society and adapting to the new society by, for example, learning Hebrew and familiarizing themselves with this society, in particular with the Western-style Israeli mental health system. Ethiopian immigrants faced additional challenges. In this group there was a marked cultural contrast with the host society, in particular with a specific medical belief system, typical health behavior, and symptom presentation ( 14 , 26 , 27 , 28 , 29 , 30 ), all unknown to Israeli health and mental health providers. There was also a high level of illiteracy among Ethiopian immigrants. This group had generally no knowledge of any language other than Amharic, which is not spoken by health care providers. Finally, at the beginning of the Ethiopian immigration to Israel (in the 1980s), there were hardly any social support networks available within the Ethiopian community structure that could help its most vulnerable members. However, social support networks developed as the Ethiopian community slowly became more organized ( 24 ).
In contrast to the Ethiopian immigrants, the FSU immigrants were highly educated and were more familiar with the Western mental health system and mode of life. Also, because persons had been immigrating to Israel from the FSU since the 1970s, by the 1990s Israel had a large FSU community and a relatively strong social support network that FSU immigrants could take advantage of ( 2 ). In addition, FSU immigrants had many physicians and mental health professionals among them ( 31 ). Thus a comparison of FSU immigrants with those born in Israel indicates the effect of immigration itself, whereas a comparison of FSU immigrants with Ethiopian immigrants indicates the effect of socioeconomic and cultural differences on rate and pattern of psychiatric hospitalization.
Immigrants have been found to have higher rates of psychopathology than the native population ( 20 , 32 ). In Israel, increased psychopathology rates were found among immigrants from both Ethiopia and the FSU ( 2 , 14 , 26 , 33 ). Even though the rate of hospitalization is related to other factors besides psychopathology, one might nevertheless have expected a higher hospitalization rate among FSU immigrants than among the Israel born 1990s. However, our study found that in the 1990s FSU immigrants did not have a higher hospitalization rate than native-born persons. One reason may be that immigration increases psychological distress ( 2 ), which can be taken care of in the community, rather than increasing severe psychiatric diagnoses, which would lead to psychiatric hospitalization. Our finding that the hospitalization rate and the number of hospitalizations during follow-up in the 1990s were even lower for FSU immigrants than for the Israel born could be due to the stigma of psychiatric hospitalization in a population from a country where it served as a political weapon ( 13 , 34 ). Hence, only severe cases would be hospitalized, explaining why in the 1990s FSU immigrants had a longer key hospitalization than the Israel born.
FSU immigrants also had a higher percentage of affective disorders than the other population groups, which is consistent with their high level of psychological distress ( 2 ). The fact that the percentage of affective disorders was lower among Ethiopian immigrants than among FSU immigrants may be due to the difference in age between the two population groups (the Ethiopian immigrant population was relatively young compared with FSU 1990s immigrants); immigration has been shown to contribute to an increase in depression, especially among elderly persons ( 35 ).
Thus immigration appeared to have minimal influence on psychiatric hospitalization when immigrants had sociodemographic and cultural characteristics similar to those of the native born. However, compared with FSU 1990s immigrants, Operation Solomon 1990s immigrants had a psychiatric hospitalization rate that was twice as high. Also, compared with FSU 1990s immigrants, Operation Solomon 1990s immigrants had a shorter key hospitalization, a larger number of hospitalizations during follow-up, and a shorter cumulative length of hospitalization during follow-up. Sociodemographic and cultural factors thus seem to play a major role in psychiatric hospitalization.
Looking at the first wave of immigration to Israel—Operation Moses immigrants in the 1980s—strengthens this interpretation. They were found to be very different from all other groups. In particular this group had the highest rate of psychiatric hospitalization. One has to keep in mind policy changes regarding psychiatric hospitalization in Israel between the 1980s and the 1990s, which served to reduce the hospitalization rate and the median length of hospitalization ( 36 ). This is reflected in our comparison of the Israel-born population in the 1980s and the 1990s. However, the reduction in psychiatric hospitalization rates between the 1980s and the 1990s was much larger among Operation Moses immigrants than among the Israel born, which indicates a specific change among the Ethiopians beyond the policy changes.
In the 1980s these immigrants from Ethiopia were not aware of the different treatment possibilities. The lack of familiarity with the Western-style Israeli mental health system, along with the inability to speak Hebrew or English, could have led to a delay in seeking treatment in psychiatric clinics and thus resulted in higher rates of psychiatric hospitalization.
Lam and Kavanagh ( 37 ) also found that Indochinese immigrants who were psychiatric patients in Sydney, Australia, had taken longer to receive psychiatric treatment from health professionals for their first episode and tended to receive initial help from family members or traditional healers. Fenta and colleagues ( 17 ) found that in Toronto only a small proportion of Ethiopian immigrants with mental disorders were treated by health care professionals, mostly family physicians, and that the Ethiopians were more likely to consult traditional healers than health care professionals for mental health problems. Moreover, the Toronto researchers also found that although the presence of somatic symptoms was significantly associated with an increased use of health care services, having a mental disorder was associated with a lower rate of health service use ( 38 ).
In addition, Operation Moses 1980s immigrants had highly traumatic experiences during their passage through Sudan ( 39 ), and mental health professionals in Israel had not yet had a chance to understand their culture and their presentation of symptoms ( 29 , 30 ). Also, Operation Moses immigrants lost their social support network and did not yet have any in Israel. All this may have contributed to a higher prevalence rate of psychopathology (mainly anxiety disorders and posttraumatic stress disorders) and overhospitalization (as indicated by hospitalization of people with less severe diagnoses, shorter stays in hospital, and less recurrent hospitalizations) among the Operation Moses 1980s immigrants, compared with the Israel born in the same years (1980s). This might mean that among these Ethiopian immigrants, psychiatric hospitalizations were not based on pure pathology but also on sociocultural factors.
Ten years later, the rate of hospitalization for these immigrants (Operation Moses immigrants in the 1990s) was similar to that of the Israel-born population in the same years. However, compared with the Israel born 1990s, Operation Moses immigrants in the 1990s had a higher proportion of diagnoses of schizophrenia or other psychosis and longer hospitalizations. The prevalence of psychosis was the highest for the rehospitalizations of Operation Moses immigrants in the 1990s. Among Operation Moses immigrants in the 1990s, the hospitalization rate was low, but those with schizophrenia had the highest likelihood of being rehospitalized, probably because of a lack of an adequate support system among the Ethiopian families and the inability of the Ethiopian community as a whole to deal with severe cases of schizophrenia or other psychotic disorders. Their rate of hospitalization was significantly lower than that of the Ethiopians who immigrated in the 1990s. Thus a large change concerning Operation Moses 1980s immigrants occurred during the ten years after their immigration.
Through the years, mental health professionals made apparent progress in the diagnosis and treatment of Ethiopian patients. Between the 1980s and the 1990s, Operation Moses immigrants had learned some Hebrew, learned about the available services, and developed support networks. This might explain the reduction in hospitalization rates among Operation Moses immigrants between the 1980s and the 1990s; for Operation Moses immigrants in the 1990s, the rates and pattern of hospitalization became similar to those of Israel-born 1990s.
The more recent Ethiopian wave, Operation Solomon 1990s immigrants, had hospitalization characteristics (rate and pattern) that fell between those of Operation Moses 1980s immigrants and Operation Moses immigrants in the 1990s. Unlike immigrants from Operation Moses 1980s, Operation Solomon 1990s immigrants benefited from the improved expertise of mental health professionals and from an existing support network. However, Operation Solomon 1990s immigrants recently had undergone the trauma of immigration and tended to not know Hebrew and to feel alienated.
Another finding is the very high prevalence of Z codes among both Operation Moses 1980s immigrants and Operation Solomon 1990s immigrants, which probably reflects psychiatrists' difficulties in understanding the pathology of the newly arrived Ethiopian immigrants and their decision to refer these patients to the hospital for further examination and observation.
Conclusions
The new immigrants from Ethiopia and the FSU were shown to have very different rates and patterns of psychiatric hospitalization. They share a common risk factor, immigration, but the sociocultural differences between FSU immigrants and the Israel born are not as large as for immigrants from Ethiopia. A reasonable conclusion is that sociocultural differences and understanding of these differences by mental health professionals may have a more crucial influence upon rates and patterns of psychiatric hospitalization than the immigrant experience itself.
Acknowledgments and disclosures
This research was supported by a grant from the Institute of Immigration and Social Integration, Ruppin Academic Center, Emek Heffer, Israel. The authors are grateful to their colleagues, Yaacov Lerner, M.D., and Marjorie Chary Feinson, Ph.D., for their illuminating contributions.
The authors report no competing interests.
1. Odegaard O: Emigration and insanity: a study of mental disease among the Norwegian-born population of Minnesota. Acta Psychiatrica Scandinavica 7(suppl 4):1–206, 1932Google Scholar
2. Zilber N, Lerner Y: Psychological distress among recent immigrants from the former Soviet Union to Israel: I. correlates of level of distress. Psychological Medicine 26:493–501, 1996Google Scholar
3. Hjern A, Wicks S, Dalman C: Social adversity contributes to high morbidity in psychoses in immigrants: a national cohort study in two generations of Swedish residents. Psychological Medicine 34:1–9, 2004Google Scholar
4. Lay B, Lauber C, Nordt C, et al: Patterns of inpatient care for immigrants in Switzerland. Social Psychiatry and Psychiatric Epidemiology 41:199–207, 2006Google Scholar
5. Bhugra D: Migration and schizophrenia. Acta Psychiatrica Scandinavica: Supplementum 407:68–73, 2000Google Scholar
6. Cantor-Graae E, Zolokowska K, McNeil TF: Increased risk of psychotic disorder among immigrants in Malmo: a 3-years first-contact study. Psychological Medicine 35:1155–1163, 2005Google Scholar
7. Leao TS, Sundquist J, Frank G, et al: Incidence of schizophrenia or other psychoses in first- and second-generation immigrants: a national cohort study. Journal of Nervous and Mental Disease 194:27–33, 2006Google Scholar
8. Orely J: Psychological distress among refugees: some clinical and epidemiological considerations; in Amidst Peril and Pain: The Mental Health and Well-Being of the World's Refugees. Edited by Mersella AJ, Bornemann T, Ekblad S, et al. Washington, DC, American Psychological Association, 1994Google Scholar
9. Carta MG, Kovess V, Hardoy MC, et al: Psychiatric disorders in Sardinian immigrants to Paris: a comparison with Parisians and Sardinians resident in Sardinia. Social Psychiatry and Psychiatric Epidemiology 37:112–117, 2002Google Scholar
10. Ortega AN, Rosenberg R, Alegria M, et al: Acculturation and the lifetime risk of psychiatric and substance use disorders among Hispanics. Journal of Nervous and Mental Disease 188:728–735, 2000Google Scholar
11. Bhugra D: Migration and depression. Acta Psychiatrica Scandinavica 108:67–72, 2003Google Scholar
12. Ward C, Bochner S, Furnham A: The Psychology of Culture Shock. London, United Kingdom, Routledge, 2001Google Scholar
13. Levav I, Kohn R, Flaherty JA, et al: Mental health attitudes and practices of Soviet immigrants. Israel Journal of Psychiatry and Related Sciences 27(3):131–144, 1990Google Scholar
14. Arieli A, Aychen S: Psychopathology among Jewish Ethiopian immigrants in Israel. Journal of Nervous and Mental Disease 180:465–466, 1992Google Scholar
15. Steel Z, Silove D, Chey T, Bauman A, et al: Mental disorders, disability and health service use amongst Vietnamese refugees and the host Australian population. Acta Psychiatrica Scandinavica 111:300–309, 2005Google Scholar
16. Jackson JS, Neighbors HW, Torres M, et al: Use of mental health services and subjective satisfaction with treatment among Black Caribbean immigrants: results from the National Survey of American Life. American Journal of Public Health 97:60–67, 2007Google Scholar
17. Fenta H, Hyman I, Noh S: Mental health service utilization by Ethiopian immigrants and refugees in Toronto. Journal of Nervous and Mental Disease 194:925–934, 2006Google Scholar
18. Takei N, Persaud R, Woodruff P, et al: First episodes of psychosis in Afro-Caribbean and White people: an 18-year follow-up population-based study. British Journal of Psychiatry 172:147–153, 1998Google Scholar
19. Takeuchi DT, Uehara E, Maramba G: Cultural diversity and mental health treatment; in A Handbook for the Study of Mental Health. Edited by Horowitz AV, Scheild TL. Cambridge, United Kingdom, Cambridge University Press, 1999Google Scholar
20. Kinzie JD: Immigrants and refugees: the psychiatric perspective. Transcultural Psychiatry 43:577–591, 2006Google Scholar
21. Lichtenberg P, Kaplan Z, Grinshpoon A, et al: The goals and limitations of Israel's psychiatric case register. Psychiatric Services 50:1043–1048, 1999Google Scholar
22. Statistical Abstract of Israel. No 47. Central Bureau of Statistics. Tel Aviv, Government Publishing House, 1996Google Scholar
23. Statistical Abstract of Israel. No 56. Central Bureau of Statistics. Tel Aviv, Government Publishing House, 2005Google Scholar
24. Kaplan S: Salomon H: Ethiopian Jews in Israel: a part of the people or apart from people? in Jews in Israel: Contemporary Social and Cultural Patterns. Edited by Rebhun V, Waxman CI. Hanover and London, United Kingdom, Brandeis University Press, 2004Google Scholar
25. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva, World Health Organization, 1992Google Scholar
26. Grisaro N, Irwin M, Kaplan Z: Acute psychotic episodes as a reaction to severe trauma in population of Ethiopian immigrants to Israel. Stress and Health 19:241–247, 2003Google Scholar
27. Andermann LF: Ethiopian Jews meet Israeli family physicians: a study of cultural somatization. Transcultural Psychiatry Research Review 33:333–345, 1996Google Scholar
28. Hodes RM: Cross-cultural medicine and misunderstanding: the case of Ethiopians. Western Journal of Medicine 166:29–36, 1997Google Scholar
29. Reiff M, Zakut H, Weingarten MA: Illness and treatment perceptions of Ethiopian immigrants and their doctors in Israel. American Journal of Public Health 89:1814–1818, 1999Google Scholar
30. Youngmann R, Minuchin-Itzigsohn S, Barasch M: Manifestation of emotional distress among Ethiopian immigrants in Israel: patient and clinician perspective. Transcultural Psychiatry 36:45–63, 1999Google Scholar
31. Flaherty JA, Kohan R, Levav I, et al: Demoralization in Soviet-Jewish immigrants to the United States and Israel. Comprehensive Psychiatry 29:588–597, 1988Google Scholar
32. Kirmayer LJ, Weinfeld M, Burgos G, et al: Use of health care services for psychological distress by immigrants in an urban multicultural milieu. Canadian Journal of Psychiatry 52:295–304, 2007Google Scholar
33. Ponizovsky A, Ginath Y, Durst R, et al: Psychological distress among Ethiopian and Russian Jewish immigrants to Israel: a cross-cultural study. International Journal of Social Psychiatry 44:35–45, 1998Google Scholar
34. Lerner Y, Mirsky J, Barasch M: New beginnings in an old land: refugee and immigrant mental health in Israel; in Amidst Peril and Pain: The Mental Health and Well-Being of the World's Refugees. Edited by Mersella AJ, Bornemann T, Ekblad S, et al. Washington, DC, American Psychological Association, 1994Google Scholar
35. Zilber N, Lerner Y, Eidelman R, et al: Depression and anxiety disorders among Jews from former Soviet Union five years after their immigration to Israel. International Journal of Geriatric Psychiatry 16:993–999, 2001Google Scholar
36. Shani M: The Israel reform of psychiatric hospitalization. Israel Medical Association Journal 7: 818–819, 2005Google Scholar
37. Lam AP, Kavanagh DJ: Help seeking by immigrant Indochinese psychiatric patients in Sydney, Australia. Psychiatric Services 47:993–995, 1996Google Scholar
38. Fenta H, Hyman I, Noh S: Health service utilization by Ethiopian immigrants and refugees in Toronto. Journal of Immigrant and Minority Health 9:349–357, 2007Google Scholar
39. Parfitt T: Operation Moses: The Untold Story of the Exodus of the Falasha Jews From Ethiopia. London, United Kingdom, Weidenfeld and Nicolson, 1985Google Scholar



