Community Integration and Associated Factors Among Older Adults With Schizophrenia
Although 85% of older adults with schizophrenia reside in the community ( 1 ), little is known about community integration in this population. In this study, we examined community integration and related factors among adults aged 55 and over with schizophrenia.
Recently, community integration has gained greater attention because of its relationship to recovery. Although there are numerous definitions of recovery ( 2 ), Bond and colleagues ( 3 ) regard community integration as epitomizing the aspirations of the consumer movement, and as such, it constitutes one of the two core elements of recovery, process and outcome. Process views recovery as an individual's pursuit of personal goals, self-efficacy, self-determination, and community life, but not necessarily the absence of symptoms ( 2 , 3 ). This perspective does not easily lend itself to empirical measurement, whereas outcome entails concrete, measurable, external manifestations such as social ties or employment. Community integration can be conceptualized as the outcome component of the recovery experience, and consequently, it can be operationalized and empirically assessed. There is evidence that community integration facilitates the process aspects of recovery ( 3 ), and the empirical measures of community integration can assist patients in realizing their goals and identify societal barriers to integration.
Community integration examines the extent to which people live, participate, and socialize in their community ( 4 , 5 ). Several researchers ( 5 , 6 ) have conceptualized community integration as comprising three dimensions: physical integration (for example, the extent of engagement and use of community resources), social integration (for example, the quantity and quality of social relationships), and psychological integration (such as the perceived sense of community belonging). With a homeless sample (mean age 41), of whom 42% had a history of psychosis, Gulcur and associates ( 4 ) operationalized this concept, using ten variables. They confirmed the legitimacy of the three dimensions and added one dimension related to independence and self-actualization.
Although older adults are the fastest growing segment of the schizophrenia population ( 7 ), only one study has examined community integration in this age group ( 8 ). That study focused on Dutch elders with mental illness in community residences and hospitals. A broader examination of community integration of older adults will require modification of the parameters used in studies of younger populations because the former are likely to be unemployed and less physically robust. Furthermore, studies will need to compare them with their age peers in the general population in order to establish reasonable expectations about community integration. In the only extant comparative analysis, Aubry and Myner ( 6 ) found that in contrast to a community sample, persons with psychiatric disabilities living in congregate housing (mean ages not given) had lower levels of social integration but similar levels of psychological and physical integrations.
Previous studies of a broad age range of individuals with schizophrenia found associations between community integration and various personal and environmental variables, such as younger age ( 9 , 10 , 11 ), being white ( 10 ), higher daily functioning ( 9 ), lower levels of psychopathology ( 11 , 12 ), greater financial well-being ( 11 , 13 ), greater independence and control ( 9 ), greater availability of services ( 9 , 13 ), and being in environments where psychiatric illness is dispersed rather than concentrated ( 8 , 9 ). However, a limitation of earlier studies is that their analyses were not situated within any theoretical frameworks. Theoretical models are valuable because they allow for the generalizability of results and provide a rationale for the inclusion of predictor variables associated with community integration. Wong and Solomon ( 5 ) have proposed using Moos' ecosystem model ( 14 ) to explore factors associated with community integration. The model theorizes that community integration is affected by personal determinants such as sociodemographic characteristics, psychiatric symptoms, health, and functioning as well as by environmental determinants, especially various features of the consumer's treatment and housing programs. In this study we used a modified version of this model with a focus on the personal components, and where data were available, we included environmental factors.
We tested Wong and Solomon's ( 5 ) hypothesis that the ecosystem model can explain a significant percentage of the variance in community integration and that it identifies personal and environmental factors that are associated with community integration of older adults with schizophrenia. A secondary aim was to test the hypothesis that older adults with schizophrenia have significantly lower levels of community integration compared with their age peers in the general community.
Methods
Details of the study methods and the rationale for the age criteria are provided elsewhere ( 7 , 15 ). Briefly, we recruited participants aged 55 and over living in the community with early-onset schizophrenia (onset before age 45). We used a stratified sampling method in which we attempted to interview approximately half the participants from outpatient clinics and day treatment programs and the other half from supported community residences. Inclusion was based on a DSM-IV diagnosis of schizophrenia or schizoaffective disorder that was assessed by clinical agency staff and on a lifetime illness review adapted from Jeste and associates ( 16 ). We excluded persons with cognitive impairment too severe to complete the questionnaire—that is, scores <5 on the Mental Status Questionnaire ( 17 ).
We recruited a community comparison group using Wessex Census Summary Tape Files 3 for Kings County, New York. We used randomly selected block groups as the primary sampling unit. An effort was made to interview all persons aged 55 and over in a selected block group by knocking on doors. In order to enhance response rates, participants from the selected block group were also recruited at senior centers and churches and through personal references. We excluded persons with histories of treatment for schizophrenia or schizoaffective disorder.
The rejection rate was 15 (7%) in the schizophrenia group and 190 (48%) of those contacted in the community group. The study was approved by an institutional review board, and we obtained written informed consent from all participants. The schizophrenia group consisted of 198 persons with schizophrenia. Among these, 77 (39%) were living independently in the community, and 121 (61%) were in supported community residences. From the original community comparison group of 206, we selected 113 persons who more closely matched the schizophrenia group for age, gender, race and ethnicity, and income. There were no significant gender differences or racial-ethnic differences between groups. Ninety-seven (49%) of the schizophrenia group were women compared with 55 (49%) of the community comparison group. The racial-ethnic distribution in the schizophrenia group was 68 (34%) African Americans, 112 (57%) Caucasians, 14 (7%) Latinos, and four (2%) of other race or ethnicity compared with 41 (36%) African Americans, 68 (60%) Caucasians, two (2%) Latinos, and two (2%) of other race or ethnicity in the community comparison group. The mean±SD ages of the schizophrenia group and community comparison group were 61.5±5.6 and 63.0±5.5 years (t=2.37, df=306, p=.02), respectively. Thus, even though the absolute difference in age between the two groups was small, it attained statistical significance. Both groups were in the same median income category ($7,000–$12,999).
Measures
We used an adaptation of Moos' ecosystem model ( 14 ) as the scaffolding upon which to include variables that were identified previously as being related to community integration or having theoretical relevance. We identified 15 predictor variables, of which 11 were personal variables (five sociodemographic and six psychosocial variables) and four were environmental variables. The following instruments were used to derive the predictor variables and the dependent variable, which was our "community integration scale": Center for Epidemiological Studies Depression Scale (CES-D) ( 18 ), Positive and Negative Syndrome Scale (PANSS) ( 19 ), Dementia Rating Scale ( 20 ) (higher scores indicate better functioning), a summed total of physical illnesses ( 21 ), Instrumental Activities of Daily Living Scale ( 21 ), Abnormal Involuntary Movement Scale (AIMS) ( 22 ), Rosenberg Self-Esteem Scale ( 23 ), Quality of Life Index ( 15 ), CAGE alcoholism screen ( 24 ), and the Network Analysis Profile ( 25 ). All scales had internal reliability (Cronbach's alpha) scores >.77. Reliability >.60 is considered acceptable according to Nunally's criteria ( 26 ). The intraclass correlations of the raters ranged from .79 to .99 on the various scales.
In creating the dependent variable (the community integration scale), we adapted the conceptual model of Wong and Solomon ( 5 ) and its operationalization by Gulcur and associates ( 4 ). We factor analyzed 12 variables using principal-components analysis with equimax rotation. It yielded four components that corresponded to Gulcur and colleagues' ( 4 ) four dimensions: independence, psychological integration, physical integration, and social integration. The internal reliability for the scale was .68. The summed score (possible range 0–12) of the overall scale served as the dependent variable.
Data analysis
We compared the schizophrenia and community comparison groups on the community integration scale using Mann-Whitney U tests and chi square analyses. In examining predictors of community integration within the schizophrenia group, we used a hierarchical regression analysis with the variable sets of the ecosystem model entered in the following order: sociodemographic characteristics, psychosocial variables, and environmental variables. The dependent variable, the community integration scale, had a normal distribution. Cases in which data were missing were eliminated from the analysis. Because of the high correlation between the PANSS positive scores and the PANSS negative scores (.52), we entered the score sets separately in two regression analyses. There was no evidence of colinearity among the other independent variables in the regression analysis, with all variance inflation factors <1.77.
Our analyses contained multiple comparisons that increased the possibility of type I errors. There is considerable debate as to the value of corrections for such comparisons. However, much of our thinking regarding this matter is summarized by Perneger ( 27 ). He contended that, contrary to popular belief, the Bonferroni correction or other similar adjustments do not guarantee a "prudent" interpretation of results. He noted that the correction is actually a test of the universal null hypothesis. If one or more of the p values is less than the corrected value,the universal null hypothesis is rejected. We can say that the two groups are not equal for all the variables, but we cannot say which—or even how many—variables differ. Thus Bonferroni adjustments provide a correct answer to a largely irrelevant question. Perneger also noted that type II errors are just as serious as type I errors. In exploratory studies of the type presented here, it is important to not overlook potentially clinically relevant variables, especially in the interpretation of the regression analysis.
Results
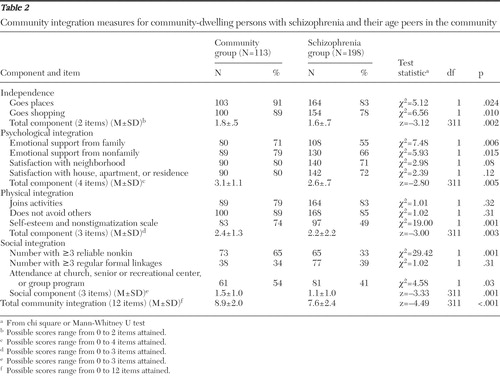
Table 1 shows the components of community integration determined from the principal-components analysis and the items for each dimension. There was a significant difference in the distribution of the community integration scale scores, with 46 (41%) participants in the community comparison group scoring in the top three categories, versus 45 (23%) participants in the schizophrenia group ( Figure 1 ). There was also a significant difference in overall mean scores of the community comparison group and the schizophrenia group (8.9 versus 7.6) ( Table 2 ). Persons with schizophrenia differed significantly from those in the community comparison group on seven of the 12 items of the scale ( Table 2 ). Moreover, overall mean scores for each of the four dimensions of community integration differed significantly between groups ( Table 2 ).
 |

 |
For the schizophrenia group, we examined the personal and environmental factors in the ecosystem model associated with community integration. In regression analysis, seven variables attained significance: being female, higher personal income, lower CES-D scores, lower PANSS positive scale scores, lower AIMS scores, greater likelihood of a CAGE positive history, and greater satisfaction with control of one's life ( Table 3 ). The personal variable set in the model attained significance, although within this set, the psychosocial variable subset attained significance whereas the sociodemographic variable subset did not. The environmental variable set also attained significance. The overall model was significant and accounted for 49% of the explained variance. When we substituted the PANSS negative symptoms scale for the PANSS positive symptoms scale, the results attained significance ( β =-.34, t=-4.71, df=183, p<.001). The other variables did not change significance.
 |
We conducted several post hoc analyses. We found a significant correlation between history of alcohol problems and only one of 12 community integration scale items (having three or more reliable social contacts; r=.14, df=196, p=.04). We also examined the association between the type of antipsychotic medication and the AIMS scores. Among persons with complete medication information and those who took only one antipsychotic medication (N= 145, 73%), we found no significant differences in mean AIMS scores between those who were taking first-generation versus second-generation antipsychotic medications (3.0 versus 4.6).
Discussion
The study supported our hypothesis that older adults with schizophrenia would have lower rates of community integration than their age peers in the general community. These findings confirmed the results of the only other comparative study using a multidimensional community integration model ( 6 ). However, we found group differences on all four community integration dimensions, whereas Aubry and Myner ( 6 ) found group differences in the social integration dimension but not in the physical or psychological integration dimensions. These differences may reflect their use of a smaller, presumably younger sample who had a range of psychiatric diagnoses (only 57% with schizophrenia) and were living in supported housing programs in Canada.
Our study provides provisional data about what level of community integration is attained by older persons with schizophrenia and in so doing suggests possibilities for what might be achieved. Members of the community comparison group were nearly twice as likely as those in the schizophrenia group to be in the top three categories in the community integration scale (general community, N=46, or 41%, versus schizophrenia, N=45, or 23%). If we used the strictest criteria—that is, meeting criteria for all 12 items—only nine (8%) and seven (4%) participants in the community comparison group and schizophrenia group, respectively, attained that level. Obversely, 17 (15%) persons in the community group fell into the lowest six tiers on the scale, whereas 63 (32%) of those in the schizophrenia group were in those tiers. We are uncertain about the most appropriate cutoff level for community integration, although it seems that people with schizophrenia did about half as well as their community age peers. The findings suggest that fulfilling all 12 categories may be unrealistic for older adults with schizophrenia, especially because persons in the general community rarely attain it. It should be noted that older community adults with higher income might have attained even better scores on community integration, as suggested by its association with personal income ( Table 3 ).
With respect to the main hypothesis, we confirmed the value of Moos' ecosystem model as a conceptual approach for examining factors associated with community integration. Both the personal and environmental variable categories were significant. The overall model was significant, and the variables explained nearly half the variance in community integration. The explained variance was more than twice the variance explained for each of the separate dimensions in Gulcur and coauthors' ( 4 ) study; however, further refinement of our model may yield even greater explanatory power.
Our findings that community integration was associated with lower levels of positive or negative symptoms and lower levels of depressive symptoms are consistent with earlier studies that found significant associations between lower levels of psychopathology and community integration ( 11 , 12 , 28 ). From a practical standpoint, improvements in community integration might result from more aggressive treatment of clinical symptoms, especially depressive symptoms, which in contrast to positive symptoms often go untreated ( 29 ). However, because our data are cross-sectional, we cannot be certain of causal direction, and it is possible that lower levels of community integration may increase clinical symptoms.
The finding that abnormal movements were associated with diminished community integration is consistent with previous studies that found a relationship between abnormal movements and social adaptation ( 30 , 31 ). Although we found no difference between persons who were receiving first-generation versus second-generation antipsychotic medications, this finding was probably because all persons had been exposed to first-generation medications, often for many years. Since the use of second-generation medications or lower doses of first-generation medications can reduce the risk and severity of tardive dyskinesia ( 32 ), such strategies may also indirectly serve to improve community integration.
A somewhat paradoxical finding was the fact that current or past history of alcohol problems was associated with better community integration. The literature has typically found alcoholism to be associated with poor social and coping skills ( 33 , 34 ). Nevertheless, Gulcur and colleagues ( 4 ) found conflicting results regarding substance abuse treatment, with participation increasing physical integration but decreasing social integration. We found a significant correlation between history of alcohol problems and only one of the community integration scale items (having at least three reliable social contacts). We are uncertain whether persons with alcohol abuse or dependence histories perceive their relationships as more reliable or whether they are more adept at making stronger social ties.
With respect to nonclinical personal predictors, we found that being female and having higher income were significantly associated with better community integration. In some earlier studies, women were involved in fewer activities in the community than men were ( 35 , 36 ). On the other hand, Gulcur and associates ( 4 ) observed a trend for an association between female gender and the independence component. The relationship between higher income and community integration was consistent with some earlier reports that found that having sufficient spending money was associated with greater community integration ( 11 , 13 ). Although causal direction cannot be determined here, it raises the possibility that improving financial well-being might enhance community integration. Finally, with respect to environmental factors, only one variable (greater satisfaction with control over one's life) attained significance in the regression analysis. This finding was consistent with earlier findings that consumer choice and a lower proportion of rigid routines were associated with greater community integration ( 4 , 9 ).
Several variables, such as race ( 10 ), age ( 9 , 10 , 11 , 37 ), and type of residential status ( 8 ), that had been significant in earlier studies were not significant in our analyses. The absence of significant findings for these variables may reflect differences in samples (especially age) and instruments.
To our knowledge, this is the first American study to examine community integration among older adults with schizophrenia. Our study has several strengths: a four-dimensional measure of community integration, with acceptable internal reliability, derived from factor analysis, the validity of which is provisionally supported by its correspondence with the four components identified previously ( 4 ); use of a theoretical model; a large multiracial sample; and a community comparison group. Nevertheless, our study was limited by the use of cross-sectional data, was a secondary analysis of data that were not designed primarily to study community integration, was confined to one geographical area, and was based on a convenience sample recruited from outpatient programs and supported residences, thereby excluding persons who were no longer in treatment or living in institutions.
Conclusions
Our study confirmed both of our hypotheses: first, that older adults with schizophrenia have lower levels of community integration than their age peers within the community, and second, that our model for community integration can identify potentially ameliorable clinical and social variables that may be targets for intervention research, including depression, movement disorders, positive and negative symptoms, personal autonomy, and income supports. Future studies must first replicate these findings in other samples of older persons with schizophrenia as well as demonstrate the utility of our community integration instrument. Moreover, if individuals with schizophrenia averaged one component higher on the summed community integration instrument, they would approach the levels of their age peers. Thus future intervention studies might also target the scale items that differed most substantially between the two groups, such as aspects of social and psychological engagement.
Acknowledgments and disclosures
This study was funded by grants SO6-GM-74923 and SO6-GM-5465 from the National Institute of General Medical Sciences.
The authors report no competing interests.
1. McAlpine DD: Patterns of care for persons age 65 years and older with schizophrenia; in Schizophrenia Into Later Life: Treatment, Research, and Policy. Edited by Cohen CI. Arlington, Va, American Psychiatric Publishing, 2003Google Scholar
2. Lieberman JA, Drake RE, Sederer LI, et al: Science and recovery in schizophrenia. Psychiatric Services 59:487–496, 2008Google Scholar
3. Bond GR, Salyers MP, Rollins AL, et al: How evidence-based practices contribute to community integration. Community Mental Health Journal 40:569–588, 2004Google Scholar
4. Gulcur L, Tsemberis S, Stefancic A, et al: Community integration of adults with psychiatric disabilities and histories of homelessness. Community Mental Health Journal 43:211–228, 2007Google Scholar
5. Wong YI, Solomon PL: Community integration of persons with psychiatric disabilities in supportive independent housing: a conceptual model and methodological considerations. Mental Health Services Research 4:13–28, 2002Google Scholar
6. Aubry T, Myner J: Community integration and quality of life: a comparison of persons with psychiatric disabilities in housing programs and community residents who are neighbours. Canadian Journal of Community Mental Health 15:5–20, 1996Google Scholar
7. Cohen CI, Vahia I, Reyes P, et al: Schizophrenia in later life: clinical symptoms and social well-being. Psychiatric Services 59: 232–234, 2008Google Scholar
8. Depla MF, de Graaf R, van Busschbach JT, et al: Community integration of elderly mentally ill persons in psychiatric hospitals and two types of residences. Psychiatric Services 54:730–735, 2003Google Scholar
9. Kruzich JM: Community integration of the mentally ill in residential facilities. American Journal of Community Psychology 13: 553–563, 1985Google Scholar
10. Nagy MP, Fisher GA, Tessler RC: Effects of facility characteristics on the social adjustment of mentally ill residents of board-and-care homes. Hospital and Community Psychiatry 39:1281–1286, 1988Google Scholar
11. Segal SP, Everett-Dille L: Coping styles and factors in male/female social integration. Acta Psychiatrica Scandinavica 61:8–20, 1980Google Scholar
12. Silverman CJ, Segal SP: Who belongs? An analysis of ex-mental patients' subjective involvement in the neighborhood. Adult Residential Care Journal 8:103–113, 1994Google Scholar
13. Segal SP, Aviram U: The Mentally Ill in Community Based Sheltered Care: A Study of Community Care and Social Integration. New York, Wiley, 1978Google Scholar
14. Moos RH: Evaluating Treatment Environments: The Quality of Psychiatric and Substance Abuse Programs, 2nd ed. New Brunswick, NJ, Transaction, 1997Google Scholar
15. Bankole AO, Cohen CI, Vahia I, et al: Factors affecting quality of life in a multiracial sample of older persons with schizophrenia. American Journal of Geriatric Psychiatry 15:1015–1023, 2007Google Scholar
16. Jeste DV, Symonds LL, Harris MJ, et al: Non-dementia non-praecox dementia praecox? Late-onset schizophrenia. American Journal of Geriatric Psychiatry 5:302–317, 1997Google Scholar
17. Kahn RL, Goldfarb AI, Pollack M, et al: Brief objective measures for the determination of mental status in the aged. American Journal of Psychiatry 117:326–328, 1960Google Scholar
18. Radloff LS: The CES-D Scale: a self-report depression scale for research in the general population. Journal of Applied Psychological Measurement 1:385–401, 1977Google Scholar
19. Kay SR, Opler LA, Fiszbein A: Positive and Negative Syndrome Scale User's Manual. North Tonawanda, NY, Multi-Health Systems, 1992Google Scholar
20. Mattis S: Mental Status Examination for organic mental syndrome in the elderly patient; in Geriatric Psychiatry. Edited by Bellak L, Karasu TB. New York, Grune and Stratton, 1976Google Scholar
21. Lawton MP, Moss M, Fulcomer M, et al: A research and service oriented multilevel assessment instrument. Journal of Gerontology 37:91–99, 1982Google Scholar
22. National Institute of Mental Health Psychopharmacology Research Branch: Development of a Dyskinetic Movement Scale. ECDEU Intercom 4:3–6, 1975Google Scholar
23. Rosenberg M: Conceiving the Self. New York, Basic Books 1979Google Scholar
24. Bernadt MW, Mumford J, Taylor C, et al: Comparison of questionnaire and laboratory tests in the detection of excessive drinking and alcoholism. Lancet 6:325–328, 1982Google Scholar
25. Sokolovsky J, Cohen CI: Toward a resolution of methodological dilemmas in network mapping. Schizophrenia Bulletin 7: 109–116, 1981Google Scholar
26. Nunally JC: Psychometric Theory. New York, McGraw-Hill, 1967Google Scholar
27. Perneger TV: What's wrong with Bonferroni adjustments. British Medical Journal 316:1236–1238, 1998Google Scholar
28. Timko C, Moos RH: Outcomes of the treatment climate in psychiatric and substance abuse programs. Journal of Clinical Psychology 54:1137–1150, 1998Google Scholar
29. Diwan S, Cohen CI, Bankole AO, et al: Depression in older adults with schizophrenia spectrum disorders: prevalence and associated factors. American Journal of Geriatric Psychiatry 15:991–998, 2007Google Scholar
30. Cohen CI, Talavera N: Functional impairment in older schizophrenic persons: toward a conceptual model. American Journal of Geriatric Psychiatry 8:237–244, 2000Google Scholar
31. Eastham JH, Jeste DV: Treatment of schizophrenia and delusional disorder in the elderly. European Archives of Psychiatry and Clinical Neuroscience 247:209–218, 1997Google Scholar
32. Jeste DV, Rockwell E, Harris MJ, et al: Conventional vs newer antipsychotics in elderly patients. American Journal of Geriatric Psychiatry 7:70–76, 1999Google Scholar
33. Scheier LM, Botvin GJ, Diaz T, et al: Social skills, competence, and drug refusal efficacy as predictors of adolescent alcohol use. Journal of Drug Education 29:251–278, 1999Google Scholar
34. Ilgen M, McKellar J, Moos R: Personal and treatment-related predictors of abstinence self-efficacy. Journal of Studies on Alcohol and Drugs 68:126–132, 2007Google Scholar
35. Prince PN, Gerber GJ: Subjective well-being and community integration among clients of assertive community treatment. Quality of Life Research 14:161–169, 2005Google Scholar
36. Nikkonen M: Life after the mental hospital: the way of life of deinstitutionalized psychiatric patients. Journal of Psychiatric and Mental Health Nursing 3:373–383, 1996Google Scholar
37. Sherman SR, Newman ES, Frenkel ER: Community acceptance of the mentally ill in foster family care. Health and Social Work 9:188–199, 1984Google Scholar



