Conditional Release in Western Australia: Effect on Hospital Length of Stay
Involuntary outpatient commitment statutes require individuals' participation in proffered mental health care. These are individuals who, because of a mental disorder, pose a danger to themselves or others or need treatment but refuse to accept it on a voluntary outpatient basis. Mandated compliance may extend to requiring someone to live in a particular apartment, take prescribed medications, attend counseling sessions, and abstain from illicit substances ( 1 ). A community treatment order is the legal action for involuntary outpatient commitment. This study evaluated use of community treatment orders in Western Australia where previous research has reported that these orders do not affect hospital utilization in overall number of admissions or in days of hospitalization ( 2 ). This study offers an alternative perspective that is based on length of stay for each admission.
There are two primary ways in which community treatment orders are used. First, in by far the oldest and most used approach ( 3 ), a person is placed on orders as a form of conditional release from involuntary hospitalization as part of an aftercare plan and as a means to shorten the duration of the hospitalization. Second, the person is placed on orders directly from the community to prevent hospitalization. Outpatient commitment research, most notably three comparison group studies ( 2 , 4 , 5 ), has focused primarily on preventing hospitalization. These studies considered how outpatient commitment reduced the likelihood of a future hospitalization but did not address whether outpatient orders for conditional release are effective in reducing the duration of an episode of hospital care. Two of these studies focused on prevention by randomizing the sample without attention to current inpatient episode ( 4 , 5 ); the third study statistically controlled for the effects of preceding hospitalizations ( 2 ). Because the primary utility of community treatment orders in a conditional release system is the provision of an alternative to hospitalization that enables shortening hospital stays for a population selected because of their history of long-term inpatient care episodes ( 3 ), this investigation aimed to expand the focus of the Western Australia study ( 2 ) to consider the conditional release function of community treatment orders in that system. Analysis focused on the change in the duration of each hospitalization episode that could be accounted for by the introduction of community treatment orders.
The 1996 Mental Health Act of Western Australia ( 6 ) was implemented in November 1997 ( 7 ). As with legislation for other parts of Australia and New Zealand, the act includes provision for involuntary treatment in the community through the introduction of a community treatment order ( 8 ). The legal provisions of the act use the same behavioral criteria for both involuntary inpatient admission and placement on a community treatment order. [A summary of the legal provisions is available as an online supplement to this article at ps.psychiatryonline.org .] The provisions require, as soon as deemed possible, that an involuntary hospitalization be terminated and that placement within the community be initiated by means of a community treatment order as a less restrictive alternative. Specifically, the act requires a psychiatrist who is evaluating the continued involuntary detention of a person "to consider whether the object[ive] of the act would be better achieved by making a community treatment order in respect of the person" ( 6 ).
Persons confined involuntarily are most frequently experiencing rapid remission from an acute psychotic episode ( 9 ). The assessment of the extent to which a person because of his or her mental illness continues to be a danger to self or others or in need of treatment to protect health or safety (thereby continuing to meet the involuntary detention standard) is an inexact science. At some point in remission the person's status enters a gray area; for example, he or she meets the standard yet might be able to function without untoward consequences in a community placement with supervision that offers structure and protective oversight. Unlike patients released without a community treatment order, patients on orders with a treatment plan—including the attendance of counseling sessions—are monitored periodically by a special review board for conformity with the orders.
Before the implementation of the act, individuals who continued to meet the standard of involuntary detention were hospitalized because there was no alternative. The act encourages conditional release as an alternative to recurring hospital admissions. Although there was no direct increase in community service resources with the introduction of the act aside from funds for training community mental health staff in the act's implementation, it was expected that the legal requirement for participation, the periodic monitoring of that participation, and the threat of a return to the hospital would lead to increased outpatient service use by the group with community treatment orders. This assumption was tested in this study. Thus, if the act has achieved its intent, then the gray area of conformity to the involuntary standard—the time during any given involuntary admission episode spent in a hospital before the act was implemented—would now be spent in the community under a community treatment order, thereby shortening the duration of hospitalization episodes. Eighty-five percent of community treatment orders in Western Australia are used as a form of conditional release with the aim of facilitating an earlier hospital discharge.
Previous work from Western Australia compared hospitalization stays after implementation of the act between groups with and without community treatment orders; the analyses controlled for stays before implementation. It is possible that this control procedure statistically removed from consideration the functional objective of community treatment orders in conditional release—the shortening of an existing episode of care. To determine whether community treatment orders shortened hospitalization episodes, this study also compared patients given community treatment orders with those who were not, but this study used an altered criterion variable—a measure of change in inpatient episode duration. The patient's average length of hospitalization before the community treatment order was subtracted from the patient's average hospitalization after receipt of the community treatment order to yield a change in episode duration score. A comparison of the change in episode duration scores was then made for patients who were and were not subject to community treatment orders in the period after the act's implementation. The study thus compared the groups on the change in inpatient utilization accounted for by the introduction of the community treatment order as a less restrictive alternative to continued hospitalization.
Methods
Data and design
A logical time span of data to use for pre-post intervention analyses was 1997 through 1998 because community treatment orders went into effect in November 1997. Although a decade has passed since the implementation of this law, significant changes in the law, the service system, and the funding of the service system have not occurred during this period. Therefore, the 1997–1998 data are still relevant to the analysis of this important policy issue. Other studies of community treatment orders have used postintervention data for periods of approximately 12 months ( 2 , 4 , 5 ). Therefore, a 12-month follow-up period was used in this study to enable comparisons with the prior studies.
Sample
Data were obtained by the Western Australia Group ( 2 ) as part of a larger investigation of the effects of community treatment orders. Individuals were selected from the Western Australia Mental Health Information System, which records inpatient, outpatient, and community visits to psychiatric inpatient units, general hospitals, and community mental health services in the state. This information system was linked with two other databases: one administered by the Mental Health Review Board that records involuntary admissions under the Mental Health Act and the other the Police Offenders database of all offenses and convictions in Western Australia. All data were subsequently deidentified. Use of these three registers captured data for all individuals placed on community treatment orders in the entire state during the study period. The study sample included all individuals placed on orders between November 13, 1997 (the date of implementation of the Mental Health Act 1996), and November 31, 1998, and a matched comparison group who had been admitted to a hospital in the same period but had not been placed on an order.
Comparison group members were matched on sex, Aboriginal ethnicity, an age difference of less than two years, and a weighted set of clinical and demographic characteristics. Although attempts were made to match on prior hospitalization, this was not possible because the community treatment order group had significantly more extensive hospital utilization before their placement on orders than did the matched comparison group. A total of 456 people were included in the original larger study sample ( 2 ), which consisted of all 228 persons placed on community treatment orders in the period and 228 persons matched to the first group to enable comparisons.
In order to evaluate the utility of community treatment orders as a form of conditional release, only individuals from the larger sample who were hospitalized both before and after the act's implementation were evaluated: 246 individuals, 129 placed on community treatment orders (57% of the 228 individuals placed on orders in the period) and 117 (51%) of the persons matched for comparison. Of the 456 original sample members, we chose those who were hospitalized both before and after the act's implementation because it is not possible to be placed on conditional release unless one is hospitalized, and in evaluating change in the number of hospitalization episode days pre- and postimplementation the person had to have the opportunity to be placed on conditional release.
We also included in the sample all patients hospitalized before and after enactment who received a community treatment order rather than only those placed on conditional release. We did so because all but four of the 33 patients who received preventive orders also received a conditional release order. In other words, they had multiple hospitalizations and multiple community treatment orders. Although some of these orders were preventive, the result of such a preventive effort was thought to influence how subsequent conditional releases were or were not granted and needed to be taken into account if the effects of conditional release on inpatient episode duration are to be understood in the context of an inpatient treatment history. Finally, although it would have been desirable to match the groups on prior hospitalization, this data set, as noted above, was created as part of a larger evaluation that did not include such matching. Therefore, this procedure could not be used.
Measurement
Primary measures. Inpatient episode duration was measured by the number of days from admission to release from a psychiatric hospital. As noted above, the primary dependent variable used herein is a change score measuring the difference between a person's inpatient episode duration before and after the implementation of the community treatment order legislation. The primary independent variable was group status.
Potential confounders. Potential confounders, associated in previous research with admission to a psychiatric hospital or compulsory community treatment ( 2 , 3 , 4 , 5 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 ), were taken into account in the model. Demographic characteristics included gender (coded 1 for male and 0 for female), age in years, and Aboriginal ancestry (yes, 1; no, 0). Schizophrenia and affective psychosis diagnoses were recorded (yes, 1; no, 0). Functional status indicators included never having married, having an occupation, and completing high school or education beyond high school (for each item, yes was coded 1 and no was coded 0).
Outpatient service effects. We measured the number of outpatient service contacts and the interaction of community treatment order status with number of service contacts. The latter tested the combined effect of the expected increase in required use of mental health services and any unique features of such services for patients placed on orders.
Utilization controls. The analysis included three utilization controls. First, given that the primary determinant of hospital utilization is usually found to be prior hospitalization ( 12 ), we included the number of inpatient days a person had accumulated before enactment of the law. Second, we used year of first inpatient admission to control for the effect of the deinstitutionalization trend toward briefer hospital stays. Third, we included unsuccessful community-initiated orders, or orders initiated in the community that were intended to be preventive but resulted in hospitalization (entered as 1 for yes and 0 for no). This measure was included because a patient's hospital admission after the failure of a community-initiated order was likely to delay, stop, or contraindicate the use of subsequent conditional release (given the observed limited utility of such orders for the patient). The failure to use conditional release for such a patient or the use of orders only after the clinician has increased certainty of a successful community adjustment is likely to extend the duration of the patient's current and perhaps future inpatient episodes. This was found to be the case in the use of community treatment orders among patients who had both conditional release orders and preventive orders in Victoria, Australia ( 13 ). Persons with failed community-initiated orders may be the most seriously ill—those who cycle in and out of the hospital ( 14 ).
Area of residence. Residential areas were described as metropolitan versus other in order for the analysis to account for differential service availability outside of metropolitan areas.
Criminal offender status. A criminal offense was indicated if there was a recorded offense or an imprisonment (the equivalent of jail time or imprisonment in the United States) before the law's implementation. Defendants with mental illness cannot be placed on a community treatment order. Thus their experience was controlled for in the analysis ( 6 ).
Analysis
All analyses were completed with SPSS, version 15. This article reports on descriptive characteristics of the reduced sample; the total sample has been described elsewhere ( 2 ). A multivariate analysis of covariance was used to evaluate the impact of community treatment orders on change in inpatient episode duration after taking account of the control variables. Unstandardized coefficients (b) for each independent variable were used for establishing a prediction model for the change in inpatient days after the introduction of community treatment orders. Standardized coefficients (beta) were used to determine the relative importance of each independent variable in the model in contributing to the change in inpatient days.
Institutional review board approvals were obtained from the Committee for the Protection of Human Subjects, University of California, Berkeley, and from the Confidentiality of Health Information Committee, Department of Health, Western Australia.
Results
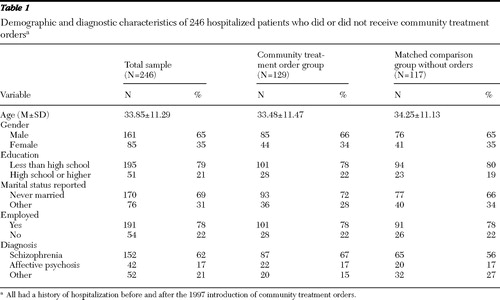
The sample included 246 people, 129 with community treatment orders and 117 without orders who were matched for control in the analysis. Their demographic and diagnostic characteristics are summarized in Table 1 . The differences between the groups were small, although the most notable one was diagnostic—more individuals with schizophrenia were present in the community treatment order group (67% versus 56%).
 |
The between-group difference in mean±SD occasions of outpatient service use before implementation of the legislation was significant. The community treatment order group had 69.7±86.3 occasions of service, and the comparison group had 28.3±41.4 (N=244, F=19.38, df=1 and 243, p<.001). The between-group difference in outpatient occasions of service after implementation was also significant; the community treatment order group had 89.7±106.0 occasions of service compared with 36.2±52.0 for the control group (N=244, F=21.32, df=1 and 243, p<.001). Although both groups increased their utilization of outpatient services both before and after implementation, the community treatment order group by 20 occasions of service and the comparison by seven, these increases were not significantly different.
The between-group difference in inpatient hospitalization days per inpatient episode before implementation of the legislation was significant. The community treatment order group's average was 46.3±46.5 days, whereas that of the matched control group was 30.0±37.1 days (N=244, F=7.85, df=1 and 243, p=.006). After implementation of the legislation, there was no difference in hospitalization days per inpatient episode between the groups. Both groups had 26-day episodes. Table 2 shows the multivariate analysis of covariance results. The model produced significant results (R 2 =.23, adjusted R 2 =.17; N=243, F=3.99, df=17 and 226, p<.001). After taking all control factors into account, we found that the use of community treatment orders for conditional release accounted for a 19.16-day reduction per episode of hospitalization (b=19.16, SE=9.00, β =.16; t=2.13, df=1, p=.034).
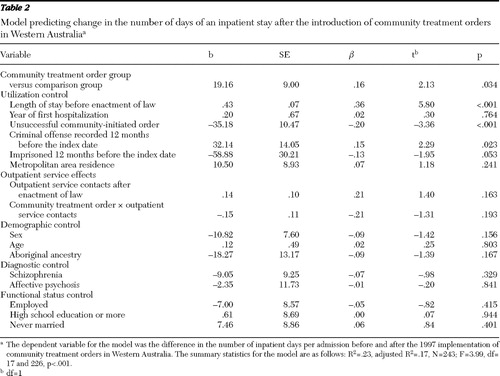 |
Unsuccessful community-initiated orders in the model were associated with a significant increase in hospitalization days in the postimplementation period (b=–35.18, SE=10.47, β =–.20, t=–3.36, df=1, p<.001), an increase of 35.18 days per hospitalization in this group. The most important significant predictors of change in hospital duration between periods were length of inpatient hospitalization during the preimplementation period ( β =.36), unsuccessful community-initiated orders ( β =–.20), and placement on community treatment order to conditional release ( β =.16).
Discussion
This study suggests that the conditional release function of community treatment orders shortened individual hospital stays. The study findings were consistent with experience in Victoria, Australia, where the introduction of community treatment orders was also associated with shortened inpatient episodes over a ten-year period ( 3 ). This study extended the findings from Victoria by using a pre-post legislation design and change score methodology to evaluate the size of the effect. The results indicate that there was a greater reduction in inpatient days per hospitalization in the community treatment order group compared with the matched control group. The 19.16-day savings per inpatient stay attributable to the use of community treatment orders is the equivalent of a 47% reduction in the duration of a preimplementation inpatient episode after all other factors were taken into account. This result is consistent with another study that compared individuals across jurisdictions, where one jurisdiction had community treatment orders and the other did not have such legislation ( 15 ). This comparison showed that individuals on community treatment orders were significantly less likely to have subsequent inpatient episodes of more than 100 days.
The study also observed a significant increase in average episode duration—almost a doubling—for those with unsuccessful community-initiated orders. This finding is consistent with other studies ( 4 , 5 , 16 , 17 , 18 ) in which community treatment orders did not prevent hospitalization and a recent study in Victoria that identified the patient characteristics and treatment situations associated with successful (preventive) community treatment orders ( 13 ).
This study's results thus appear to indicate that community treatment orders are most effective in reducing the duration of an inpatient episode when used in the form of a conditional release. On the other hand, when initiated for or on behalf of someone still residing in the community—someone who needs treatment but has not been hospitalized—the community treatment order may be on the "late" side, coming either as an attempt to save a failing program of care with which the person is not cooperating by providing a set of rules to which the person must conform in order to avoid hospitalization or as an initial attempt to avoid hospitalization for an outpatient whose mental condition has deteriorated badly. Although use of outpatient services has increased since the community treatment order legislation was enacted, this study failed to show that the increase is attributable to the use of the community treatment orders. If patients on community treatment orders are not using more outpatient services, then this may account for the failure of such orders to prevent hospitalization. Without linkage to outpatient care, those placed on community treatment orders in the community may be subject to neglect, causing further deterioration and leading to longer inpatient stays. A study in Victoria that found links between the increase in use of outpatient services and the use of community treatment orders ( 17 ) indicates that judicious selection of persons for community treatment orders is crucial in implementing the preventive function of these orders ( 18 ). Use of community treatment orders to prevent a first hospitalization is likely to fail, although subsequent use is likely to succeed for a selected subset of individuals ( 18 ).
This study has limitations. It did not provide the level of causal certainty of a randomized clinical trail. Yet it brought a stronger design to evaluate the utility of conditional release than has been previously reported in the literature, and it replicated the Victoria experience.
Conclusions
The study implications emphasize the necessity of adopting a functional approach to the evaluation of the use of community treatment orders. The community treatment order is a tool to facilitate service delivery; it is not a treatment or a cure for psychosis. The results of its use are only as good as the associated treatment efforts. In the case of conditional release, the mental health service system requires little resource investment to shorten the duration of a hospital episode. With increased investment of outpatient service resources, keeping individuals within the protective oversight of the community treatment order has yielded significant results in the prevention of victimization ( 19 ) and in the reduction of premature deaths ( 20 ). Results in Western Australia might have shown more broad-based positive outcomes had use of community treatment orders been linked to increased outpatient service use. Understanding this linkage is an important objective for future research on community treatment orders. Some useful aspects of community treatment orders have yet to be substantiated in studies with controlled comparison group designs, notably the use of such orders to deliver assisted treatment ( 2 , 21 ) and to stop "revolving-door" admissions ( 4 , 5 , 15 ). Some studies have yielded contradictory findings about useful aspects of community treatment orders, such as a study without a comparison group that found that such orders enhanced treatment compliance ( 22 ) and a study with a comparison group that showed the opposite effect ( 17 ).
Our study illustrates the importance of closely tying evaluative design to the function of the intervention and selecting a dependent variable that directly addresses the intervention objective. Multiple outcome measures can and should be used to address the multiple functions of community treatment orders. These include number of admissions, community survival, total hospitalization days, and hospitalization days per episode. If the aim of conditional release is to reduce hospitalization days per episode, our study indicates success in this area, if not in other outcomes.
Acknowledgments and disclosures
The authors report no competing interests.
1. Monahan J, Bonnie RJ, Appelbaum PS, et al: Mandated community treatment: beyond outpatient commitment. Psychiatric Services 52:1198–1205, 2001Google Scholar
2. Preston NJ, Kisely S, Xiao J: Assessing the outcome of compulsory psychiatric treatment in the community: epidemiological study in Western Australia. British Medical Journal 524:1244–1246, 2002Google Scholar
3. Segal SP, Burgess P: Conditional release: a less restrictive alternative to hospitalization? Psychiatric Services 57:1600–1606, 2006Google Scholar
4. Swartz MS, Swanson JW, Hiday VA, et al: Can involuntary commitment reduce hospital recidivism? Findings from a randomized trial with severely mentally ill individuals. American Journal of Psychiatry 12:1968–1974, 1999Google Scholar
5. Steadman HJ, Gounts K, Dennis D, et al: Assessing the New York City Involuntary Outpatient Commitment Pilot Program. Psychiatric Services 52:330–337, 2001Google Scholar
6. Western Australia Mental Health Act 1996 (no 68 of 1996). Perth, Western Australia, Mental Health Review Board. Available at www.mhrbwa.org.au/publications Google Scholar
7. Rolfe T: Community-treatment orders: a review. Perth, Western Australia, Department of Health, Office of the Chief Psychiatrist, 2001Google Scholar
8. Gerrand V: Transforming Mental Health Services From 1993 to 1998 in Victoria, Australia: A Case Study of Policy Implication. Doctoral dissertation, University of Melbourne, Department of Political Science, 2006Google Scholar
9. Gruenberg ED, Turns D, Segal SP, et al: Social breakdown syndrome: environmental and host factors associated with chronicity. American Journal of Public Health 62:91–94, 1972Google Scholar
10. Xiao J, Preston NJ, Kisely S: What determines compulsory community treatment? A logistic regression analysis using linked mental health and offender databases. Australian and New Zealand Journal of Psychiatry 38:613–618, 2004Google Scholar
11. Sensky T, Hughes T, Hirsch S: Compulsory psychiatric treatment in the community: I. a controlled study of compulsory community treatment with extended leave under the Mental Health Act: special characteristics of patients treated and impact of treatment. British Journal of Psychiatry 158:792–799, 1991Google Scholar
12. Huntley DA, Cho DW, Christman J, et al: Predicting length of stay in an acute psychiatric hospital. Psychiatric Services 49:1049–1053, 1998Google Scholar
13. Segal SP, Burgess PM: Use of community treatment orders to prevent psychiatric hospitalization. Australian and New Zealand Journal of Psychiatry 42:733–740, 2008Google Scholar
14. Solomon P, Draine J, Marcus SC: Predicting incarceration of clients of a psychiatric probation and parole service. Psychiatric Services 53:50–56, 2002Google Scholar
15. Kisely S, Smith M, Preston NJ, et al: A comparison of health service use in two jurisdictions with and without compulsory community treatment. Psychological Medicine 35:1357–1367, 2005Google Scholar
16. Kisely S, Smith M, Preston NJ, et al: Impact of compulsory community treatment on admission rates: survival analysis using linked mental health and offender databases. British Journal of Psychiatry 184:432–438, 2004Google Scholar
17. Segal SP, Burgess P: The utility of extended outpatient civil commitment. International Journal of Law and Mental Health 29:525–534, 2006Google Scholar
18. Burgess P, Bindman J, Leese M, et al: Do community treatment orders for mental illness reduce readmission to hospital? An epidemiological study. Social Psychiatry and Psychiatric Epidemiology 41:574–579, 2006Google Scholar
19. Hiday VA, Swartz MS, Swanson JW, et al: Impact of outpatient commitment on victimization of people with severe mental illness. American Journal of Psychiatry 159:1403–1411, 2002Google Scholar
20. Segal SP, Burgess P: Effect of conditional release from hospitalization on mortality risk. Psychiatric Services 57:1607–1613, 2006Google Scholar
21. Muirhead D, Harvey C, Ingram G: Effectiveness of community treatment orders for treatment of schizophrenia with oral or depot antipsychotic medication: clinical outcomes. Australian and New Zealand Journal of Psychiatry 40:596–605, 2006Google Scholar
22. Van Putten DA, Santiago JP, Bergen MR: Involuntary commitment in Arizona: a retrospective study. Hospital and Community Psychiatry 39:953–958, 1988Google Scholar



