Persistent Depression and Anxiety in the United States: Prevalence and Quality of Care
Persistent psychiatric illnesses are a major national health care challenge ( 1 ). These persistent illnesses include depressive and anxiety disorders. Although these common psychiatric disorders are often time limited, substantial morbidity and social burden arises from the population of individuals who remain persistently ill ( 2 , 3 ). A study from the Netherlands found that 20% of adults with new onset of major depression remained ill at 24 months ( 4 ). Research in treatment settings has found that anxiety and depressive disorders are often persistent, with substantial morbidity ( 5 , 6 ).
Both antidepressant medication and cognitive-behavioral psychotherapy are effective in treating persistent depression ( 3 , 7 ). Research also supports the efficacy of cognitive-behavioral therapy, certain antidepressant medications, and benzodiazepines for persistent panic and generalized anxiety disorder ( 8 , 9 , 10 , 11 ). However, relatively little is known about the national prevalence of persistent anxiety and depressive disorders in the United States or about treatment use in this population. It would be valuable to know which individual characteristics affect treatment use and how often providers and health care organizations respond to persistent psychiatric illness by increasing the likelihood and intensity of treatment.
Researchers have been able to accurately estimate the overall national prevalence of depressive and anxiety disorders ( 12 , 13 ). In this population, treatment rates are increasing ( 12 , 14 , 15 ), although treatment is received by only about one-third of affected individuals ( 16 ). However, it has not been possible to characterize treatment use and the quality of treatment in the population of individuals with persistent depressive and anxiety disorders. Very few studies have surveyed nationally representative samples at more than one time point ( 4 , 17 ). The Epidemiologic Catchment Area study conducted a 15-year follow-up in Baltimore and found a median duration of eight to 12 weeks for major depression ( 18 ). The National Comorbidity Study assessed outcomes at ten years and found that outcomes were worse among those who had greater illness severity at baseline ( 19 ). Most research on persistent depression and anxiety has been conducted in specialty treatment settings ( 20 ) or selected primary care practices ( 21 ). Because the majority of affected individuals receive no treatment, studies from treatment settings cannot be used to characterize the overall population with persistent anxiety and depression.
Most individuals with acute depression are encountered in primary care. When treatment is initiated in primary care, many patients have good clinical, quality-of-life, and employment outcomes ( 22 ). For those with treatment-resistant disorders, however, there may be a particular need for consultation with and treatment from mental health specialists. In persistent depression, research supports the use of antidepressant medication combined with psychotherapy ( 3 ) and of multiple sequential antidepressant medication trials ( 23 ). Access to both of these is often limited in primary care. In response, researchers have implemented and demonstrated the effectiveness of "stepped" care models that facilitate the involvement of psychiatrists, increase treatment intensity, and improve outcomes ( 24 , 25 ).
It is not known nationally whether treatment rates are increasing for people with persistent illness or whether treatment intensity increases over time. A better understanding of problems in the quality of treatment could inform the development of interventions and policy to improve care. This study tracked 1,642 adults with probable major depression, dysthymia, panic disorder, or generalized anxiety disorder. Participants were drawn from a nationally representative sample and interviewed at baseline and approximately 32 months later. Because this was an observational study, the data cannot be used to estimate the effectiveness of treatments. Rather, the study evaluated whether treatments of known efficacy were delivered to individuals who were likely to benefit. The aim of this study was to provide national estimates of the prevalence of persistent depression and anxiety, and within this population, estimates of illness severity, treatment use, and treatment quality.
Methods
Sample
Data are from Healthcare for Communities (HCC), a longitudinal, nationally representative household survey of adults in the United States that began in 1997 ( 26 ). The objective of HCC was to track changes in health policy, access, service delivery, and outcomes within and across communities for persons at risk for alcohol, drug, and mental health conditions. The baseline wave of HCC was a stratified probability sample of participants in the Community Tracking Study (CTS), which was a Health Tracking Initiative study funded by the Robert Wood Johnson Foundation that focused on general medical care ( 27 ). The CTS sample was nationally representative and was drawn from 60 randomly sampled communities across the United States plus a supplemental national sample.
To improve power for analyses, HCC oversampled the following CTS groups: the national sample, individuals with family income less than $20,000, individuals with high psychological distress on a scale consisting of two items from the 12-item Short-Form Health Questionnaire (SF-12) ( 28 ), and individuals with any mental health specialty use during the previous year. Of the 14,985 CTS respondents selected for HCC, 9,585 were interviewed at baseline, for a response rate of 64%. HCC data were weighted by using CTS data to adjust for the probability of selection, unit nonresponse, and households without telephones. The HCC sample is representative of adults age 18 and older in the civilian, noninstitutionalized population of the continental United States. It closely matches the 1997 U.S. household population in demographic characteristics. Two to three years later, 6,659 (70%) of the baseline HCC respondents were interviewed for a second time. Differences between HCC responders and nonresponders at follow-up were small, suggesting that the samples were sociodemographically similar ( 29 ).
Measures
Data were collected with computer-assisted telephone interviewing. Baseline interviews (wave 1) occurred between October 1997 and December 1998, and follow-up interviews (wave 2) occurred between April 2000 and October 2001. After participants received a complete description of the study, verbal informed consent was obtained. The study was approved by the institutional review boards at the University of California, Los Angeles, and RAND.
The study reported here focused on a subsample of adults with probable depressive or anxiety disorder at the baseline interview. All survey items used in this study can be found on the HCC Web site at www.hsrcenter.ucla.edu/research/hcc.shtml . Ethnicity was defined by the respondent ( 16 ). At both waves, major depression, dysthymia, and generalized anxiety disorder during the past year and lifetime mania were defined by DSM-III-R criteria and assessed by using the Composite International Diagnostic Interview Short Form (CIDI-SF) ( 30 ), which has excellent sensitivity and specificity (90% to 100% concordance) compared with the full CIDI ( 31 ). Panic disorder was assessed by screening items from the CIDI ( 31 ) supplemented by additional items from the full battery that were modified for this study. To reduce potential false positives on this instrument, for panic we required limitation in social or role functioning, which we measured by two items from the SF-12 and three items from the Sickness Impact Profile ( 32 ).
Substance misuse was assessed by using the Alcohol Use Disorders Identification Test ( 33 ) and items adapted from the CIDI. Nonaffective psychosis was assessed by asking respondents whether they had ever been told they had schizophrenia or schizoaffective disorder or been hospitalized because of psychotic symptoms ( 26 ). A total of 240 respondents met criteria for psychosis or mania. Because treatment needs differ in this population, these persons were excluded from the analyses.
At both waves, suicidal ideation during the past 12 months was assessed by an item from the CIDI. Established scales were used to assess satisfaction with care, quality of life, functioning, and the presence of chronic medical conditions ( 28 , 34 ). Respondents provided information about their insurance status. Managed care was categorized as strong if it had primary care gate keeping, preauthorization for specialty care, and a closed provider panel ( 35 ). At the first wave, respondents were also asked whether during the past 12 months they had the following severe life difficulties: witnessing an assault, losing custody of a child, or being homeless, sexually assaulted, incarcerated, or on parole or probation.
Use of health services during the past 12 months was determined by self-report. Primary care provider visits included visits for any reason to a primary care doctor, family physician, general internist, nurse, physician assistant, or chiropractor. Mental health specialist visits included visits to a psychiatrist, psychologist, social worker, psychiatric nurse, or counselor for "emotional or mental health problems." Respondents provided the daily dosage and duration of use for each medication taken "at least several times a week for a month or more" and reported the number of counseling sessions with specialists. Counseling from primary care providers was identified by asking whether the health care visit included at least five minutes of counseling regarding an "emotional, mental health, alcohol, or drug problem."
For each depressive and anxiety disorder, the appropriateness of treatment was evaluated by using an established method ( 16 ). Appropriate care was defined as use of either appropriate psychotropic medication or appropriate counseling during the past year. Appropriate medication was defined as a medication proven to be efficacious for the diagnosed disorder and used at a dosage exceeding the minimum recommended dosage for an adequate duration. For major depression and dysthymia, we used the lower end of the therapeutic dosage range for each antidepressant medication from the Guideline for Depression in Primary Care of the Agency for Health Care Policy and Research ( 36 ), updated for newer medications. We required two or more months of use during the past 12 months. For panic disorder, appropriateness criteria were based on guidelines for general practitioners ( 37 ). Medication for panic disorder was appropriate if it included at least two months of an antidepressant medication (other than bupropion) at a potentially effective dosage or a benzodiazepine. For generalized anxiety disorder, medication was considered appropriate if it included at least two months of an antidepressant medication at an adequate dosage, buspirone, or a benzodiazepine.
For respondents with multiple disorders, appropriateness was evaluated for their most significant clinical disorder by means of the following hierarchy: major depression, dysthymia, panic disorder, and generalized anxiety disorder. To illustrate the rationale behind this hierarchy, individuals with comorbid major depression and panic disorder have appropriate treatment for both disorders if they have any appropriate treatment for depression (for example, an antidepressant); however, certain treatments for panic disorder (for example, a benzodiazepine and no counseling) would not be sufficient. Appropriate counseling was defined as at least four visits with a mental health specialist or four visits with a primary care provider that included counseling for mental health problems. A very similar counseling definition was previously found to be associated with improved two-year functional outcomes in depression ( 38 ).
Statistical analysis
Estimates were calculated by using SUDAAN software ( 39 ), and they take into account the complex survey design and survey clustering. Differences between proportions were evaluated using Wald statistics converted to F statistics ( 40 ). A multinomial logit model was used to examine the effect of baseline individual and insurance characteristics on the receipt of appropriate treatments at follow-up. The population for the model consisted of individuals with probable depression, dysthymia, panic disorder, or generalized anxiety disorder at follow-up. Independent variables were age, gender, racial or ethnic group, marital status, years of education, employment status, family income, number of chronic medical disorders, number of severe life difficulties, the presence of drug or alcohol misuse at baseline, and primary medical insurance. Managed care was entered as weak, strong, or no management.
Results
Diagnoses
At baseline, 1,642 respondents met criteria for one or more disorders. A total of 1,148 respondents had a primary diagnosis of major depression, 175 had dysthymia, 172 had panic disorder, and 147 had generalized anxiety disorder. A total of 1,092 respondents were interviewed again at follow-up, for a response rate of 67%. The mean interval between interviews was 32±4 months. At follow-up, 626 respondents no longer met criteria for a disorder. Of the 466 with a probable disorder, 342 had major depression, 46 had dysthymia, 44 had panic disorder, and 34 had generalized anxiety disorder. A total of 154 had a different primary diagnosis at follow-up than at baseline.
For subsequent analyses, data were weighted so that proportions would apply to the U.S. adult population. Weights were developed for each respondent based on the probability of selection from the CTS sample and of nonresponse to the telephone survey. After weighting, analyses estimated that 4.7% of the U.S. population had a disorder at both baseline and follow-up (95% confidence interval [CI]=4.1%–5.2%). When categorized by baseline disorder, 3.4% of the population had persistent major depression (CI=2.9%–3.9%), .6% had persistent dysthymia (CI=.4%–.8%), and .7% had persistent generalized anxiety or panic disorder (CI=.5%–.9%).
At follow-up, 59% no longer met criteria for a disorder. Table 1 presents baseline characteristics of the population that recovered and the population that continued to be ill at follow-up. Individuals with persistent illness were significantly more likely to be female, have lower family income, and have lower physical and mental health scale scores. They were also more likely to have chronic medical disorders, suicidal ideation, and a lifetime history of treatment for depression or anxiety.
 |
Clinician visits and treatment use
Treatment use was studied during one-year periods before baseline and follow-up ( Table 2 ). Primary care visits were common, with 84% having at least one visit (CI=81%–87%). Rates of primary care use did not differ in the group that remained persistently ill, nor did the rate change at follow-up. Specialty mental health visits were much less common. At baseline, specialists were seen by 19% of the population that recovered (CI=14%–24%) and 25% of the population that remained persistently ill (CI=19%–32%). Over time, specialty care decreased markedly in the group that recovered but did not change among those who remained ill. Among those who were ill at baseline, 37% recovered with no treatment.
 |
At baseline, only 30% of people with a disorder received appropriate medication or counseling (CI=28%–33%). Twenty-six percent of those who recovered received either appropriate medication or counseling (CI=20%–31%), compared with 35% of those with persistent illness (CI=28%–41%). Over time, the proportion of people receiving medication treatment increased in the population with persistent illness (from 21% to 29%; p=.003), but use of counseling did not increase.
Treatment use at follow-up was then examined for people with persistent illness. Forty-two percent of those with major depression received either appropriate medication or counseling, compared with 30% of those with dysthymia and 22% of those with generalized anxiety disorder or panic disorder (the two diagnostic groups were merged for the analysis). Only 12% of individuals with persistent illness received both appropriate medication and counseling at follow-up. The multivariate model indicated that individuals with persistent illness were significantly less likely to receive appropriate medications and counseling if they had less than a high school education ( Table 3 ). They were more likely to report appropriate counseling if they were female or had suicidal ideation and more likely to report appropriate medication if they had an alcohol or drug problem. Family income and medical insurance had no overall effect on receipt of treatment. However, private insurance that did not involve managed care was associated with greater use of appropriate counseling, and Medicaid was associated with greater use of appropriate medication.
 |
Morbidity
In the population with persistent illness, morbidity at follow-up was substantial and significantly worse than in the population that recovered ( Table 4 ). Quality of life was one standard deviation below the norm for the general population. Satisfaction with care was lower. Rates of unemployment were significantly higher among individuals with persistent illness than among those who recovered (21% compared with 10%; p<.05). Notably, 51% of those in the persistently ill group reported having suicidal ideation (CI=46%–56%), compared with 9% of those who recovered (250 respondents compared with 54; F=87.5, df=1 and 296, p<.001).
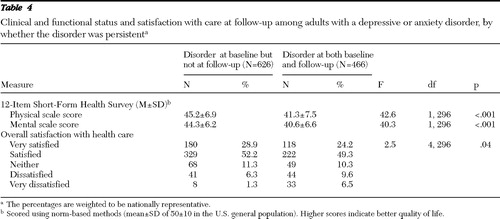 |
To better understand the high level of suicidal ideation in the population with persistent illness, we compared the groups with (N=250) and without (N=214) suicidal ideation at follow-up. No significant difference (at p<.05) was found in substance misuse, number of chronic medical disorders, or insurance type. The population with suicidal ideation had more life difficulties (1.2 compared with .9; F=6.2, df=1 and 146, p=.014) and lower quality of life (mental scale score of 39.6 compared with 41.6; F=5.9, df=1 and 146, p=.02).
Discussion
This is the first study to provide national estimates of treatment use and quality of care for people with persistent anxiety and depressive disorders. As such, it provides critical new information regarding problems in care for this population and can inform policy to improve health care. People with persistent anxiety and depressive disorders are a vulnerable population, and there are pervasive problems with the care they receive. Because many people with persistent anxiety and depressive disorders do not receive treatment, it has previously been difficult to estimate how large this population is and how often they use psychotherapy or medication treatments. This study characterized the population with persistent anxiety and depressive disorders by using community-based sampling combined with tracking of individuals over time.
Persistent depression and anxiety are common and associated with substantial reductions in quality of life and high rates of suicidal ideation. As has been found in cross-sectional research, this study found that about one-third of people with a depressive or anxiety disorder received treatment. When individuals with a probable disorder were reinterviewed about two-and-a-half years later, 57% no longer met criteria for a psychiatric disorder. As expected, treatment utilization declined markedly in this recovered group. Surprisingly, however, within the group that remained ill there was only a modest increase in use of medication and no increase in use of counseling. In controlled trials, evidence-based psychotherapy and medication markedly improve outcomes in persistent illness, and the combination of these two treatments appears to be more effective than either treatment alone ( 3 ). In the general U.S. population, however, treatment rates remain low, and combined medication and counseling is rare. It appears that there is a low, relatively fixed level of treatment provided to people with psychiatric problems, and the care provided responds minimally or not at all to persistent or high levels of need. This response is certainly less than one would expect given the urgency, illness severity, and known impact of these disorders.
Persistent depressive and anxiety disorders pose unique challenges to clinicians and health care organizations and particularly difficult challenges in primary care. Organizational interventions are available that improve outcomes in persistent psychiatric illness by enhancing access to evidence-based medication and psychotherapy. In older adults, controlled trials have demonstrated that making treatment available improves depression and reduces suicidal ideation ( 41 ). In primary care populations, stepped care models improve outcomes of people with persistent illness ( 24 , 42 ). These models begin with detection and treatment in primary care, but they also include clearly defined roles for mental health specialists and increased treatment intensity when disorders persist over time.
Efforts to broadly improve quality will need to attend to the persistent, low level of psychotherapy utilization. Evidence-based psychotherapies have consistently been shown to improve outcomes ( 43 ). We defined appropriate counseling broadly, including as little as four sessions, and were not able to identify whether counseling was evidence based. During a one-year period, only 19% of persistently ill individuals received counseling four or more times. Therefore, the rate of evidence-based psychotherapy is likely to be very low. This is remarkable, given that many patients state a preference for psychotherapy over medications ( 44 ). Education is needed to inform clinicians and the public regarding the effectiveness of psychotherapy and to ensure that clinicians are competent to provide evidence-based psychotherapies.
Persistent illness was found to be more common among women, those with lower income, and those with concurrent medical illness. With regard to treatment use, we found that men were less likely to use counseling and that people with less than a high school education were less likely to use either counseling or medication. These disparities are similar to those found in previous research on acute psychiatric illness and suggest that efforts to reduce disparities should also attend to persistent illness. We also found that private insurance that did not involve managed care and Medicaid were associated with greater access to appropriate counseling and medication, respectively. It should be possible to increase use of appropriate treatment by improving insurance arrangements.
The generalizability and policy relevance of this study are enhanced by the inclusion of common, treatable depressive and anxiety disorders and by the use of community-based sampling. This study included a large number of individuals who received no treatment. This finding underscores the relevance of results for policy makers and organizations responsible for improving the health care of large populations. However, this study's methods also resulted in important limitations. For one, some individuals did not respond to the baseline and follow-up surveys. To address this, we weighted for nonresponse in our analyses and compared the demographic characteristics of responders and nonresponders. Although nonresponse may have affected our results somewhat, our results are consistent with cross-sectional national surveys, suggesting that the effect of nonresponse may not have been large.
Also, we identified illnesses by screening methods rather than by a clinical interview. Researchers have compared a similar brief diagnostic assessment with a structured, clinical assessment and have found that the brief assessment is highly specific and moderately sensitive ( 45 ). Therefore, one would expect that most of the people we identified had, in fact, a depressive or anxiety disorder. In addition, we do not know the illness status of respondents between the two surveys. The population identified as having persistent illness is likely to have included both individuals with continuous illness and individuals who recovered and later relapsed. In either case, our interviews were separated by about two-and-a-half years, and most people in the group with persistent illness are likely to have a long-term illness course.
Conclusions
Persistent depressive and anxiety disorders are remarkably common in the U.S. population and are associated with substantial morbidity. There are significant problems with the quality of care received by this population, and these problems persist over time. Improving the treatment of people with persistent depressive and anxiety disorders may require changes in policy and services, including support for care models that systematically increase treatment intensity when patients do not respond to initial treatment. Most people with persistent depressive and anxiety disorders are seen in primary care, and this is a promising location to engage them in treatment. However, rates of appropriate medication treatment and counseling are much lower in primary care than in specialty care ( 16 ). Improving care will require greater collaboration between primary care practitioners and mental health specialists and increased use of specialists by people with persistent or treatment-resistant illness. Intervention research in depression has demonstrated that the largest improvements in outcomes occur when care is brought to the most disadvantaged populations ( 46 ). In the population with persistent depressive and anxiety disorders, increasing the rate of appropriate care from its current low level could result in substantial improvement in individuals' lives.
Acknowledgments and disclosures
This study was supported by grant 038273 from the Robert Wood Johnson Foundation, grant P30-MH068639 from the National Institute of Mental Health, and by the Department of Veterans Affairs, Los Angeles. The Robert Wood Johnson Foundation approved the design and conduct of the study. However, sponsors had no other role in study conduct or data collection, management, analysis, or interpretation. Sponsors had no role in manuscript preparation, review, or approval. The authors thank Lily Zhang, M.S., for data analysis. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of any affiliated institutions.
The authors report no competing interests.
1. Achieving the Promise: Transforming Mental Health Care in America. Pub no SMA-03-3832. Rockville, Md, Department of Health and Human Services, President's New Freedom Commission on Mental Health, 2003Google Scholar
2. Greenberg PE, Kessler RC, Birnbaum HG, et al: The economic burden of depression in the United States: how did it change between 1990 and 2000? Journal of Clinical Psychiatry 64:1465–1475, 2003Google Scholar
3. Keller MB, McCullough JP, Klein DN, et al: A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. New England Journal of Medicine 342:1462–1470, 2000Google Scholar
4. Spijker J, de Graaf R, Bijl RV, et al: Duration of major depressive episodes in the general population: results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). British Journal of Psychiatry 181:208–213, 2002Google Scholar
5. Klein DN, Schwartz JE, Rose S, et al: Five-year course and outcome of dysthymic disorder: a prospective, naturalistic follow-up study. American Journal of Psychiatry 157: 931–939, 2000Google Scholar
6. Schweizer E, Rickels K: The long-term management of generalized anxiety disorder: issues and dilemmas. Journal of Clinical Psychiatry 57(suppl 7):9–12, 1996Google Scholar
7. American Psychiatric Association: Practice guideline for the treatment of patients with major depressive disorder (revision). American Journal of Psychiatry 157:1–49, 2000Google Scholar
8. American Psychiatric Association: Practice guideline for the treatment of patients with panic disorder. American Journal of Psychiatry 155:1–34, 1998Google Scholar
9. Pollack MH, Allgulander C, Bandelow B, et al: WCA recommendations for the long-term treatment of panic disorder. CNS Spectrums 8:17–30, 2003Google Scholar
10. Allgulander C, Bandelow B, Hollander E, et al: WCA recommendations for the long-term treatment of generalized anxiety disorder. CNS Spectrums 8:53–61, 2003Google Scholar
11. Barlow DH, Lehman CL: Advances in the psychosocial treatment of anxiety disorders: implications for national health care. Archives of General Psychiatry 53:727–735, 1996Google Scholar
12. Kessler RC, Demler O, Frank RG, et al: Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine 352:2515–2523, 2005Google Scholar
13. Narrow WE, Rae DS, Robins LN, et al: Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys' estimates. Archives of General Psychiatry 59:115–123, 2002Google Scholar
14. Olfson M, Marcus SC, Wan GJ, et al: National trends in the outpatient treatment of anxiety disorders. Journal of Clinical Psychiatry 65:1166–1173, 2004Google Scholar
15. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:203–209, 2002Google Scholar
16. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55–61, 2001Google Scholar
17. Blazer DG, Hughes D, George LK: Generalized anxiety disorder, in Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. Edited by Robins LN, Regier DA. New York, Free Press, 1991Google Scholar
18. Eaton WW, Anthony JC, Gallo J, et al: Natural history of Diagnostic Interview Schedule/DSM-IV major depression: The Baltimore Epidemiologic Catchment Area follow-up. Archives of General Psychiatry 54:993–999, 1997Google Scholar
19. Kessler RC, Merikangas KR, Berglund P, et al: Mild disorders should not be eliminated from the DSM-V. Archives of General Psychiatry 60:1117–1122, 2003Google Scholar
20. Furukawa TA, Kitamura T, Takahashi K: Time to recovery of an inception cohort with hitherto untreated unipolar major depressive episodes. British Journal of Psychiatry 177:331–335, 2000Google Scholar
21. Bech P, Lucas R, Amir M, et al: Association between clinically depressed subgroups, type of treatment and patient retention in the LIDO study. Psychological Medicine 33: 1051–1059, 2003Google Scholar
22. Schoenbaum M, Unützer J, McCaffrey D, et al: The effects of primary care depression treatment on patients' clinical status and employment. Health Services Research 37: 1145–1158, 2002Google Scholar
23. Fava M, Rush AJ, Wisniewski SR, et al: A comparison of mirtazapine and nortriptyline following two consecutive failed medication treatments for depressed outpatients: a STAR*D report. American Journal of Psychiatry 163:1161–1172, 2006Google Scholar
24. Katon W, Von Korff M, Lin E, et al: Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Archives of General Psychiatry 56:1109–1115, 1999Google Scholar
25. Roy-Byrne PP, Katon W, Cowley DS, et al: A randomized effectiveness trial of collaborative care for patients with panic disorder in primary care. Archives of General Psychiatry 58:869–876, 2001Google Scholar
26. Sturm R, Gresenz C, Sherbourne C, et al: The design of Healthcare for Communities: a study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry 36:221–233, 1999Google Scholar
27. Kemper P, Blumenthal D, Corrigan JM, et al: The design of the community tracking study: a longitudinal study of health system change and its effects on people. Inquiry 33:195–206, 1996Google Scholar
28. Ware J Jr, Kosinski M, Keller SD: A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care 34:220–233, 1996Google Scholar
29. Stockdale SE, Klap R, Belin TR, et al: Longitudinal patterns of alcohol, drug, and mental health need and care in a national sample of US adults. Psychiatric Services 57:93–99, 2006Google Scholar
30. Kessler RC, Andrews G, Mroczek D, et al: The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). Geneva, World Health Organization, 1998Google Scholar
31. Composite International Diagnostic Interview (CIDI), version 2.1. Geneva, World Health Organization, 1997Google Scholar
32. Bergner M: The Sickness Impact Profile (SIP), in Assessment of Quality of Life in Clinical Trials of Cardiovascular Therapies. Edited by Wenger NK, Mattson ME, Furberg CD, et al. New York, Le Jacq Publishing, 1984Google Scholar
33. World Health Organization: The Alcohol Use Disorders Identification Test (AUDIT): Guidelines for Use in Primary Health Care. Geneva, World Health Organization, 1992Google Scholar
34. Wells KB: The design of Partners in Care: evaluating the cost-effectiveness of improving care for depression in primary care. Social Psychiatry and Psychiatric Epidemiology 34: 20–29, 1999Google Scholar
35. Sturm R, Sherbourne CD: Managed care and unmet need for mental health and substance abuse care in 1998. Psychiatric Services 51: 177, 2000Google Scholar
36. Depression Guideline Panel: Depression in Primary Care: Treatment of Major Depression. Rockville, Md, Agency for Health Care Policy and Research, 1993Google Scholar
37. Roy-Byrne P, Stein M, Bystrisky A, et al: Pharmacotherapy of panic disorder: proposed guidelines for the family physician. Journal of the American Board of Family Practice 11:282–290, 1998Google Scholar
38. Sturm R, Wells KB: How can care for depression become more cost-effective? JAMA 273:51–58, 1995Google Scholar
39. SUDAAN: Professional Software for Survey Data Analysis, Version 7.5. Research Triangle Park, NC, Research Triangle Institute, 1997Google Scholar
40. Koch GG, Freeman DH, Freeman JL: Strategies in the multivariate analysis of data from complex surveys. International Statistical Review 43:59–78, 1975Google Scholar
41. Bruce ML, Ten Have TR, Reynolds CF III, et al: Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA 291:1081–1091, 2004Google Scholar
42. Lin EH, VonKorff M, Russo J, et al: Can depression treatment in primary care reduce disability? A stepped care approach. Archives of Family Medicine 9:1052–1058, 2000Google Scholar
43. Schoenbaum M, Unützer J, Sherbourne C, et al: Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA 286:1325–1330, 2001Google Scholar
44. Dwight-Johnson M, Sherbourne CD, Liao D, et al: Treatment preferences among depressed primary care patients. Journal of General Internal Medicine 15:527–534, 2000Google Scholar
45. Murphy JM, Monson RR, Laird NM, et al: A comparison of diagnostic interviews for depression in the Stirling County study: challenges for psychiatric epidemiology. Archives of General Psychiatry 57:230–236, 2000Google Scholar
46. Wells K, Sherbourne C, Schoenbaum M, et al: Five-year impact of quality improvement for depression: results of a group-level randomized controlled trial. Archives of General Psychiatry 61:378–386, 2004Google Scholar



