Improving Medication Management of Depression in Health Plans
Improving depression treatment is critical given the low rates of appropriate care for this common and treatable disorder. About 17% of the population will have a major depressive disorder during their lifetime ( 1 ), and 7% of the population has had such a disorder in the past year ( 2 ). Deficiencies in depression care, especially in primary care, are well documented ( 3 , 4 , 5 , 6 ). Among persons with depression in the past year, only half received any treatment for it, and only 38% of those who received any care got at least minimally adequate treatment ( 3 ). An analysis of quality of care in the United States found that adults treated for depression received 58% of recommended care processes ( 5 ).
One approach to influencing care is the use of performance measures for accountability, comparison, and quality improvement purposes ( 7 ). Since 1999 the National Committee for Quality Assurance (NCQA) has tracked and reported on depression care in health plans, primarily health maintenance organizations (HMOs) and point-of-service (POS) plans, using a three-component antidepressant medication management (AMM) measure for patients with a diagnosis of major depression who are prescribed antidepressants. In contrast to measures for medical conditions such as diabetes, AMM measures have shown little improvement over time, stagnating at suboptimal levels, with rates from one-fifth to just over half depending on the measure ( 6 ).
Studies addressing improvement in depression treatment at the practice level show promising results ( 8 ). Other studies have addressed the connection between particular plan features, such as behavioral health carve-outs, and depression treatment ( 9 , 10 ). Plans influence quality independently from provider groups ( 11 ), and significant variation exists in plan structure, behavioral health contracting, and quality improvement efforts that could affect treatment ( 12 ). However, little is known about the relationship between a range of organizational features and performance in depression treatment. Our results have implications for improving depression care by identifying actionable health plan factors that influence performance, informing plans and purchasers about ways to improve quality and facilitating value-based purchasing.
Methods
Data on health plan characteristics and practices for this study were from the Brandeis Survey on Alcohol, Drug Abuse, and Mental Health Services, a survey of 441 market area-specific private plans regarding mental health and substance abuse services in 2003. The response rate was 83% (N=368). The survey was a follow-on to a survey conducted in 1999. The telephone survey in 2003 included an administrative module addressing behavioral health contracting, benefits, network management, and provider payment and a clinical module addressing primary care screening and treatment, entry into specialty care, utilization management, prescription drug formularies, quality improvement, and other clinically oriented topics. Each plan was asked about its top three commercial managed care products. Items were asked at the product level within each market area-specific plan.
Typically, the executive director for the administrative module and medical director for the clinical module were able to respond to all topics in the survey, although some plans referred to the managed behavioral health organization (MBHO) for some information. For some national or regional plans, respondents at the corporate headquarters-level were interviewed regarding multiple sites. We found heterogeneity in plan operation among health plans with a presence in multiple market areas. For example, in some cases corporate-level respondents reported variation across markets, and in some other cases they directed us to contact market-level staff. In all cases we gathered information pertaining specifically to the market area. Active informed consent was obtained from each respondent, and the study was approved by the Brandeis University Institutional Review Board. Respondents were informed that their identities and those of the health plans they represented would remain confidential and that all data would be presented only in aggregate fashion.
The study is linked to the Community Tracking Study (CTS), a longitudinal study of health system change funded by the Robert Wood Johnson Foundation ( 13 ). The primary sampling units were the 60 CTS market areas selected to be nationally representative. The second stage consisted of selecting plans within market areas. Plans serving multiple markets were defined as separate plans for the study, and data were collected with reference to the specific market.
The 2003 sample included all of the 1999 sample plus a national sample of plans not previously operating in the sites. There were 441 eligible plans, of which 368 (83%) responded and reported on 812 products. Nonresponse analysis examined differences in terms of region and plan type; responding plans were more likely to offer HMO products.
We linked health plan survey data with antidepressant medication management data from NCQA's Health Plan Employer Data and Information Set (HEDIS) and plans' self-reported data on model type. The sample included 361 HMO and POS products representing 183 plans.
The goal of the HEDIS AMM measure is to monitor the degree to which plan members who receive a diagnosis of a new episode of major depression and who are treated with antidepressants receive effective treatment. The first two components focus on antidepressant prescribing during acute and continuation phases, and the third focuses on follow-up visit frequency. The specifications are generally concordant with treatment guidelines, such as those of the American Psychiatric Association ( 14 ), although HEDIS requires less frequent follow-up. Rather than determining phase of treatment according to the individual's condition, HEDIS uses number of weeks since the index prescription. Using time since initiation is a common approach to operationalizing treatment phase in administrative data. Each component of the measure is a dependent variable in our analyses.
Independent variables that may be related to the quality of depression treatment were categorized into organizational, provider, and consumer domains. The organizational domain included whether plans carve out mental health services, use depression disease management programs, and require mental health specialists to contact primary care physicians given patients' permission. The provider domain included whether the plan distributes written guidelines and provides related training, gives feedback to providers regarding their own performance relative to guidelines, and gives providers feedback regarding overall performance of the network. We also included whether, beyond medication management, plans allow primary care physicians to bill using other psychiatric procedure codes, such as for psychotherapy.
The consumer domain included cost sharing for outpatient mental health visits. Coinsurance exceeding 20% or copayments exceeding $20 were considered "high." We included whether plans allowed access to outpatient mental health care without gatekeeping or prior authorization. Finally, we examined how many of the four newer selective serotonin reuptake inhibitors (SSRIs) (sertraline, paroxetine, citalopram, and escitalopram), as of 2003, were available on tier 2 of the formulary without requirements for prior authorization or for first failing treatment with another drug. Copayments are typically lowest for generic drugs (tier 1), higher for brand drugs "preferred" by the plan (tier 2), and highest for "nonpreferred" brands (tier 3).
Multivariate analyses were conducted by using ordinary least squares regression to determine how organizational, provider, and consumer factors were related to plan performance on each component of the AMM measure. Analyses were conducted at the insurance product level by using SUDAAN for sampling variance estimation. The dependent variable in each case is the product-level rate for that HEDIS measure, expressed as a percentage of eligible members whose care met criteria on the measure. Thus the coefficients in each regression model represent differences in the HEDIS rates associated with each independent variable, relative to the reference group and with other variables held constant. We also conducted sensitivity analyses to examine the potential effect of larger, multimarket health plans. When we included dummy variables for the largest such plans, results for all three dependent variables were very similar to the original models in terms of significance and directionality of independent variable coefficients. Therefore, we present the models without these controls.
Results
Sample description
Table 1 describes sample characteristics. In the organizational domain, 29% of products used physician groups or networks, 27% were independent practice associations, and 44% had a mixed approach. About 78% of products were offered by for-profit plans. Eighty-one percent contracted with a MBHO. Products were geographically dispersed and varied widely in terms of enrollment. Depression disease management was used by 48% of products, and 84% required specialty behavioral health providers to contact primary care physicians with the patient's permission.
 |
Within the provider domain, 76% provided training on depression guidelines, 37% provided individual feedback to providers regarding their own performance, and 21% provided feedback regarding overall network performance.
Within the consumer domain, 32% of products had high cost sharing for outpatient mental health. Direct access to mental health care was available in 39% of products. Most products had three-tier formularies, and on average three of the newer SSRIs were available on tier 2 without restriction.
Overall performance on HEDIS AMM measures
Table 2 presents definitions and overall performance scores on HEDIS AMM measures. On average, 60% of plan members who were started on antidepressants for a new episode of depression remained on antidepressants during the acute phase, 43% continued antidepressants during the continuation phase, and 22% received optimal practitioner contact. These figures are comparable to the rates for all private plans participating in HEDIS in 2003 ( 15 ).
 |
Performance across measures
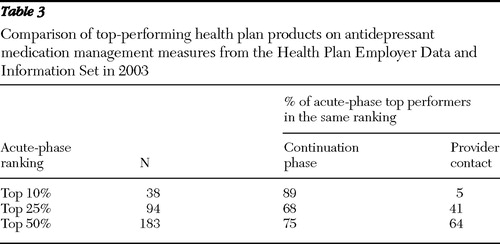
Table 3 provides a comparison of top-performing products across the three components of the AMM measure. The top 10% of products were relatively consistent for acute- and continuation-phase components; 89% of the products that ranked in the top 10% for the acute phase also were in the top 10% for the continuation phase. However, some variability was noted among the top 25% of products on these two measures. Among products ranking in the top 25% for the acute phase, 68% were also in the top 25% for the continuation phase. The provider contact component was dramatically different from the acute-phase component, with only 5% of the products that ranked in the top 10% for the acute phase also ranking in the top 10% for the provider contact component of the AMM measure.
 |
Association between plan characteristics and performance
Organizational domain. Multivariate analyses indicated that when other factors were controlled for, performance rates among plans that carved out mental health were higher on the acute and continuation measures ( Table 4 ). Having a depression disease management program was also associated with better performance on these measures. Neither factor was significantly related to the provider contact measure. Requiring specialty providers to contact primary care physicians was consistently associated with lower performance across all measures.
 |
Plans with group or network models were associated with significantly better performance on the continuation-phase measure and provider contact measure. Independent practice association models were associated with better performance on the provider contact measure. For-profit status was associated with better performance on the continuation-phase measure but lower performance on provider contact. Northeast region was a predictor of better performance on all measures. Volume of enrollment was not consistently related to performance.
Provider domain. When the analysis controlled for other factors, providing training on depression guidelines was associated with a lower rate of optimal provider contact. Providing individual feedback to providers regarding their performance was associated with higher performance rates for all measures. Feedback regarding overall performance of the network and allowing primary care physicians to bill for psychiatric treatment other than medication management was associated with significantly lower performance scores on the contact measure.
Consumer domain. Multivariate analyses showed a significant inverse association between cost sharing for mental health visits and performance on the acute- and continuation-phase measures. No significant association was found between cost sharing and optimal provider contact rates. Offering more of the newer SSRIs on tier 2 was associated with better performance during the acute and continuation phases of treatment but lower rates of optimal provider contact. After other factors were controlled for, performance on the provider contact measure was higher in plans that allowed direct access.
Discussion
A number of factors, including the high prevalence of depression, the recent push to increase screening for depression in primary care ( 16 ), and health plans' relatively poor past performance on depression quality measures, necessitate improvement in the quality of depression treatment. Our results indicate that there are tools and structures that health plans may be able to use to improve depression care.
Individual feedback on performance relative to practice guidelines was positively related to performance on the HEDIS AMM measures. Our study could not determine whether feedback caused better performance; however, it appears to be a powerful tool in influencing provider behavior. This indicates that providers are responsive to efforts to help them improve performance and that such feedback is an actionable technique for health plans to use to influence performance. We do not know how feedback was provided; this is an important consideration because research shows that not all feedback tools are effective ( 17 ). This finding suggests that providers may also be responsive to other direct efforts by health plans to recognize or reward performance.
Cost sharing for mental health visits appears to be another important mechanism influencing rates of acute- and continuation-phase medication management. Higher cost sharing was associated with lower performance on both of these measures. Increased access to SSRIs was associated with higher rates of effective medication management during both phases of treatment. These findings suggest that financial barriers may prevent patients from receiving high-quality health care, adding to existing research that shows an inverse relationship between cost sharing and utilization of mental health services ( 18 , 19 ). The reduction of financial barriers to mental health care is an action that employers and other purchasers can undertake to improve quality of care when selecting benefit features.
Plans that contract with MBHOs had higher rates of effective acute- and continuation-phase antidepressant medication management on this HEDIS measure. This may be because plans that carve out are more likely to have patients in specialty treatment where providers are more likely to meet HEDIS standards ( 20 ).
At the same time, some results were counterintuitive—for example, the negative relationships between performance measures and requiring specialty providers to contact primary care physicians and allowing primary care physicians to bill for psychiatric procedures other than medication management. One possibility is that plans that allow expanded mental health billing may have more depression treatment occurring in primary care, where treatment may be less likely to meet measure criteria. These findings require further exploration, and future research should focus on the mechanisms underlying these associations.
The provider contact measure seems to be driven by factors different from those that drive the medication measures. This is supported by our analysis of top-performing products across the three components of the AMM measure. There were also more counterintuitive results for the provider contact measure. NCQA is currently reconsidering the definition of this measure. NCQA began allowing telephone contact with providers to count toward the visit measure in 2004 and is currently considering including case management and disease management contacts in the provider contact count. Our results indicate these may be reasonable changes, although it is not clear how they will affect performance. Plans with depression disease management had a significantly higher proportion of members receiving effective medication management during the acute and continuation phases, but this is not currently captured in the provider contact measure.
The study has some limitations. The sample is limited to plans included in both the health plan survey and the NCQA HEDIS database. Preferred-provider organization products were not included because they generally did not participate in HEDIS before 2006. As noted above, this study analyzed associations between health plan characteristics and HEDIS performance, but causality could not be determined given our observational research design. This analysis captures one aspect of depression care—namely, treatment with antidepressants—and is limited to new episodes. Analyses were conducted at the organizational level, and we could not assess the quality of care received by individual patients, severity, outcomes, or reasons for discontinuation. Patients may have received prescriptions for antidepressants but may not have filled them, or they may not have taken medications they did get. Providers may have given medication samples, but this seems unlikely to be a significant issue because samples are normally used for a short time until a prescription can be filled.
Conclusions
Our study found that health plan features had a significant relationship to performance on HEDIS AMM measures. Some efforts to improve performance, such as providing individual provider feedback and depression disease management programs, appear to have positive results. Many of the features we identified suggest actionable ways for plans to improve quality of care for depression.
Acknowledgments and disclosures
Funding for this study was provided by grant 051651 from the Robert Wood Johnson Foundation Depression in Primary Care Initiative, grant R01-DA-10915 from the National Institute on Drug Abuse, and grant R01-AA-20869 from the National Institute on Alcohol Abuse and Alcoholism. The authors thank Grant Ritter, Ph.D., for statistical consultation; Dominic Hodgkin, Ph.D., and Deborah Garnick, Sc.D., for helpful comments; Galina Zolotusky, M.S., for statistical programming; and Joanna Volpe-Vartanian, Ph.D., L.I.C.S.W., for research assistance.
The authors report no competing interests.
1. Kessler RC, Berglund P, Demler O, et al: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:593–602, 2005Google Scholar
2. Kessler RC, Chiu WT, Demler O, et al: Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:617–627, 2005Google Scholar
3. Wang PS, Lane M, Olfson M, et al: Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry 62:629–640, 2005Google Scholar
4. Young A, Klap R, Sherbourne C, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55–61, 2001Google Scholar
5. McGlynn EA, Asch SM, Adams J, et al: The quality of health care delivered to adults in the United States. New England Journal of Medicine 348:2635–2645, 2003Google Scholar
6. The State of Health Care Quality, 2005. Washington, DC, National Committee for Quality Assurance, 2005Google Scholar
7. Horgan CM, Garnick DW: The Quality of Care for Adults With Mental and Addictive Disorders: Issues in Performance Measurement. Report for the Institute of Medicine, Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Washington, DC, Institute of Medicine, 2005Google Scholar
8. Wells K, Sherbourne C, Schoenbaum M, et al: Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA 283:212–220, 2000Google Scholar
9. Merrick EL: Effects of a behavioral health carve-out on inpatient-related quality indicators for major depression treatment. Medical Care 37:1023–1033, 1999Google Scholar
10. Busch S: Specialty health care, treatment patterns, and quality: the impact of a mental health carve-out on care for depression. Health Services Research 37:1583–1601, 2002Google Scholar
11. Baker LC, Hopkins D, Dixon R, et al: Do health plans influence quality of care? International Journal for Quality in Health Care 16:19–30, 2004Google Scholar
12. Horgan CM, Merrick EL, Garnick DW, et al: The Provision of Mental Health Services in Managed Care Organizations. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2003Google Scholar
13. Kemper P, Blumenthal D, Corrigan JM, et al: the design of the Community Tracking Study: a longitudinal study of health system change and its effects on people. Inquiry 33:195–206, 1996Google Scholar
14. Karasu TB, Gelenberg A, Merriam A, et al: Practice guideline for the treatment of patients with major depressive disorder. American Journal of Psychiatry 157(Apr suppl):1–45, 2000Google Scholar
15. State of Health Care Quality Report, 2003. Washington, DC, National Committee for Quality Assurance, 2004Google Scholar
16. US Preventive Services Task Force: Screening for depression: recommendations and rationale. Annals of Internal Medicine 136:760–764, 2002Google Scholar
17. Bambauer K, Adams A, Zhang F, et al: Physician alerts to increase antidepressant adherence: fax or fiction? Archives of Internal Medicine 166:498–504, 2006Google Scholar
18. Lindrooth R, Lo Sasso A, Lurie I: The effect of expanded mental health benefits on treatment initiation and specialist utilization. Health Services Research 40:1092–1107, 2005Google Scholar
19. Simon G, Grothaus L, Durham M, et al: Impact of visit copayments on outpatient mental health utilization by members of a health maintenance organization. American Journal of Psychiatry 153:331–338, 1996Google Scholar
20. Robinson R, Long S, Change S, et al: Higher costs and therapeutic factors associated with adherence to NCQA HEDIS antidepressant medication management measures: analysis of administrative claims. Journal of Managed Care Pharmacy 12:43–54, 2006Google Scholar



