Correlates of Mental Health Service Use Intensity in the National Comorbidity Survey and National Comorbidity Survey Replication
Numerous national studies have linked sociodemographic and mental illness variables with use of mental health care ( 1 , 2 , 3 ). However, the intensity of treatment use (that is, visit counts) has not been adequately studied, nor has it been analyzed by appropriate statistical methods given the large numbers of nonusers. Thus, despite our sophisticated understanding of what predicts initial treatment use, few data exist on correlates of continuing use of mental health care.
Recent large-scale studies demonstrate several variables associated with an increased likelihood of mental health care use. These variables can be considered within a well-validated theoretical framework, Andersen's behavioral model of health care use ( 4 ). Significant sociodemographic variables (or predisposing factors in the behavioral model of health care use) include female gender ( 2 , 5 , 6 , 7 ), younger age ( 3 , 8 ), Caucasian race ( 2 , 3 , 7 ), and higher education ( 3 , 6 ). Significant access variables (or enabling factors in the behavioral model of health care use) include unemployment ( 5 ), urban residence ( 2 ), and health insurance coverage ( 9 ). Finally, significant illness variables (or need factors in the behavioral model of health care use) include mood disorders ( 3 , 6 ), substance use disorders ( 3 , 6 ), and anxiety disorders ( 3 , 6 , 10 ); also included as significant illness variables are mental health disability and perceived need for treatment, although these have been demonstrated to have weaker effects ( 11 ). It should be noted that some research has demonstrated that needs variables evidence stronger effects than sociodemographic variables and access variables ( 5 , 12 , 13 ).
Despite previous research on correlates of mental health care use, few investigations have examined treatment use intensity (visit counts), a more dynamic indicator of disease burden. Three studies that used data from the 1990–1992 National Comorbidity Survey (NCS) examined associations between psychiatric status and treatment visit counts ( 10 , 14 , 15 ), but these studies used general linear model analyses. This approach violates analytic assumptions based on visit counts' substantially skewed distributions with excessive zero values ( 16 ), posing serious analytic consequences—for example, mistakenly finding statistical significance (also known as type I error) ( 17 , 18 ). Statistical methods were not available to address this problem until recently ( 19 , 20 , 21 ).
The study presented here aimed to examine associations between needs variables and intensity of mental health care use. We statistically controlled for the effects of sociodemographic and access variables ( 4 ) because these variables may affect mental health care use. We hypothesized that when appropriate analyses were used, presence of a mental illness (that is, objective need) would be most strongly associated with treatment use intensity ( 5 , 12 , 13 ).
To test this hypothesis we first conducted univariate analyses to examine the relationship between service use intensity and several potential correlates of service use: sociodemographic factors (age, education, gender, and race), access factors (presence of health insurance, employment status, and residence [urban or rural]), and need factors (psychiatric diagnoses, psychiatric disability, and perceived need). Results of univariate analyses were compared with multivariate results, assessing the extent to which needs factors contribute to treatment use intensity above and beyond sociodemographic and access factors. Because our analytic plan gathered information from the NCS (1990–1992) and the NCS Replication (NCS-R) (2001–2003), it had the additional advantage of comparing treatment use correlates across two time cohorts. Our study design also had the advantage of gathering data on the delivery of mental health care from three service system sectors (mental health, social services, and medical). Thus we were able to identify both time-specific and sector-specific relationships between the need for services and use of services, as well as relationships that were consistent across time and service sectors. This approach provides a basis for relatively strong inferences to test Andersen's ( 4 ) model, with a focus on delineating the unique relationship between need and actual use of mental health services.
Methods
Sample
The NCS ( 22 ) and NCS-R ( 23 ) consist of nationally stratified, multistage area household probability samples of noninstitutionalized persons (ages 15–54 for the NCS and ages 15 or older for the NCS-R) that investigated sociodemographic characteristics and mental health status. The NCS was conducted with more than 8,000 participants (1990–1992). The NCS-R was conducted with more than 9,000 participants (2001–2003). The article presented here reports on the subsample of participants, ages 15–54, who completed parts I and II of the NCS (N=5,877) or who completed parts I and II of the NCS-R (N=4,320). Both surveys screened for mental disorders and service use. Informed consent and institutional review board approval were obtained.
Instruments
Sociodemographic characteristics. The NCS and NCS-R queried respondents about their gender, racial and ethnic background, age, education, employment status, geographical residence, and health insurance possession.
Diagnostic assessment. A modified version of the structured Composite International Diagnostic Interview (CIDI) ( 24 ) has been shown to possess adequate psychometric properties ( 25 , 26 ) and was used to diagnose DSM-III-R mental disorders on the NCS and DSM-IV mental disorders on the NCS-R. We collapsed variables into the following relatively high-prevalence past-year disorder categories: any anxiety disorder (panic disorder, agoraphobia with or without panic disorder, social phobia, simple phobia, generalized anxiety disorder, and posttraumatic stress disorder), any mood disorder (major depressive disorder, dysthymia, and bipolar disorder), and any substance use disorder (alcohol or drug dependence or abuse).
Mental health service use. The NCS and NCS-R inquired about outpatient service use for "emotions, or nerves or your use of alcohol/drugs" (yes or no) from a variety of providers and settings and for the number of visits in the past year. These questions provided count indices of service use intensity (zero visits or any positive integer). We summed visit counts for three provider categories: mental health providers (psychiatrists, psychologists, and other mental health professionals), social service providers (ministers, priests, rabbis, spiritualists or other healers, social workers, counselors, and other nonmedical professionals), and medical providers (general practitioners or family doctors, other physicians, nurses, occupational therapists, and other medical professionals). These categories were defined to be as consistent as possible, although there were some changes in variables between the two surveys ( 10 , 14 , 15 ).
Analyses
Sampling weights from part II of the NCS and NCS-R were used to adjust for differential household size, nonresponse, and poststratification.
Predictor variables. Sociodemographic predictor variables included age, education level, gender, and race. Access variables included health insurance coverage, employment status, and urban or rural residence. Need variables included the past-year presence of three psychiatric disorder categories (anxiety, mood, and substance use disorders). Additional need variables were derived from items previously reported ( 11 ), including mental health disability (whether the respondent cut down on or was unable to perform usual activities because of a mental health problem for at least one day in the past month) and subjectively perceived need (whether a nonservice user thought that he or she needed to visit a professional for such problems or whether a service user had seen a professional of his or her own free will).
Outcome variables. Outcome variables were the number of unique mental health visits in the past year to mental health providers, social service providers, and medical providers.
Univariate and multivariate analyses. We used zero-inflated negative binomial regression (ZINB), a regression analysis for count data ( 19 , 20 , 21 ), to examine univariate and multivariate associations between the predictor and outcome variables. ZINB was designed for nonnormal count data with excessive zero values, using maximum likelihood estimation to make count outcomes linear. This approach can model service nonuse versus use and can weigh cases accordingly in order to model service use intensity. We controlled for sociodemographic and access variables and assessed the incremental contribution of presence of need variables. Analyses were two tailed and were performed by using Stata, version 9 ( 27 ).
We did not implement a Bonferroni correction to adjust for type I error. This decision was based on the fact that large samples were used that were nationally representative to the general U.S. population, on the fact that we used 12 predictor variables and thus such a such a correction would be overly conservative, and on the fact that such a correction is often needed when examining exploratory hypotheses, whereas our predictor model was based on solid conceptual ( 4 ) and empirical grounds ( 2 , 3 , 5 , 6 , 7 , 11 ).
Results
Descriptive analyses
Demographic characteristics that have been gathered by the NCS and NCS-R have been extensively reviewed. Similar to findings reported by Kessler and colleagues ( 7 ) that were based on the NCS-R, findings from our study showed that 308 NCS respondents (5.2%) and 411 NCS-R respondents (9.5%) visited a mental health provider in the past year. Our study also found that 487 (8.3%) NCS respondents and 418 (9.7%) NCS-R respondents visited a social service provider and that 254 NCS respondents (4.2%) and 484 NCS-R respondents (11.2%) visited a medical provider for mental health-related reasons. As expected, the count variables for mental health visits were extremely skewed, and data transformations were unsuccessful in normalizing distributions.
Univariate analyses
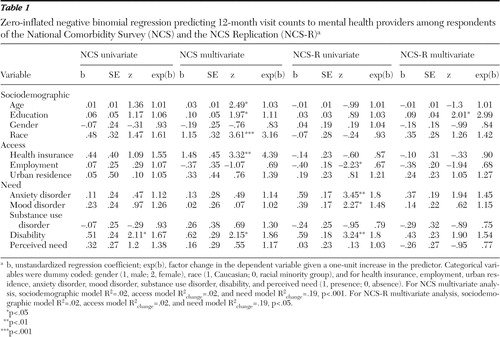
Tables 1 , 2 , 3 report univariate associations between individual predictor variables and visit count outcomes, using univariate ZINB analyses.
 |
 |
 |
Mental health providers. In the NCS data set, only mental health disability was related on a univariate basis to mental health provider visit counts. In the NCS-R data set, in addition to psychiatric disability's association with visit counts, three additional variables were significant: being unemployed, having an anxiety disorder, and having a mood disorder.
Social service providers. In the NCS, only the presence of an anxiety disorder was related on a univariate basis to social service provider visit counts. In the NCS-R data set, two variables were related to social services visits: lacking health insurance and having a mental health disability.
Medical providers. In the NCS data set, two variables were significantly related on a univariate basis to medical provider visit counts: unemployment and having a substance use disorder. In the NCS-R, need variables were related to medical provider visit counts: having an anxiety or mood disorder, having a psychiatric disability, and perceived treatment need.
Multivariate analyses
Tables 1 , 2 , 3 also present results from multivariate ZINB analyses (final models), testing associations between need variables (step 3) and provider visit count outcomes after first controlling for sociodemographic variables (step 1) and access variables (step 2). For the multivariate analyses, data were available for 5,805 persons in the NCS data set and for 4,220 persons in the NCS-R data set.
Mental health providers. In the NCS data set, the need model (step 3) was significantly associated with mental health provider visit counts ( χ2 =40.49, df=12, p<.001), contributing incrementally over the access model (likelihood ratio: χ2 =30.87, df=5, p<.001). Significant final model variables were older age, having more education, being Caucasian, possessing health insurance, and having a psychiatric disability.
In the NCS-R, the need model (step 3) was significantly associated with mental health provider visit counts ( χ2 =22.84, df=12, p<.05), contributing incrementally over the access model (likelihood ratio: χ2 =14.06, df=5, p<.05). However, only higher education level was significant in the final model.
Social service providers. In the NCS data set, the need model (step 3) was significantly associated with social service provider visits ( χ2 =31.24, df=12, p<.01), contributing incrementally over the access model (likelihood ratio: χ2 =24.57, df=5, p< .001). Being younger, being female, and having an anxiety or substance use disorder were significant.
In the NCS-R data set, the access model (step 2) incrementally enhanced predictions over the sociodemographic model for visits to social service providers (likelihood ratio: χ2 =10.29, df=3, p<.05), but the need model (step 3) did not contribute additional variance. Lacking health insurance was the only significant variable.
Medical providers. In the NCS, the access model (step 2) incrementally contributed variance over the sociodemographic model (likelihood ratio: χ2 =23.56, df=3, p<.001), but the need model (step 3) did not contribute incrementally. However, in the final model only having a substance use disorder was significant.
In the NCS-R data set, the need model (step 3) was significantly associated with medical provider visit counts ( χ2 =61.84, df=12, p<.001), contributing incrementally over the access model (likelihood ratio: χ2 =54.33, df=5, p<.001). Older age, less education, rural residence, and having an anxiety or mood disorder were significant.
Service use versus service use intensity
We next assessed whether the predictor variables performed differently when using ZINB univariate and multivariate analyses to model service use (service use versus nonuse) versus service use intensity. We found across NCS and NCS-R analyses that variables representing all three factors in the behavioral model of health care use (that is, sociodemographic, access, and need factors) were more consistently significant in predicting service use (especially in the NCS-R) than in predicting treatment intensity (results not displayed; available by request). One exception to this general finding was that some sociodemographic variables (that is, age, gender, race, and education) were nonsignificant in predicting service use, but they became significant in predicting treatment intensity (as noted above). However, this occurred only for NCS multivariate analyses and not for any NCS-R analyses.
More specifically, in the NCS data set, psychiatric disability and perceived need were associated with both use and intensity of mental health care services across multivariate and univariate analyses. Both psychiatric disability and perceived need also were associated with use, but not intensity, of social and medical services. Employment, urban residence, and mood disorder presence were associated with use, but not intensity, of mental health and social services. In the NCS-R data set, disability again was a consistent univariate correlate of both use and intensity across all three service types. On a multivariate basis, other need variables (mood, anxiety, and substance use disorders and perceived need) were associated with use of mental health specialty and social services, as were demographic variables (that is, age and race) and access variables (that is, insurance and employment); however, these variables were not associated with service use intensity.In the medical services domain, however, both service use and intensity had a similar number of correlates in the NCS-R data set, particularly the need variables (anxiety and mood disorders, disability, and perceived need).
Discussion
We found in univariate analyses that greater intensity of mental health care services was most consistently associated with psychiatric variables, such as mental health disability and the presence of anxiety, mood, or substance use disorders. Service use intensity was not consistently related to access factors or subjectively perceived need and was consistently unrelated to predisposing sociodemographic variables. In multivariate analyses, sociodemographic and access models were inconsistently related to visit counts, and only after adding objective need (that is, psychiatric disorders or disability) did predicting utilization significantly improve in four of six models analyzed. In two analyses, adding need variables did not improve the models, but in one model (that is, social service providers in NCS-R) the only significant variable in the final model was presence of a substance use disorder.
Our results replicate previous research findings that psychiatric disorders and associated disability are the primary predictors of mental health care use ( 5 ). In addition, the study presented here extends this literature, demonstrating that not only service use but also service use intensity is substantially related to objective need factors, such as psychiatric disorders and disability. These findings help quantify those from previous studies on the behavioral model of health care use, suggesting that although sociodemographic and access factors may contribute to the amount of mental health care use, the primary determinant appears to be objective need, as indexed by the presence of psychiatric disorders or disability related to mental health.
General findings
Overall, in the NCS data set, fewer consistent correlates of service use intensity were identified than correlates for service use, and fewer correlates were identified for services provided by social service providers and medical providers than for services provided by mental health providers. In the NCS-R data set, service use again was better accounted for than service intensity, except that both service use and intensity for services provided by a medical provider were consistently associated with objective and subjective need variables. These findings suggest that use of services provided by a mental health care provider may have been more sensitive to objective and subjective need in the NCS era (1990–1992), whereas mental health services provided by a medical provider may be particularly sensitive to needs factors in more recent times (2001–2003 for the NCS-R). This shift is consistent with the general trend of increased provision of mental health care by medical providers and stable or reduced use of mental health specialty services noted in other comparisons of the NCS and NCS-R data sets ( 28 ).
Taken together, these unique findings suggest that, especially in more contemporary times, the managed care initiative's embrace of rationally allocated health care services based on objective need has strongly influenced both the use and intensity of mental health care services. In both eras (NCS, 1990–1992; NCS-R, 2001–2003) the presence of a psychiatric disorder or associated disability (that is, objective need for treatment) more consistently appeared to drive the initial use and continued use of services. However, in the early 1990s, when managed care was just taking root (that is, in the NCS data set), sociodemographic variables were associated with service use intensity. In the next decade (during the NCS-R), sociodemographic and access factors were more equally and consistently associated with initiation of service use, compared with the NCS period; however, by that time objective need (that is, psychiatric disorders and disability) clearly was the dominant correlate of treatment use intensity.
Specific findings
More specific findings warrant comment. In the NCS, anxiety disorder was the psychiatric disorder most consistently associated with use of services provided by social service providers, and substance use disorder was the psychiatric disorder most associated with use of services provided by medical providers. In the NCS-R, mood and anxiety disorders were particularly associated with intensity of mental health services provided by a medical provider. Thus, although specific relationships between the type of psychiatric disorder and mental health service use varied by provider type, the study's overall results support a positive relationship between amount of mental health care use and presence of a mood ( 3 , 6 ), anxiety ( 3 , 6 , 10 ), or substance use disorder ( 3 , 6 ).
Associations between different types of objective need (psychiatric disorders and disability) and the extent of use of mental health-related services varied between the NCS cohort (1990–1992) and the NCS-R cohort (2001–2003). For example, Tables 1 , 2 , 3 indicate that compared with the NCS-R, in the NCS sociodemographic variables were more consistently related to mental health services provided by a mental health provider or a social service provider but not to those provided by a medical provider. In contrast, compared with the NCS, in the NCS-R, objective need variables were more consistently related to mental health visits to a mental health provider or a medical provider but not to a social service provider. This finding may be partly explained by the reduction of stigma related to mental illness and increased acceptance of psychotropic medications ( 29 , 30 ) between the NCS and NCS-R time periods. Additional factors such as financing of health care and social services (for example, copayments and limits on specialty mental health care) are subject to change over time and may contribute to different patterns of mental health-related morbidity and service use ( 31 ).
Sociodemographic and access variables were not as consistently associated with service use as objective need variables. However, age and education were significant service use correlates in two or more analyses. On a multivariate basis, older age was associated with increased service use intensity from a mental health care provider in the NCS and increased service use intensity from a medical provider in the NCS-R, whereas younger age was associated with increased service use intensity from a social service provider in the NCS. Thus our study showed that older individuals appear to use more formal health care services and that younger adults tend to use more allied social services for mental health problems, consistent with the findings of a previous study ( 1 ).
Education was positively associated with intensity of service use from mental health providers in multivariate analyses for the NCS and NCS-R cohorts. This finding was consistent with previous findings on service use ( 32 ), although our study extended these findings to intensity of service use. However, education was inversely associated with intensity of mental health-related services provided by a medical provider in NCS-R multivariate analyses. This finding suggests that although medical services for psychiatric problems were equally used by persons of all levels of education even as recently as a decade ago, in recent years persons with more education may be less likely to use as many physician-provided services for mental health, perhaps increasingly relying upon specialty mental health services.
Interestingly, gender and race had no more than one significant association with mental health-related service use intensity across provider types. On a multivariate basis in the NCS cohort, Caucasian race was associated only with service use provided by mental health providers, and female gender was associated only with service use provided by human and social service providers. Those positive findings replicate results from NCS service use studies, suggesting that in the NCS cohort not only service use but also service use intensity was related to gender (in social services) and race (in mental health specialty services) ( 1 ). The absence of such relationships with service use intensity in the NCS-R cohort suggests that gender and race may play a smaller role over the past decade in service use patterns.
Two of three access variables, health insurance and employment status, had more than one significant relationship with service use across univariate and multivariate analyses. Health insurance was unrelated to service use intensity of medical care for mental health-related problems but was positively related to mental health specialty use in the NCS only and inversely related to human and social service use in the NCS-R only. The past decade has emphasized managed care and reducing mental health costs at a rate disproportionate to those of other health care ( 33 ). Thus lacking insurance now appears to be associated with seeking less costly social services for mental health, perhaps in part because having insurance may no longer be sufficient to let people obtain or afford mental health specialty care.
Several instances were found where a given predictor variable was correlated with treatment use intensity in a univariate analysis but lost significance when other variables were controlled for in multivariate analysis. For example, NCS-R analyses demonstrated at least some significant univariate associations for need variables; however, these associations were not significant when multivariate analysis was performed. It is possible that the lack of multivariate association for these variables is due to shared variance between need, sociodemographic characteristics, and access factors and that controlling for sociodemographic and access factors accounts for the association between need and service use.
Previous studies tend to indicate a larger number of consistent significant relationships, compared with our study—especially for demographic correlates of treatment use. This discrepancy can be explained by two methodological factors. First, sociodemographic and need variables have a greater and more consistent relationship with predicting treatment access (which has been explored previously) than treatment intensity (which was confirmed by our findings). Second, research that examined correlates of mental health treatment intensity ( 14 , 15 ) did not use newer analyses designed to account for skewed visit count distributions. The latter studies ( 14 , 15 ) found that the number and types of mental disorders were consistently related to treatment use intensity (but not for mental health services provided by a medical provider); however, our study did not find these correlations to be consistent. Because using such skewed data can result in mistakenly concluding that nonmeaningful relationships are statistically significant ( 18 ), the previous work should be cautiously interpreted given our findings. On the basis of new statistical advances, we would argue that sociodemographic and access variables are related more to entering treatment than to treatment intensity. It also is possible, however, that changes in health care delivery over the past two decades have progressively reduced the influence of sociodemographic and enabling factors (for example, ethnocultural background, gender, and insurance) in determining the amount of services that people receive for mental health problems.
Methodological limitations should be taken into account when interpreting these findings. Self-report has demonstrated some underestimation of visit counts ( 34 ). Additionally, more psychometrically robust measures of disability or perceived need may better operationalize perceived need than the single items use. Finally, the three classes of treatment providers are not necessarily independent of each other, because previous research has indicated that some individuals use multiple types of providers for mental health treatment ( 28 ).
Conclusions
This study adds to literature on factors associated with mental health care use by extending prior findings concerning the role of objective need (that is, psychiatric morbidity and disability) as a robust correlate of intensity of mental health care use across three types of providers and sociodemographic factors (for example, gender and ethnicity) and enabling factors (for example, insurance, employment, and education) as robust correlates of initiating mental health services but not of continuing services. Our findings also suggest that the objectively determined presence of a psychiatric disorder and associated disability are more important determinants of mental health care use recently (that is, in the NCS-R cohort) than they were a decade ago (that is, in the NCS cohort). Although these data cannot directly elucidate changes in well-documented disparities in mental health care use based on such factors as gender and race ( 1 ), they indicate that—to the extent that psychiatric diagnoses are evaluated without bias for demographic factors—providers of mental health services may be basing their decisions about the amount of services provided to patients less on predisposing factors and more on objectively determined psychiatric need. More direct empirical tests of this hypothesis are needed. Overall, the demonstration of some consistency and some alterations in the patterns of associations between factors in the behavioral model of health care use and service use intensity in the two survey periods indicates that as the health care system (for example, financing and service delivery models) changes over time, it is essential to monitor the pattern of service use correlates in order to guide future planning for mental health services.
Acknowledgments and disclosures
The authors thank Don Richardson, M.D., and Todd B. Kashdan, Ph.D., for their helpful comments.
The authors report no competing interests.
1. Kessler RC, Demler O, Frank RG, et al: Prevalence and treatment of mental disorders, 1990 to 2003. New England Journal of Medicine 352:2515–2523, 2005Google Scholar
2. Wang PS, Lane M, Olfson M, et al: Twelve-month use of mental health services in the United States. Archives of General Psychiatry 62:629–640, 2005Google Scholar
3. Lewis SF, Resnick HS, Ruggiero KJ, et al: Assault, psychiatric diagnoses, and sociodemographic variables in relation to help-seeking behavior in a national sample of women. Journal of Traumatic Stress 18:97–105, 2005Google Scholar
4. Andersen RM: Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36:1–10, 1995Google Scholar
5. Bland RC, Newman SC, Orn H: Help-seeking for psychiatric disorders. Canadian Journal of Psychiatry 42:935–942, 1997Google Scholar
6. Parslow RA, Jorm AF: Who uses mental health services in Australia? An analysis of data from the National Survey of Mental Health and Wellbeing. Australian and New Zealand Journal of Psychiatry 34:997–1008, 2000Google Scholar
7. Kessler RC, Chiu WT, Demler O, et al: Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:617–627, 2005Google Scholar
8. Kessler RC, Olfson M, Berglund PA: Patterns and predictors of treatment contact after first onset of psychiatric disorders. American Journal of Psychiatry 155:62–69, 1998Google Scholar
9. Bruce ML, Wells KB, Miranda J, et al: Barriers to reducing burden of affective disorders. Mental Health Services Research 4:187–197, 2002Google Scholar
10. Greenberg PE, Sisitsky T, Kessler RC, et al: The economic burden of anxiety disorders in the 1990s. Journal of Clinical Psychiatry 60:427–435, 1999Google Scholar
11. Katz SJ, Kessler RC, Frank RG, et al: The use of outpatient mental health services in the United States and Ontario: the impact of mental morbidity and perceived need for care. American Journal of Public Health 87:1136–1143, 1997Google Scholar
12. Leaf PJ, Bruce ML, Tischler GL, et al: Factors affecting the utilization of specialty and general medical mental health services. Medical Care 26:9–26, 1988Google Scholar
13. Rayburn NR, Wenzel SL, Elliott MN, et al: Trauma, depression, coping, and mental health service seeking among impoverished women. Journal of Consulting and Clinical Psychology 73:667–677, 2005Google Scholar
14. Kessler RC, Zhao S, Katz SJ, et al: Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry 156:115–123, 1999Google Scholar
15. Kessler RC, Frank RG, Edlund M, et al: Differences in the use of psychiatric outpatient services between the United States and Ontario. New England Journal of Medicine 336:551–557, 1997Google Scholar
16. Elhai JD, Patrick SL, Anderson S, et al: Gender- and trauma-related predictors of use of mental health treatment services among primary care patients. Psychiatric Services 57:1505–1509, 2006Google Scholar
17. Bao Y: Predicting the use of outpatient mental health services: do modeling approaches make a difference. Inquiry 39:168–183, 2002Google Scholar
18. Gardner W, Mulvey EP, Shaw EC: Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychological Bulletin 118:392–404, 1995Google Scholar
19. Hall DB, Zhengang Z: Marginal models for zero inflated clustered data. Statistical Modeling 4:161–180, 2004Google Scholar
20. Cameron AC, Trivedi PK: Regression Analysis of Count Data. New York, Cambridge University Press, 1998Google Scholar
21. Long JS: Regression Models for Categorical and Limited Dependent Variables. Thousand Oaks, Calif, Sage, 1997Google Scholar
22. Kessler RC: National Comorbidity Survey, 1990–1992 (Computer File). Conducted by University of Michigan, Survey Research Center. 2nd ed. Ann Arbor, Mich, Inter-University Consortium for Political and Social Research, 2002Google Scholar
23. Kessler RC: National Comorbidity Survey: Replication (NCS-R), 2001–2003 (Computer File). Conducted by Harvard Medical School, Department of Health Care Policy/University of Michigan, Survey Research Center. Pub no ICPSR04438-v1. Ann Arbor, Mich, Inter-University Consortium for Political and Social Research, 2006Google Scholar
24. Composite International Diagnostic Interview (CIDI), Version 1.0. Geneva, World Health Organization, 1990Google Scholar
25. Wittchen HU: Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. Journal of Psychiatric Research 28:57–84, 1994Google Scholar
26. Andrews G, Peters L: The psychometric properties of the Composite International Diagnostic Interview. Social Psychiatry and Psychiatric Epidemiology 33:80–88, 1998Google Scholar
27. Stata, version 9. College Station, Tex, StataCorp, 2005Google Scholar
28. Wang PS, Demler O, Olfson M, et al: Changing profiles of service sectors used for mental health care in the United States. American Journal of Psychiatry 163:1187–1198, 2006Google Scholar
29. Corrigan P, Gelb B: Three programs that use mass approaches to challenge the stigma of mental illness. Psychiatric Services 57:393–398, 2006Google Scholar
30. Mojtabai R: Americans' attitudes toward mental health treatment seeking: 1990–2003. Psychiatric Services 58:642–651, 2007Google Scholar
31. Mark TL, Coffey RM, Vandivort-Warren R, et al: US spending for mental health and substance abuse treatment, 1991–2001. Health Affairs 24(suppl Web exclusives): W5-133–W5-142, 2005Google Scholar
32. Ten Have M, Oldehinkel A, Vollebergh W, et al: Does educational background explain inequalities in care service use for mental health problems in the Dutch general population? Acta Psychiatrica Scandinavica 107:178–187, 2003Google Scholar
33. Barry CL, Gabel JR, Frank RG, et al: Design of mental health benefits: still unequal after all these years. Health Affairs 22(5):127–137, 2003Google Scholar
34. Roberts RO, Bergstralh EJ, Schmidt L, et al: Comparison of self-reported and medical record health care utilization measures. Journal of Clinical Epidemiology 49:989–995, 1996Google Scholar



