Feasibility, Acceptability, and Sustainability of Telepsychiatry for Children and Adolescents
Psychiatric disorders affect from 7% to 20% of children and adolescents ( 1 ), but most youths receive inadequate care. Those living in nonmetropolitan areas are especially underserved ( 2 ) because evidence-based treatments are not widely disseminated outside of urban areas ( 3 ). In nonmetropolitan areas primary care physicians sustain a "hidden mental health network" in that they routinely screen for developmental, behavioral, and educational difficulties. Also, guidelines are available for treating common pediatric mental disorders ( 4 ). However, multiple factors prevent primary care physicians from evolving further as frontline mental health providers ( 5 , 6 ). Having better mental health referral sources would strengthen their practice and improve patients' care. Telepsychiatry offers one means of building mental health referral sources.
In this brief report, we present preliminary work on the feasibility, acceptability, and sustainability of a telepsychiatry service for children and adolescents. Feasibility refers to whether a community needs psychiatric services and whether telepsychiatry can meet those needs. Acceptability refers to whether involved parties are satisfied with services provided. Sustainability refers to whether financial models adequately reimburse services and other costs.
Methods
This study protocol was approved by the institutional review board of Children's Hospital and Regional Medical Center (CHRMC) in Seattle, Washington. CHRMC provides on-site specialty care at 20 satellite or regional outpatient locations throughout Washington, Alaska, Montana, and Idaho, which is complemented by telemedicine services through the Children's Health Access Regional Telemedicine (CHART) program. Four of these sites include telepsychiatry: Olympia, Wenatchee, Longview, and Yakima.
Olympia, the state capital, is a city with a population of 207,000 located 75 miles south of Seattle. The economy is based on government, agriculture, insurance, and the local college. The population is over 85% Caucasian. Despite its size, location, and two mental health centers, Olympia has experienced a chronic shortage of child and adolescent psychiatrists. Olympia is the site of a CHRMC satellite clinic and joined CHART in October 2001.
Wenatchee is a town of 29,000 located more than 150 miles northeast of Seattle over two mountain passes. Agriculture, forestry, and ranching support the economy. Hispanics constitute the largest ethnic minority group (<16%). Wenatchee has also had a chronic shortage of child and adolescent psychiatrists. In October 2001 Wenatchee's Central Washington Hospital began to host CHART for the larger region of north-central Washington.
Longview is a town of 36,000 located more than 150 miles southwest of Seattle. This community has struggled with failing fishing and timber industries. Longview has a small population of ethnic minority groups (11%), predominantly African American and Hispanic. Longview has had great difficulty in retaining child and adolescent psychiatrists who initially settle in the community. In October 2003 Longview's Child and Adolescent Clinic joined CHART.
Yakima is a city of 73,000 lying 150 miles southeast of Seattle across a mountain pass. Agriculture and ranching form the major economy. Approximately 40% of the population is Hispanic. Yakima has had access to three child and adolescent psychiatrists plus two nurse mental health practitioners. Children's Village, a freestanding specialty referral clinic, started to host CHART in 2002.
Telepsychiatry sites are linked to CHRMC by Polycom MP or FX videoconferencing equipment by using integrated services digital network (ISDN) lines with a bandwidth of 384 kbps, providing "near-TV" quality. Transmission protocols were compliant with requirements of the Health Insurance Portability and Accountability Act (HIPAA).
Telepsychiatrists serving these four clinics consisted of three child and adolescent psychiatrists who were faculty at the University of Washington School of Medicine. They met via videoconferencing with parents and youths together, then separately as clinically indicated and tolerated. Although referring physicians were invited to attend the sessions, none did so. Frequently, the family invited a teacher, therapist, or other professional to the sessions. After completion of each session, the telepsychiatrist sent a note by fax summarizing findings while the referring physician awaited the full report in two to three weeks. The service model was not rigid. Treatment was individualized and recommendations implemented according to preferences of the family, referring physician, and telepsychiatrist. For example, either the telepsychiatrist or referring physician might prescribe medication depending on complexity of the medication regimen, practice preference of the telepsychiatrist, and convenience of the family.
Referring physicians included pediatricians and family physicians. Physicians could refer any patient for whom they wanted help. There was no screening or triage. The caseload included a range of patients, diagnoses, and severity of problems. Generally, patients tended to present complex problems, with multiple diagnoses, prior complications, and multiple interventions, including polypharmacy.
Services were initially provided free through a grant from the Office for the Advancement of Telehealth (2000–2005) and subsequently through fee for service. First, we negotiated coverage with Washington State Medicaid and then used these agreements to negotiate with commercial payers. A review of benefits and a preauthorization process were undertaken before providing any services.
For the study reported here, profiles for demographic characteristics, utilization, and diagnoses for telepsychiatry visits were developed for January 1 through December 31, 2004. The hospital clinic scheduling system was used to identify telepsychiatry visits. Payer mix was determined via hospital billing systems.
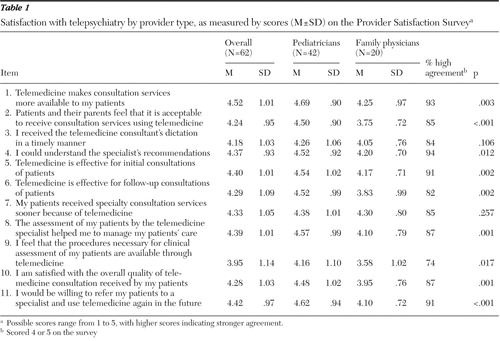
The Provider Satisfaction Survey is an 11-item self-administered questionnaire that assesses referring physicians' satisfaction with telemedicine service. Five domains associated with provider satisfaction in previous studies ( 7 ) were assessed: technical quality, attitudes regarding access, clinical appropriateness, perceived patient acceptance, and global satisfaction. The survey was sent quarterly to referring providers. Only one survey was sent, regardless of the number of referrals made.
Differences in provider satisfaction were analyzed with the Kruskal-Wallis nonparametric rank test and the Mann-Whitney rank-sum test from SPSS version 12.1.1.
Results
During the study period 387 telepsychiatry encounters were provided for 172 patients, with a mean±SD of 2.25±2.2 encounters. Patients ranged from two to 21 years of age (8.6±3.2 years), predominantly boys (118 boys, or 69%). Twenty-three (6%) visits were for children two to five years old, 290 visits (75%) were for children six to 13 years old, and 74 visits (19%) were for youths 14 to 21 years old, which was representative of outpatient mental health clinics ( 1 ). Utilization varied. Olympia had the largest number of visits (149 visits, or 39%), with an average of 2.6 patients per physician. Longview utilized 119 visits (31%), with an average of 3.5 patients per physician. Wenatchee followed with 85 visits (22% of total), an average of 2.5 patients per physician. Yakima used only 34 visits (8%), with an average of 4.0 patients per physician.
Diagnoses across encounters were typical of outpatient child and adolescent psychiatry clinics ( 1 , 7 ), the most common being attention-deficit hyperactivity disorder (175 encounters, or 45%) and other disruptive behavior disorders (31 encounters, or 8%); mood disorders (62 encounters, or 16%); developmental disorders, including autism spectrum (54 encounters, or 14%); anxiety disorders (23 encounters, or 6%); adjustment disorders (19 encounters, or 5%); tic disorders (four encounters, or 1%); and other disorders (19 encounters, or 5%).
Sixty-two (50% response rate) primary care providers returned satisfaction questionnaires. Forty-two (68%) were pediatricians and 20 (32%) were family practice physicians. Overall mean scores were strong ( Table 1 ). Referring providers rated item 1 the highest, at 4.52 of 5 possible points: "Telemedicine makes consultation services more available to my patients." Item 9 had the lowest rating, of 3.95: "I feel that the procedures necessary for clinical assessment of my patients are available through telemedicine," suggesting that referring physicians thought that their patients needed more than telepsychiatry could provide. Although both groups of physicians were highly satisfied with their patients' care, pediatricians endorsed significantly higher ratings on nine of the 11 items.
 |
Diagnostic evaluations (Current Procedural Terminology [CPT] code 90801) and medication management (CPT 90862) were the most frequently provided services, at 32% and 48% of sessions, respectively. Commercial and public payers included the Public Employees Benefits Board, Community Health Plan of Washington, Molina, Healthy Options, Pacific Medical, Premera Blue Cross, Regence, Uniform Medical, TriCare, and Department of Social and Human Services. In addition, Blue Cross-Blue Shield and First Choice covered telepsychiatry services under selected conditions. Several major insurers did not cover telepsychiatry, but we were able to negotiate single-case payment: Pacific Care, First Choice Health Network, United Health Care, Private Healthcare Systems, One Health Plan-Great West, Basic Health Plan, First Health, First Health Network, Cigna, and Aetna.
For CPT code 90801 (initial evaluation), Medicaid reimbursed $87.36 and commercial payers reimbursed from $171.45 to $222.20. For CPT code 90862 (medication treatment), public payers reimbursed from $29.30 to $31.30, and commercial payers reimbursed from $50.35 to $111.79. These reimbursements by both public payers and commercial payers were identical to their respective reimbursements in our outpatient psychiatry clinic: overall, Medicaid reimbursed 23% of billed charges in each clinic and commercial payers reimbursed 42% in telepsychiatry and 43% in the outpatient clinic. However, telepsychiatry included more total Medicaid patients, resulting in overall lower collectability of 28% for telepsychiatry versus 38% for our on-site outpatient clinic. Collectability takes into account multiple factors such as the "discounts" that payers negotiate with providers and refusal of payment due to use of unauthorized CPT codes. Currently, CHRMC underwrites these losses.
Discussion and conclusions
The results of our study demonstrated the feasibility and acceptability of telepsychiatry for providing care to underserved youth. Challenges to sustainability were also elucidated.
Feasibility was demonstrated by the demographic, clinical, and utilization profiles of our telepsychiatry service. Telepsychiatry was not used for a select population but served youths representative of in-person psychiatric clinics ( 1 , 7 ). Multiple physicians referred multiple youths, and most youths returned for a second session.
Acceptability was shown by providers' high satisfaction ratings. Although satisfaction does not equate to effectiveness, the availability of very few outcome studies ( 8 , 9 ) in the face of mushrooming telepsychiatry programs ( 10 ) leaves acceptability data to point the way to more systematic study of effectiveness. For example, if telepsychiatry is to build effective referral networks, these disparate satisfaction ratings by pediatricians and family physicians underscore that future outcome studies must address the specific needs of different disciplines ( 11 ).
Our experience demonstrates the financial challenges to sustainability. Multiple factors must be considered. The poor utilization by Yakima was predictable. During our feasibility study, Yakima was interested in only selected medical services, not psychiatry. Sustainability is predicated on abiding by the needs assessment.
Our overrepresentation of Medicaid and public payer cases attests to the ability of telepsychiatry to reach the neediest patients but also indicates the liability of including suboptimal reimbursement in a fee-for-service model. Major medical centers may tolerate such reimbursement in order to meet their mission and stakeholders' interests, but individual telepsychiatrists will not be able to accept such an adverse case mix. Although accurate data are difficult to ascertain, reimbursement records indicate that in 2003, from 23 to 27 states included telepsychiatry in their Medicaid services ( 12 ). Recently, at the urging of the American Telemedicine Association, the Centers for Medicare and Medicaid Services announced plans to increase reimbursement for selected neurobehavioral services (www.cms.hhs.gov/apps/ama/license.asp?). In 2005 a total of 116 telemedicine programs were identified, and from 38 ( 12 , 13 ) to 64 ( 14 ) programs reported private reimbursement.
The good news is that insurers increasingly are covering telepsychiatry, but the bad news is that even the best reimbursement will not cover infrastructural costs such as purchase of equipment, its upkeep, line charges, and technical consultation. To minimize risk, alternative models should be considered, such as contracting for a set amount of the telepsychiatrist's time, including coverage for infrastructural costs, or requesting a facility charge for both the provider and patient sites. In the future, infrastructural costs will decrease as secure, but expensive, point-to-point ISDN lines are replaced by lower-cost broadband Internet protocols. However, Internet protocols do not provide secure point-to-point transmission. Thus this next step awaits the development of HIPAA-compliant encryption protocols.
Naturalistic observational studies are subject to many biases, and the findings reported here should not be overinterpreted. Specifically, although satisfaction does not equate with effectiveness, it does suggest that the field is ready for systematic, controlled study. The response rate from our referring physicians was only 50%, which raises questions about the representativeness of the sample. Also, we did not survey our telepsychiatrists' satisfaction, an important topic because psychiatrists have been more reluctant than primary care physicians and patients to use this new medium for health services. Finally, we did not survey youths. Our prior experience ( 15 ) suggests that teens offer a valuable perspective that should be included in future studies.
In conclusion, telepsychiatry offers a valuable service that reaches typical youths in need of psychiatric care. These services are acceptable to primary care physicians. However, sustainability is a challenge. Feasibility studies must be conducted before implementing services and financial models considered during these feasibility studies. Future controlled studies are now needed to assess whether telepsychiatric care is more effective than treatment as usual in primary care and as effective as in-person evidence-based psychiatric care.
Acknowledgments and disclosures
This work was supported by grant D1-BTH00008-02-08 from the Office for the Advancement of Telehealth, Health Resources and Services Administration.
The authors report no competing interests.
1. Friedman R, Katz-Leavy J, Manderscheid R, et al: Prevalence of serious emotional disturbance in children and adolescents, in Mental Health: United States. Edited by Manderscheid R, Sonnenschein MA. Rockville, Md, Department of Health and Human Services, 1996Google Scholar
2. Achieving the Promise: Transforming Mental Health Care in America. Pub no SMA-03-3832. Rockville, Md, Department of Health and Human Services, President's New Freedom Commission on Mental Health, 2003Google Scholar
3. Chorpita BF: Treatment manuals for the real world: where do we build them? Clinical Psychology Science and Practice 9:431–433, 2002Google Scholar
4. American Academy of Pediatrics, Committee on Psychosocial Aspects of Child and Family Health: The new morbidity revisited: a renewed commitment to the psychosocial aspects of pediatric care. Pediatrics 108:1227–1230, 2001Google Scholar
5. Phillips S, Clawson L, Osinski A: Pediatricians' pet peeves about mental health referrals. Journal of Adolescent Medicine 9:243–258, 1998Google Scholar
6. Cohn RJ: Health professionals' attitudes to videoconferencing in paediatric health-care. Journal of Telemedicine and Telecare 8:274–282, 2002Google Scholar
7. Myers KM, Sulzbacher S, Melzer SM: Telepsychiatry with children and adolescents: are patients comparable to those evaluated in usual outpatient care? Telemedicine Journal and E-Health 10:278–285, 2004Google Scholar
8. Ruskin P, Silver-Aylaian M, Kling MA, et al: Treatment outcomes in depression: comparison of remote treatment through telepsychiatry to in-person treatment. American Journal of Psychiatry 161:1471–1476, 2004Google Scholar
9. Nelson E, Barnard M, Cain S: Treating childhood depression over videoconferencing. Telemedicine Journal and E-Health 9:49–55, 2003Google Scholar
10. Office for the Advancement of Telehealth: Grantee Directory: 2004–2005. Rockville, Md, US Department of Health and Human Services, 2006. Available at telehealth.hrsa.gov/grants/grantee.htmGoogle Scholar
11. Godleski L, Darkins A, Lehmann L: Telemental Health Toolkit, Field Work Group of the Veterans' Health Administration. Chapel Hill, NC, 2003Google Scholar
12. Brown NA: State Medicaid and private payer reimbursement for telemedicine: an overview. Journal of Telemedicine and Telecare 12(Suppl):32–30, 2006Google Scholar
13. Private Payer Reimbursement Information Directory. North Chelmsford, Mass, AMD Telemedicine. Available at www.amdtelemedicine.com/privatepayer/aboutsurvey.cfmGoogle Scholar
14. Whitten P, Buis L: Private payer reimbursement for telemedicine services in the United States. Telemedicine Journal and E-Health 13:15–23, 2007Google Scholar
15. Myers K, Valentine J, Morganthaler R, et al: Telepsychiatry with incarcerated youth. Journal of Adolescent Health 38:643–648, 2006Google Scholar



