Personality Disorder and Chronicity of Addiction as Independent OutcomePredictors in Alcoholism Treatment
Alcoholism causes enormous societal costs and is among the leading causes of death in industrialized countries ( 1 , 2 ). Thus research on alcoholism treatment is of major importance for public health. A central issue of therapy research is to estimate the intensity of treatment needed on the basis of addiction severity of individuals. This approach is based on the assumption that patients whose addiction is less severe than others' might also benefit from less intensive treatment, whereas patients whose addiction is more severe need a more intensive therapy. However, it is far from clear which variables within the broad range of substance use data constitute the essential features of addiction severity.
One way to determine the important characteristics is to identify outcome predictors of addiction therapy. Numerous investigations have tried to detect such predictors ( 3 ). Among this vast literature the traditional alcoholism typologies stand out, for example, the famous Jellinek classification ( 4 ). His gamma and delta types share prominent features with other well-known typologies, for example, Cloninger's type I/type II or Babor's type A/type B dichotomy ( 5 ). These typologies include factors such as early onset of alcohol dependence and chronic psychopathological impairment, which resembles the contemporary concept of comorbid personality disorder. Surprisingly, however, empirical data on the significance of chronicity and personality disorders for outcome in alcoholism treatment are rare and inconsistent ( 3 , 5 , 6 ).
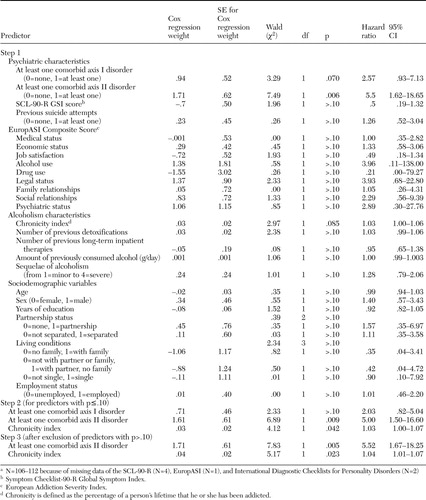
The goal of this prospective longitudinal study was to examine which components of addiction severity ( see Table 1 ) predict time to relapse for a sample of 112 chronic alcohol-dependent patients who participated in a comprehensive and intensive two-year outpatient treatment program. We collected various data on sociodemographic and alcoholism characteristics, as well as on psychiatric comorbidity at the beginning of treatment. Beginning from admission to outpatient treatment, we monitored alcohol abstinence by contacts and urine and blood analyses for the two years of therapy and for two additional years after termination of treatment. Prediction of time from first outpatient contact to relapse was determined by survival analysis.
 |
a N=106-112 because of missing data of the SCL-90-R (N=4), EuropASI (N=1), and International Diagnostic Checklists for Personality Disorders (N=2)
Methods
The study presented here is part of an ongoing research project approved by the local ethics board. This project investigates the effectiveness of the outpatient long-term intensive therapy for alcoholics (OLITA), which was initiated in 1993. Since its inception, the program has included 180 people with severe chronic alcoholism. OLITA is a four-step program of integrated outpatient care and aims for immediate social reintegration. The success rate, expressed as continuously abstinent patients after termination of the two-year OLITA program, is about 50 percent ( 7 ).
The prospective study reported herein included recruitment cohorts 4 to 6 of six cohorts to which patients are assigned. After we completely described the study, patients provided their written informed consent to participate.
Between March 1998 and June 2002, 118 patients were consecutively admitted. Inclusion criteria were having alcohol dependence ( DSM-IV ), living in a nearby residence, and having health insurance to cover the costs of treatment. Exclusion criteria were being older than 60 years, having Korsakoff syndrome, or having acute concurrent dependence on a substance other than alcohol (with the exception of caffeine and nicotine).
Of 276 patients to whom the program was presented and who fulfilled the eligibility criteria, 129 (47 percent) were inpatients referred from different wards, 61 (22 percent) were brought in from the emergency department, 50 (18 percent) were outpatients who came in on their own initiative, 23 (8 percent) were referred by external institutions (general practitioners, addiction counselors, and probation service), and 13 (5 percent) were inpatients who entered the program on their own initiative. Of all 276 patients, 143 kept appointments during mandatory inpatient detoxification, 132 came for first outpatient orientation sessions after discharge, and 118 patients decided to participate in OLITA. Data for four participants were not used because of language barriers, and data for two patients could not be obtained because the patients could not read.
Of the final 112 participants, 46 (41 percent) were referred from different wards, 32 (28 percent) were outpatients who entered on their own initiative, 13 (12 percent) came from the emergency department, 12 (11 percent) were referred by external institutions, and nine (8 percent) were inpatients who entered on their own initiative.
Alcohol abstinence was the primary outcome measure and was strictly monitored by sampling urine and blood within the framework of frequent therapeutic and follow-up contacts. Urinalyses were carried out daily during months 1 through 3, three times per week during months 4 through 6, twice per week during months 7 through 12, at least weekly during months 13 through 24, and weekly to quarterly after termination of treatment for another two years. Blood was analyzed for ethanol and diverse routine parameters, also comprising indicators of liver function and alcohol consumption such as gamma-glutamyltransferase (gamma-GT), alanine aminotransferase (ALT), aspartate aminotransferase (AST), and mean corpuscular volume of red blood cells (MCV).
Tests were performed at least every two weeks during months 1-3, monthly during months 4-12, bimonthly until the end of therapy, and at least twice per year after termination of treatment for another two years. An alcohol relapse was interpreted as recurrence of an addictive drinking pattern that resulted in a premature termination of treatment or cessation of posttreatment follow-up visits. Blood or urine samples that were positive for alcohol or other drugs of abuse were counted as relapse, as were self-reports of substance use even if not confirmed by laboratory analysis. Patients who spontaneously dropped out of treatment and could not be reached by therapeutic interventions or subsequent follow-up contacts were also considered to have relapsed (with the day after the last therapeutic contact counted as the relapse date).
To control for variation in age, an index was constructed to measure chronicity of addiction. Chronicity was defined as the percentage of a patient's lifetime that he or she has been addicted. The chronicity index was calculated by multiplying 100 by the ratio of duration of dependence and age at the beginning of therapy. The resulting parameter ranges from >.0 to <100.
DSM-IV axis II disorders were diagnosed with the International Diagnostic Checklists for Personality Disorders (IDCL-P) ( 8 ), which resulted in a very high interrater reliability between two independent rater teams (kappa=.82 for the judgment "at least one personality disorder," median kappa=.79 for the judgments of 13 specific categories of personality disorders). Two prerequisites for diagnosis were that the raters had to be clinicians who had observed a patient throughout a variety of situations over several months and that a diagnosis of personality disorder was made only for patients who had passed the third abstinent month (N=110) to avoid misinterpretation of temporary withdrawal-related dysfunctions as symptoms of personality disorders. Ratings were based on clinicians' experiences with patients, psychiatric history, the semistructured clinical interviews EuropASI (European Addiction Severity Index, for assessment of alcoholism-related problems) ( 9 , 10 ) and MiniDIPS (diagnosis of DSM-IV axis I disorders) ( 11 , 12 ), the Symptom Checklist SCL-90-R (self-rating of current psychiatric symptoms) ( 13 , 14 ), therapeutic records, videotapes of therapy sessions, patient files, and information by other therapists and relatives. Whereas 12 categories were defined by specific DSM-IV criteria, a diagnosis of personality disorder not otherwise specified (NOS) comprised alcohol-induced personality impairment or mild mental retardation.
The mean±SD age of participants was 43.6±7.6 years, 81 participants (72 percent) were male, and 64 participants (57 percent) were unemployed. The duration of dependence (according to DSM-IV criteria) amounted to 18.1±7.3 years, with an average daily alcohol consumption of 437.2±175.5 g of pure alcohol and 7.5±9.6 prior inpatient detoxifications. Of 110 patients, 71 (or 65 percent) met criteria for at least one comorbid personality disorder. Narcissistic personality disorder and personality disorder NOS were diagnosed for 17 (15 percent) patients each; 11 patients (10 percent), borderline personality disorder; ten patients (9 percent), dependent; seven (6 percent), antisocial; six (5 percent), avoidant; six (5 percent), histrionic; three (3 percent), depressive; and two (2 percent), paranoid personality disorder. Schizotypal and passive-aggressive personality disorders were assigned for one patient each (1 percent). Eight patients (7 percent) met criteria for at least two personality disorders. Two patients relapsed and dropped out of treatment before they were given a diagnosis of personality disorder.
The Kaplan-Meier survival analysis and Cox regression analysis programs of the SPSS for Windows software package (release 12) were used for statistical analyses. All statistical tests were two-tailed. We performed a survival analysis to investigate the time-to-event measure of days from first outpatient contact to relapse. The corresponding survival curve of remaining without relapse was obtained with the Kaplan-Meier estimate. Cox proportional hazard models were used to examine associations of time-invariant predictors (that is, patient characteristics) with time to relapse. Cases were censored if patients had not experienced an event (relapse) by the end of follow-up, including one patient who died.
Because the sample was too small to include all predictors in one model, we chose the following procedure to construct a valid set of predictors: In the first step, four separate prediction models were calculated for psychiatric variables (at least one axis I disorder, at least one axis II disorder, SCL-90-R Global Symptom Index score, previous suicide attempts), EuropASI composites (medical status, economic status, job satisfaction, alcohol use, drug use, legal status, family relationships, social relationships, and psychiatric status), alcoholism characteristics (chronicity index, number of previous detoxifications, number of previous long-term inpatient therapies, amount of previously consumed alcohol, and sequelae of alcoholism), and sociodemographic variables (age, sex, years of education, partnership status, living conditions, and employment status). In the second step, all predictors at p≤.10 were included in a model consisting of psychiatric predictors, EuropASI composites, alcoholism characteristics, and sociodemographic variables. In the third and last step, predictors at p>.10 in the second step were excluded, and a final model with the remaining variables was calculated.
Results
Cumulative abstinence probability was determined for all 112 patients and calculated from the first outpatient session until the last therapeutic or follow-up contact. During the four-year follow-up, 31 (28 percent) of the 112 patients relapsed, with 25 patients (22 percent) relapsing before and six patients (5 percent) relapsing after the completion of therapy. The Kaplan-Meier estimate of cumulative abstinence probability at four years was .64, with a mean survival time of 1,285 days (range 31 to 1,737 days).
Among the analyzed sociodemographic, psychiatric, and alcoholism-related patient characteristics, only the presence of a personality disorder (Wald χ 2 =7.83, df=1, p=.005) and chronicity of addiction (Wald χ 2 =5.17, df=1, p=.023) were independently associated with a decrease of cumulative four-year abstinence probability ( Table 1 ). Patients with a comorbid personality disorder, higher chronicity of addiction, or both had a lower abstinence probability and a shorter time to relapse than patients without personality disorder, a lower chronicity, or both.
Discussion
This study identified the presence of a comorbid personality disorder and chronicity of addiction as independent predictors of cumulative abstinence probability during a four-year follow-up of alcoholism therapy. Assuming that predictive validity is appropriate to determine essential features of a construct, these results suggest that chronicity and personality disorder rank among the most important characteristics of addiction severity.
Our findings are consistent with the results of previous studies that showed that addiction severity and chronic psychopathological impairment are related to worse substance use outcome ( 5 , 15 ). There are, however, contradictory reports that found no effect or even a positive effect of these variables on treatment outcome ( 3 , 6 ). In comparison with other substance abuse and alcoholism treatment studies that relied only on self-report of patients, collateral informants, and sporadic Breathalyzer or laboratory analyses ( 3 , 5 , 15 ), our study used regular analyses of urine and blood within the framework of frequent therapeutic contacts, ensuring the highest validity of the main outcome variable, abstinence. The relatively small sample size (N=112), too small to include all predictors in one Cox regression analysis, may be a methodological limitation of this study. However, the sample size is high enough for the procedure that we chose, that is, to calculate separate prediction models with the number of covariates ranging from two to nine.
Regarding future research on alcoholism typologies, studies with larger sample sizes are needed to investigate explicitly to what extent personality disorder and chronicity of addiction are common underlying factors of the different contemporary alcoholism classifications ( 5 ).
Conclusions
Data from this study cannot and are not meant to answer questions concerning etiological processes—for example, whether the personality disorder predates the alcohol problem or vice versa. However, the practical implications of our study are clear. Severe alcoholism must be considered a chronic and relapsing psychiatric disease that is complicated by a high comorbidity of personality disorders. Contemporary addiction treatment can be successful in interrupting a current consumption period or alleviating acute dependence symptoms, but it does not really address the underlying disorder. Only comprehensive and structured long-term treatment that integrates specific therapeutic elements for personality disorder and is followed by a lifelong participation in check-up sessions and self-help groups will support long-term recovery of patients with severe alcoholism.
Acknowledgment
The study was funded by the Max-Planck-Society.
1. Mokdad AH, Marks JS, Stroup DF, et al: Actual causes of death in the United States, 2000. JAMA 291:1238-1245, 2004Google Scholar
2. Uhl GR, Grow RW: The burden of complex genetics in brain disorders. Archives of General Psychiatry 61:223-229, 2004Google Scholar
3. Project MATCH Research Group: Matching alcoholism treatments to client heterogeneity: Project MATCH three-year drinking outcomes. Alcoholism, Clinical and Experimental Research 22:1300-1311, 1998Google Scholar
4. Jellinek EM: The Disease Concept of Alcoholism. New Haven, Conn, College and University Press, 1960Google Scholar
5. Penick EC, Nickel EJ, Powell BJ, et al: The comparative validity of eleven alcoholism typologies. Journal of Studies on Alcohol 60:188-202, 1999Google Scholar
6. Verheul R: Co-morbidity of personality disorders in individuals with substance use disorders. European Psychiatry 16:274-282, 2001Google Scholar
7. Krampe H, Stawicki S, Wagner T, et al: Follow-up of 180 chronic alcoholic patients for up to seven years after outpatient treatment: impact of alcohol deterrents on outcome. Alcholism, Clinical and Experimental Research 30:86-95, 2006Google Scholar
8. Bronisch T, Mombour W: The modern assessment of personality disorders: II. reliability and validity of personality disorders. Psychopathology 31:293-301, 1998Google Scholar
9. Gsellhofer B, Küfner H, Vogt M, et al: European Addiction Severity Index—EuropASI. Baltmannsweiler, Germany, Schneider-Verlag Hohengehren, 1999Google Scholar
10. McLellan AT, Kushner H, Metzger D, et al: The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:199-213, 1992Google Scholar
11. DiNardo PA, Barlow DH: Anxiety Disorders Interview Schedule-Revised (ADIS-R). Albany, NY, Graywind Publications, 1988Google Scholar
12. Margraf J: MiniDIPS: Diagnostisches Kurz: Interview bei Psychischen Störungen [in German]. Berlin, Germany, Springer, 1994Google Scholar
13. Derogatis LR: SCL-90-R: Administration, Scoring and Procedures Manual 1. Baltimore, Clinical Psychometrics Research, 1977Google Scholar
14. Franke GH: SCL-90-R: Die Symptom-Checkliste von Derogatis—Deutsche Version. Goettingen, Germany, Beltz Test, 1995Google Scholar
15. Ritsher JB, Moos RH, Finney JW: Relationship of treatment orientation and continuing care to remission among substance abuse patients. Psychiatric Services 53:595-601, 2002Google Scholar



