Factors in the Selection of Patients for Conditional Release From Their First Psychiatric Hospitalization
Involuntary outpatient commitment provisions are explicitly written into mental health law in most Western nations ( 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ). They require that an individual with a mental disorder who refuses care and is believed to be potentially dangerous or in need of health and safety protection accept and comply with community treatment in lieu of involuntary psychiatric hospitalization ( 11 ). Such compliance may extend to requiring people to live in a particular apartment, take prescribed medications, attend counseling sessions, and abstain from substance use ( 1 ). In many jurisdictions individuals who do not comply with a treatment regimen can be admitted to a psychiatric hospital for involuntary care. An involuntary outpatient commitment order may be issued upon an individual's release from a hospital or while the individual is residing in the community. In the first instance, the term often used is "conditional release."
Following on Appelbaum's ( 5 ) suggestion that evidence ( 3 , 4 , 12 ) and clinical experience favor efforts "to implement reasonable schemes of outpatient commitment," this study examined the use of conditional release at the outset of a patient's entry into the treatment system, before the patient experienced extended periods of treatment failure. Use of preventive community outpatient commitment or conditional release in the early stage of illness may offer significant benefits, such as allowing for minimal use of inpatient care, a frequent objective in some progressive catchment areas that seek to emphasize patient-centered treatment ( 13 ). Early use may help caregivers cope with what frequently are untenable situations. Use of either form of outpatient commitment at illness outset, however, is controversial in that it allows little time for voluntary engagement in treatment and may be contrary to legislative intent ( 7 ), because legislation may require repeated evidence of failure of voluntary treatment before use of outpatient commitment ( 14 ).
Although several studies have examined outpatient commitment ( 15 , 16 , 17 , 18 , 19 ), no quantitative investigation has addressed its use at the outset of a person's treatment. Studies tend to focus on long-term deinstitutionalized or "revolving-door" patients ( 1 , 3 , 4 , 16 ). Two of three comparison-group studies ( 1 , 4 , 16 ) did not find differences between patients with repeated hospitalizations who were placed on outpatient commitment and those who were not; one study found positive effects for those whose initial period of outpatient commitment was extended ( 3 , 4 ). Results of four studies without comparison samples are often cited as evidence that outpatient commitment reduces hospital admissions and the duration of hospital stays ( 17 , 18 , 19 , 20 ).
This study examined a decade of experience with the use of outpatient commitment in Victoria, Australia, where the term used is "community treatment orders." In Victoria the public mental health system serves a population of 4.7 million inhabitants. Legislation mandates a prescribed strategy of care, which emphasizes the desirability of community treatment over inpatient treatment and the provision of care in the least restrictive environment ( 21 , 22 , 23 ). (For additional information on the use of community treatment orders in Victoria, see the companion article in this issue [ 24 ].) Since 1986 Victoria has relied on the extensive use of community treatment orders to ensure participation in prescribed care by patients who are believed to be unable to voluntarily accept needed treatment; this treatment approach also relies on aggressive and comprehensive outreach, such as that used in the Program of Assertive Community Treatment model ( 22 ).
In Victoria community treatment orders are issued primarily to facilitate early release from an ongoing inpatient episode, although some orders are issued to individuals who are residing in the community as a way of preventing hospitalization ( 24 ). Conditional release is the most prevalent, oldest, and most traditional approach ( 25 ). The Duke experiment, which investigated the more contemporary and controversial approach in which patients residing in the community are placed on outpatient commitment, showed no short-term difference between patients in the experimental and control groups ( 3 , 4 ). However, when clinicians were permitted to select patients to remain on outpatient commitment for a period longer than the initial term of the order, those patients did better over a longer follow-up period.
The study reported here was not a randomized controlled trial of conditional release. In view of the "selection effect" noted in the Duke experiment, this study explored selection factors for conditional release and attempted to determine whether patients selected for conditional release at the outset of their treatment do better than similar patients who are not selected.
Although the Victorian law makes no specific reference to the use of a community treatment order as an intervention at the outset of treatment, extended observation of the Victorian Mental Health system indicates that orders are being used in this way. This research examined the prevalence of such early use of conditional release and attempted to determine the impact on patients' subsequent use of mental health services.
Methods
The Victorian Psychiatric Case Register (VPCR) provides a record of the characteristics of all clinical contacts that occur in the State of Victoria, Australia. The Victorian Department of Human Services Ethics Committee approved our access to the register data. All patients who were placed on a community treatment order between November 12, 1990, and June 30, 2000—a period when all mental health service use and community treatment orders in Victoria could be reliably mapped using the VPCR—were identified (N=8,879). These patients experienced their first hospitalization during this period. In documenting a patient's treatment experience, all treatment contacts were organized into episodes of care: each hospitalization (from day of admission to day of discharge) was considered a separate inpatient episode; each continuous period of community service provision without a break in service for 90 days was considered a community care episode. No specified frequency of service other than one contact every 90 days was required for categorization as a community care episode ( 26 ). A service break followed by reinitiation of care was considered the start of a new community care episode. All occasions of receipt of community service are reported as community treatment days; multiple community services received on the same day were counted as one community treatment day.
The sample under consideration comprised patients with at least one hospitalization between 1990 and 2000. Of these patients, 7,720 (87 percent) were placed on community treatment orders directly from hospital (conditionally released), 744 (8 percent) experienced both hospital- and community-initiated orders, and 415 (5 percent) experienced only community-initiated orders. Given the primary focus on conditional release in Victoria, we refer throughout this article to placement on community treatment orders as conditional release, although the flexibility of the system allowed for placements on community treatment orders directly from the community. Such placements were carried out when clinicians and oversight officials deemed them necessary.
The analysis first compared two groups of patients: those who were placed on community treatment orders within 30 days of their first service contact with the mental health system (the early-intervention group) and those who completed their first hospitalization within 30 days of system entry but who were not placed on community treatment orders during this period (the early-eligible group). Because the legal standard for placement on a community treatment order is the same as that for hospitalization, the patients in the latter group were eligible for conditional release; however, for some reason this option was not used. The study then compared the early-intervention group and the early-eligible group with later-intervention patients—that is, patients who either did not complete their initial hospitalization within 30 days of entering the mental health system or who were hospitalized at some later point in time and placed on a community treatment order in association with a later hospitalization.
In comparing the three groups—early intervention, early eligible, and later intervention—we attempted to avoid the problem of comparing patients who were selected for conditional release with those who were not selected. All patients were included in the comparison regardless of their legal status at admission to an inpatient episode, because many of those who are conditionally released enter the hospital as voluntary patients. Victorian hospitals rarely accept patients as voluntary unless they show the same disabilities that characterize involuntary patients. Involuntary legal status includes provisions for "security" and "forensic" patients, although these provisions are less frequently invoked than the standard involuntary statute, and such patients are eligible for conditional release. Although we could not distinguish the security and forensic patients from our study data, data from a separate management information system indicated that they represented only .8 percent of all patients placed on community treatment orders and .6 percent (17 cases) of the 2,829 patients in the early-intervention and early-eligible groups, hardly enough to influence study findings.
Between-group comparisons examined services received during the study period and were based on numbers of inpatient episodes, number of inpatient days, days per inpatient episode, and inpatient days per 30 days in the system between 1990 and 2000. Also considered were the number of community treatment contacts and contacts per episode of care in this period.
Lifetime duration of a patient's involvement with the mental health system in days (the "first known system contact" to the last known contact or death) was used as an indicator of severity of condition and a control for possible preperiod service contacts. Although the VPCR indicated that all patients in the sample had their first service contact—hospitalization or community episode—in 1990 or later and that all early-intervention and early-eligible patients had their "first known system contact" in 1990 or later, 57 percent of later-intervention patients had a "first known system contact" before 1990. For this study we considered first service contact as defining entry into the mental health system and "first known system contact" as an indicator of illness onset.
All analyses were completed with the SPSS Statistical Package, version 13 ( 27 ). To avoid redundant statistical testing, univariate descriptive statistics are presented and differences are discussed by inspection. Statistical tests for group differences were used only for the multivariate models. Logistic regression was used to consider from a multivariate perspective the relative importance of factors that distinguished the groups. In developing a model for distinguishing early-intervention patients, indicators of a patient's status at the outset of the initial episode were included that might have been used to justify use of conditional release: patient demographic characteristics (age at date of first contact with the mental health system and gender), the nature of the person's mental disorder (schizophrenia, major affective disorder, paranoia and acute psychosis, and dementia and other nervous system disorders), indicators associated with a poor prognosis (having never been married and receiving government support), indicators associated with a better prognosis (having greater than an 11th grade education [ 28 ]), variables that reflected an individual's community involvement (being employed and being currently married [no other family indicator was available in the data] that may also indicate prognosis [ 28 ]), the severity indicator (lifetime duration of involvement in the treatment system [ 29 ]), and current indicators of inpatient care experience (duration in days of the first inpatient episode and days between first service contact and first inpatient admission).
Ordinary least-squares (OLS) regression procedures were used to consider the impact of early-intervention conditional release on patients' service use. In the OLS models the two comparison groups, dummy coded, were entered as predictor variables (using the SPSS Enter command for simultaneous entry), with the early-intervention group as the contrast. The models included as controls all variables used in the logistic equation distinguishing early-intervention patients from early-eligible patients, community treatment indicators that might have accounted for the effect of the order for conditional release, and the year of the initial inpatient episode, a cohort control. Thus the analyses considered the impact of early intervention, while controlling for all these factors, on four dependent variables: number of inpatient episodes, total number of inpatient days, inpatient days per episode, and inpatient days per 30 days in the mental health system between 1990 and 2000.
As noted above, the conditional release of patients who were admitted voluntarily indicates that although the patients entered the hospital voluntarily, these individuals had a level of disability meeting the criteria required for conditional release. Therefore, eliminating such patients from the analyses would have failed to adequately represent actual early-intervention practice, and controlling for voluntary status in the logistic models may have given priority to legal status and masked factors that were most significant in characterizing the voluntary patients who were selected for conditional release. Although patients with voluntary and involuntary legal status at admission were included, it is necessary to consider the effect of possible differences in the representation of voluntary patients in the study's main comparison groups, because legal status on admission may have accounted for differences in service use that otherwise would be attributed to the early use of conditional release. Thus all models are first presented without the control for legal status at admission, and then the impact of adding legal status at entry to each model is reported.
Results
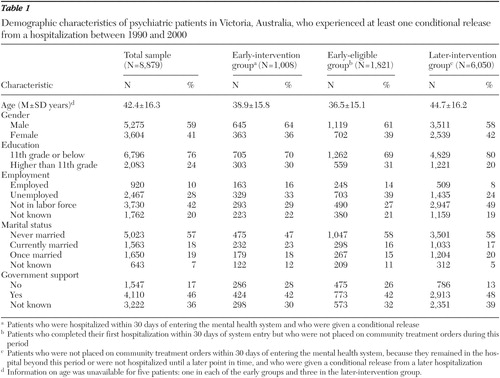
Tables 1 and 2 present data on demographic and diagnostic characteristics and legal status of the 8,879 patients and the three subgroups. A total of 1,008 patients (11 percent) were in the early-intervention group, and 1,821 (21 percent) were in the early-eligible group. The remaining 6,050 patients were in the later-intervention group.
 |
 |
The early-intervention and early-eligible groups were similar in many ways that distinguished them from the later-intervention group. They were younger (36 and 39 years, respectively, compared with 45 years) and more likely to be male (64 and 61 percent, compared with 58 percent) and to have greater than an 11th grade education (30 and 31 percent, compared with 20 percent). They were less likely to be out of the labor force (29 and 27 percent, compared with 49 percent) and less likely to be receiving government support (42 and 42 percent, compared with 48 percent).
The early-intervention group differed from the other two groups primarily in marital status (23 percent of patients were married, compared with 16 percent in the early-eligible group and 17 percent in the later-intervention groups) and diagnostic profile (5 percent had dementia and other nervous system disorders, compared with 8 and 11 percent in the other groups; 70 percent had schizophrenia, compared with 76 and 80 percent; 5 percent had paranoia or acute psychosis, compared with 3 percent and 1 percent; 11 percent had major affective disorder, compared with 10 and 6 percent; and 9 percent had other diagnoses or had no diagnosis recorded at discharge, compared with 4 percent and 2 percent). Finally, the early-intervention group had proportionally fewer voluntary patients at hospital admission (11 percent, compared with 26 percent and 27 percent in the other groups).
Service use and patient treatment experiences
As shown in Table 3 , the three groups were quite different in their use of services. The early-intervention group had a mean of 725 days from first service contact with the treatment system to last contact or death, the early-eligible group had a mean of 1,423 days, and the later-intervention group had a mean of 2,360 days. The early-intervention group had a mean of two inpatient episodes between 1990 and 2000, compared with five episodes for the early-eligible group and five for the later-intervention group—less than half the number of inpatient days and days per episode as the early-eligible group and a third to a quarter of the number of inpatient days and days per episode as the later-intervention group. The early-intervention group also had half the number of community care episodes as the comparison groups—three episodes, compared with six and seven, respectively.
 |
Early-intervention patient selection
Table 4 presents the results of three logistic models distinguishing early-intervention patients (all significant at p<.001). In the first two models the same variables distinguished early-intervention patients from the entire cohort and from the early-eligible group. Furthermore, the relative weight of each of the predictive factors was generally similar in both models. For example, ten years of age was likely to increase the probability of selection to the early-intervention sample from the total sample and from the early-eligible group by 10 percent, being male by 32 percent, being employed between 26 and 29 percent, and being currently married between 27 and 30 percent, though the latter factor distinguished the early-intervention patients from the early-eligible patients but not from the later-intervention patients.
 |
The only distinguishing diagnostic characteristic in both models was dementia or other nervous disorders, which tended to reduce the probability of being in the early-intervention group between 55 and 52 percent in the first two model comparisons. Patients in the early-intervention group were more likely than all other patients to have shorter inpatient episodes on average, but they had a slightly longer initial inpatient episode than the early-eligible patients. They also had a shorter period than the early-eligible patients between first service contact and inpatient admission.
In the third model patients in the early-intervention group differed from later-intervention patients in similar ways on demographic characteristics. They were 55 percent less likely to have a diagnosis of schizophrenia (in this population with a high rate of schizophrenia) and 74 percent less likely to have a diagnosis of dementia or other nervous system disorders. On other indicators patients in the early-intervention group were 53 percent more likely than those in the later-intervention group to be employed, 88 percent more likely to have more than an 11th grade education, 38 percent less likely to have never married, and 21 percent less likely to be receiving government support. They were also more likely to have had a briefer first inpatient episode.
Adding to the model the patient's legal status at inpatient entry did not alter the relationships between any of the characteristics and selection for conditional release in the three models. In the rerun models involuntary status at hospital admission was associated with a 63 percent increase in probability of selection, when compared with the later-intervention patients, all other factors taken into account ( Table 4 ).
Group membership and service use
Table 5 presents four significant (p<.001) multiple regression models comparing the early-intervention group with the other two groups on number of inpatient episodes, number of inpatient days, days per inpatient episode, and inpatient days per 30 days in the mental health system between 1990 and 2000, while the models controlled for the factors included. The findings indicate that the early-eligible group and the later-intervention group had significantly more inpatient experience on each inpatient criterion. In addition, the introduction of legal status into the OLS models did not alter this relationship. In fact, the introduction of legal status indicated that involuntary status at entry was associated with longer hospitalization experiences in all four models and did not alter the effect of early intervention.
 |
Discussion
In this study—given that community treatment days, intensity of community treatment, diagnoses, indicators of better prognosis, and community involvement as well as legal status at hospital admission were all taken into account and found to contribute in the expected direction to inpatient service use—the independent effect of conditional hospital release at the outset of a person's illness appeared to contribute to shortening the person's subsequent involvement with inpatient care.
Although these results seem to justify the use of conditional release early in treatment, there is considerable potential controversy about this approach, as indicated by published clinical guidelines ( 30 ), legislative intent ( 7 ), and statutory objections ( 14 ). In this study early-intervention conditional release accounted for 11 percent of community treatment orders; more that a third of patients who were eligible for early-intervention conditional release received it. Therefore, this study sought to identify characteristics of individuals for whom this intervention was used. Early-intervention patients were distinguished from later-intervention patients by characteristics typically associated with better prognosis. Early-intervention patients were also more likely to have been involuntarily admitted to the hospital, although no information was available on type of involuntary status at admission.
Factors distinguishing patients in the early-intervention group from those in the early-eligible group were less well defined. Possible explanations about how early-intervention patients were selected from patients who were eligible for it are based on fitting clues in the empirical data with observations of system operations and clinical speculation. Such explanations should be considered in the context of the defining characteristics of the entire sample. For example, 78 percent of the overall sample had a diagnosis of schizophrenia, a characteristic that did not distinguish patients in the early-intervention group from those in the early-eligible group, because this diagnosis was common to both groups. Some distinguishing factors were only marginally significant, and no significant interactions in alternate modeling efforts were observed. Therefore, combining significant main effects into hypothetical selection scenarios moves beyond the empirical data, and these hypotheses must be examined in future research.
However, two scenarios are worth future investigation. The first scenario appears to favor individuals with characteristics associated with better prognosis: patients who are older, male, employed, married, and without dementia and who are not willing to accept voluntary hospital admission. The picture is that of a person who has a first episode of illness later in life, after having a chance to become established in adult roles, and who is less likely to see hospitalization as a reasonable treatment option.
A second scenario—a community involvement scenario—is indicated by the association of current marriage and employment with selection for conditional release and with the lack of association with selection of never-married status and educational attainment beyond the 11th grade. The never-married factor is a consistent prognostic indicator, especially for people with schizophrenia, and its failure to distinguish the early-intervention and early-eligible patients seems to point toward an additional consideration in the selection process. The second scenario hypothesizes that there is pressure from the community to get some individuals out of the hospital and back into their social roles as soon as possible after an initial inpatient episode. From the perspective of retaining a person in the hospital, family placement may be considered a legitimate, less restrictive alternative to hospitalization under the law. Consequently, pressure for early release would also come from within the system, because individuals for whom there is an alternative to hospitalization do not technically meet the criteria for involuntary detention—that is, for the health or safety of the person or for community protection in the absence of a less restrictive alternative.
The availability of conditional release legitimizes a family placement as an alternative to hospitalization both in the eyes of hospital staff and community caregivers, because both would be given the responsibility for oversight of the patient. Perhaps the mechanism involved is the potential of conditional release to serve as a contract for patients, hospital staff, and care providers in the community—a contract that promises sufficient oversight outside the hospital to justify caregivers' concerns about early release and the patient's desire to leave the hospital. The finding in this study and others ( 31 , 32 ) that such patients are likely to resist voluntary admission to inpatient care would seem to bear this out. The initial inpatient episode of the early-intervention patients was slightly longer than that of the early-eligible patients, perhaps increasing the pressure to consider alternatives. Conditional release may cover the risk for inpatient staff of allowing a patient to leave an inpatient facility before the concerns about health and safety or community protection that brought the patient to the hospital are fully addressed. Conditional release may also reassure family members that professionals will be available to help them if needed. This mutual-guarantee scenario as an explanation for selection for conditional release seems more probable than a scenario in which patients selected for early release are followed up in the community with more intensive treatment, because the patients who were eligible for early release but not selected had about twice the number of community treatment days after hospital release and an equivalent number of service units per community episode as those who were selected.
It would seem that use of conditional release early in the course of illness holds considerable potential for shortening the duration of subsequent treatment by establishing rapid limits for individuals with better prognoses. Conditional release may address concerns about oversight of patients who are given early hospital discharge to a less restrictive alternative. Although the precise mechanisms remain to be delineated, conditional release early in the course of illness seems to help prevent a revolving-door syndrome of dependency on the hospital as a treatment resource.
The conclusions of this study are tempered by the nature of the data. No information was available about symptom-based severity of illness, parental involvement, and other variables that may have played a role in the decision to use conditional release, such as the availability of community services—like 24-hour emergency response teams. Furthermore, the study did not include a randomly selected comparison group, although the early-eligible patients served as a reasonable comparison. Care must also be taken in interpreting results that are based on administrative data. Although these data probably represent the best source of this type of information, they suffer all the validity problems associated with administrative data.
Conclusions
Although the precise decision mechanisms for selecting patients for conditional release early in the course of illness remain to be delineated in future research, use of this approach seems to help prevent a revolving-door syndrome of dependency on the hospital as a treatment resource. When the analyses controlled for diagnostic and demographic characteristics, illness severity, prognostic factors, and use of community treatment as well as legal status at hospital admission, use of early-intervention conditional release independently contributed to reducing the number of subsequent inpatient episodes, total inpatient days, days per inpatient episode, and days of inpatient care per 30 days in the mental health system. This approach had an independent effect with this patient subgroup as an alternative to hospitalization.
Acknowledgments
The authors thank the National Association for Research on Schizophrenia and Depression and the California Policy Research Center for funding the project, as well as the Australian-American Fulbright Association for making the collaboration possible. The authors extend special thanks to Simon Palmer, M.A., and Ruth Vine, M.B.B.S., F.R.A.N.Z.C.P., as well as colleagues at the Victorian Department of Human Services, the Australian Institute of Health and Welfare, and the Mental Health Research Institute of Victoria.
1. Preston NJ, Kisely S, Xiao J: Assessing the outcome of compulsory psychiatric treatment in the community: epidemiological study in Western Australia. British Medical Journal 324:1244-1246, 2002Google Scholar
2. Torrey EF, Kaplan RJ: A national survey of the use of outpatient commitment. Psychiatric Services 46:778-784, 1995Google Scholar
3. Swartz MS, Swanson JW, Hiday VA, et al: Can involuntary commitment reduce hospital recidivism? Findings from a randomized trial with severely mentally ill individuals. American Journal of Psychiatry 12:1968-1974, 1999Google Scholar
4. Swartz MS, Swanson JW, Hiday VA, et al: A randomized controlled trial of outpatient civil commitment in North Carolina. Psychiatric Services 52:325-329, 2001Google Scholar
5. Appelbaum P: Thinking carefully about outpatient commitment. Psychiatric Services 52:347-351, 2001Google Scholar
6. Power P: Community treatment orders: the Australian experience. Journal of Forensic Psychiatry 10:9-15, 1999Google Scholar
7. Chaimowitz GA: Community treatment orders: an uncertain step. Canadian Journal of Psychiatry 49:577-578, 2004Google Scholar
8. Lefkovitch Y, Weiser M, Levy A: Involuntary outpatient commitment: ethics and problems. Medicine and Law 12:213-220 1993Google Scholar
9. Romans S, Dawson J, Mullen R, et al: How mental health clinicians view community treatment orders: a national New Zealand survey. Australian and New Zealand Journal of Psychiatry 38:836-841, 2004Google Scholar
10. Van Veldhuizen JR: Ambivalence in legislation: outpatient commitment in the Netherlands. Presented at the International Congress on Law and Mental Health, Paris, July 2-8, 2005Google Scholar
11. Allen M, Smith VF: Opening Pandora's box: the practical and legal dangers of involuntary outpatient commitment. Psychiatric Services 52:342-347, 2001Google Scholar
12. Torrey EF, Zdanowicz MT: Outpatient commitment: what, why, and for whom. Psychiatric Services 52:337-341, 2001Google Scholar
13. Segal SP: Managing transitions and insuring good care. Psychiatric Services 55:1205, 2004Google Scholar
14. New York State: Kendra's Law: Final Report on the Status of Assisted Outpatient Treatment. Albany, New York Office of Mental Health, Mar 2005Google Scholar
15. Research Study of the New York City Involuntary Outpatient Commitment Pilot Program (at Bellevue Hospital): Final Report. Delmar, NY, Policy Research Associates, 1998.Google Scholar
16. Steadman HJ, Gounts K, Dennis D, et al: Assessing the New York City involuntary outpatient commitment pilot program. Psychiatric Services 52:330-337, 2001Google Scholar
17. Fernandez GA, Nygard S: Impact of involuntary outpatient commitment on the revolving-door syndrome in North Carolina. Hospital and Community Psychiatry 41:1001-1004, 1990Google Scholar
18. Zanni G, deVeau L: Inpatient stays before and after outpatient commitment in Washington, DC. Hospital and Community Psychiatry 37:941-942, 1986Google Scholar
19. Munetz MR, Grande T, Kleist J, et al: The effectiveness of outpatient civil commitment. Psychiatric Services 47:1251-1253, 1996Google Scholar
20. Rohland B: The role of outpatient commitment in the management of persons with schizophrenia. Iowa City, Iowa Consortium for Mental Health Services, Training, and Research, 1998Google Scholar
21. National Mental Health Report, 1996, Canberra, Commonwealth of Australia Department of Health and Family Services, 1998Google Scholar
22. National Mental Health Report, 1997. Canberra, Commonwealth of Australia Department of Health and Family Services, 1999Google Scholar
23. Mental Health Branch National Standards for Mental Health Services. Canberra, Commonwealth of Australia Department of Health and Family Services, 1997Google Scholar
24. Segal SP, Burgess PM: Conditional release: a less restrictive alternative to hospitalization? Psychiatric Services 57:1600-1606, 2006Google Scholar
25. Ridgely MS, Petrila J, Borum R: The Effectiveness of Involuntary Outpatient Treatment: Empirical Evidence and the Experience of Eight States. Santa Monica, Calif, RAND, 2001Google Scholar
26. Tansella M, Micciolo R, Biggeri A, et al: Episodes of care for first-ever psychiatric patients: a long-term case-register evaluation in a mainly urban area. British Journal of Psychiatry 167:220-227, 1995Google Scholar
27. SPSS 13.0 for Windows. Chicago, SPSS, 2005Google Scholar
28. Zigler E, Phillips L: Social competence and outcome in psychiatric disorder. Journal of Abnormal and Social Psychology 63:264-271, 1961Google Scholar
29. Huntley DA, Cho DW, Christman J, et al: Predicting length of stay in an acute psychiatric hospital. Psychiatric Services 49:1049-1053, 1998Google Scholar
30. Geller JL: Clinical guidelines for the use of involuntary outpatient treatment. Hospital and Community Psychiatry 41:749-755, 1990Google Scholar
31. Kahn P: Use of community treatment orders in the context of community care experiences in Ontario. Presented at the International Congress on Law and Mental Health, Paris, July 2-8, 2004Google Scholar
32. Oluboka OJ Community treatment order: a legal tool to recovery and wellness in the community. Presented at the International Congress on Law and Mental Health, Paris, July 2-8, 2004Google Scholar



