Effects of Attributing Serious Mental Illnesses to Genetic Causes on Orientations to Treatment
Abstract
OBJECTIVE: Professional services for persons with serious mental illnesses are underutilized. The genetics revolution has the potential to increase professional help seeking by increasing biomedical interpretations of mental illness among the public. The objective of this study was to assess whether genetic attributions for serious mental illnesses are associated with more positive orientations to professional treatment among members of the general public. METHODS: Data from two nationally representative surveys were analyzed. First, associations between perceptions of genetic causes of both schizophrenia and depression and treatment recommendations and perceived treatment effectiveness were assessed in a vignette study that was part of the 1996 General Social Survey (GSS). Second, the effect of various descriptions of the role of genetic factors in schizophrenia and depression on perceived treatment effectiveness was assessed in a vignette experiment conducted in 2002-2003. RESULTS: Perception of genetic causes was associated with more recommendations for mental hospitalization and prescription medication but not with more recommendations to see a psychiatrist, a therapist, or a general medical practitioner. Perception of genetic causes was not related to perceived treatment effectiveness in the GSS, and genetic causes as described in the vignette were associated with lower perceived effectiveness of treatment. CONCLUSIONS: Increasing emphasis on genetic causes of mental illnesses may have multifaceted effects on orientations to professional treatment. Genetic attributions appear to direct people's help seeking toward the most extreme or biological forms of intervention, possibly because people view genetically influenced disorders as more serious and chronic. At the same time, such attributions lead to pessimism that intervention will be effective.
Most people who meet criteria for major mental disorders do not seek professional treatment (1,2). Because effective treatments exist for many psychiatric problems, underutilization translates into needless suffering and interference with positive life outcomes (3). Explanations for this underutilization include monetary or other logistical barriers, stigma, and views of mental illness that are inconsistent with psychiatric intervention (1,4,5). Regarding the last point, the congruence between public views of mental illness and the views of the field of psychiatry has increased over the past half century; however, significant discrepancies remain (6,7).
One source of promise for more widespread help seeking is the genetics revolution (8). Genetic research not only is likely to produce new forms of treatment but also may increase biomedical interpretations of mental illness among members of the general public, leading in turn to increased help seeking (9). Some evidence supports this idea. On the basis of vignettes from the MacArthur Mental Health Module of the 1996 General Social Survey (GSS), which describe individuals with schizophrenia, major depressive disorder, alcohol dependence, or cocaine dependence, Schnittker and colleagues (10) found that respondents who attributed the problem described in the vignette to genetic factors were, in general, more likely to recommend professional treatment. Kuppin and Carpiano (11) provided a more nuanced view of these associations by disaggregating Schnittker's professional treatment measure. Kuppin and Carpiano found that genetic attributions were specifically associated with recommendations to check into a psychiatric hospital and use prescription medications but not with recommendations to go to a general physician, a psychiatrist, or a therapist. Thus increased help seeking associated with genetic explanations may be specific to more strictly biological psychiatric interventions.
However, other evidence suggests that the association between genetic explanations of serious mental illness and orientations to professional treatment may be more complicated than the above results would indicate. When a mental illness is attributed to genetic factors, the public perceives the problem as more likely to persist throughout the person's life (12). This finding does not contradict the idea that genetic attributions may increase help seeking. However, it does suggest that people might be more pessimistic about the long-term effectiveness of treatment if the illness is understood in genetic terms.
The analyses by Schnittker and colleagues (10) and Kuppin and Carpiano (11) provide important information about the question of genetic attributions and treatment orientations. The study reported here involved new empirical analyses that refined and expanded the previous ones in several important ways. Both Schnittker and colleagues (10) and Kuppin and Carpiano (11) considered treatment recommendations for several problems, including substance use problems, in pooled analyses. Because the public reacts differently to these problems (8,13) and because we are particularly concerned with treatment seeking for traditionally defined serious mental illnesses, we focused specifically on schizophrenia and major depressive disorder (referred to as depression throughout this article).
In addition, to broaden our understanding of genetic attributions and treatment orientations, we examined not only treatment recommendations but beliefs about treatment effectiveness. Finally, although the MacArthur Mental Health Module provides an excellent source of data on public attitudes about mental illness, it represents a single methodology and has limitations. In particular, because it relies on respondents' own beliefs about genetic causes rather than manipulating causal explanations experimentally, its results are vulnerable to confounding. For example, people who have had more exposure to modern psychiatric thinking may be more likely to endorse both genetic attributions and biological forms of treatment, but without either belief's causing the other one. Thus we also analyzed data from a vignette experiment conducted as part of a separate study—the Genes, Disease, and Stigma study (GDS). As in the GSS, a hypothetical person with schizophrenia or depression is described, but, unlike in the GSS, genetic attribution is experimentally manipulated, and its effect on perceived treatment effectiveness is measured.
Specifically, we report the following data: data from the GSS about the association between respondents' beliefs about genetic causation and both treatment recommendations and perceived effectiveness of treatment for schizophrenia and major depression, and data from the GDS study about the impact of various descriptions of genetic causes on perceptions of treatment effectiveness for schizophrenia and major depression.
Methods
1996 General Social Survey
The GSS is administered biannually, in person, to a nationwide representative sample of adults living in noninstitutional settings. The 1996 survey was conducted between February and May of that year and had a response rate of 76 percent (N=1,444) (13).
A total of 601 respondents were randomly chosen to hear one of the following vignettes. Gender, education (eighth grade, high school, or college), and ethnicity (African American, Hispanic, or white) of the person described in the vignette were also randomly assigned to the respondents. Here we present both the schizophrenia and depression vignettes describing a Hispanic man.
The schizophrenia vignette was as follows: "Juan is a Hispanic man with a college education. Up until a year ago, life was pretty okay for Juan. But then, things started to change. He thought that people around him were making disapproving comments and talking behind his back. Juan was convinced that people were spying on him and that they could hear what he was thinking. Juan lost his drive to participate in his usual work and family activities and retreated to his home, eventually spending most of his day in his room. Juan was hearing voices even though no one else was around. These voices told him what to do and what to think. He has been living this way for six months."
The depression vignette was as follows: "Juan is a Hispanic man with a college education. For the past two weeks Juan has been feeling really down. He wakes up in the morning with a flat heavy feeling that sticks with him all day long. He isn't enjoying things the way he normally would. In fact, nothing gives him pleasure. Even when good things happen, they don't seem to make Juan happy. He pushes on through his days, but it is really hard. The smallest tasks are difficult to accomplish. He finds it hard to concentrate on anything. He feels out of energy and out of steam. And even though Juan feels tired, when nighttime comes he can't go to sleep. Juan feels pretty worthless and very discouraged. Juan's family has noticed that he hasn't been himself for about a month and that he has pulled away from them. Juan just doesn't feel like talking."
The independent variable was perceived genetic causation. Respondents were asked the following question: "In your opinion, how likely is it that Juan's situation might be caused by a genetic or inherited problem?" Possible responses were 1, very or somewhat likely, or 0, very or somewhat unlikely.
The dependent variables were treatment recommendations and perceived effectiveness. To assess treatment recommendations, respondents were asked, "Should Juan (a) go to a general medical doctor for help; (b) go to a psychiatrist for help; (c) go to a therapist or counselor, such as a psychologist, social worker, or other mental health professional, for help; (d) take prescription medication; or (e) check into a mental hospital?" Each treatment option was scored as either 1, yes, or 0, no. Respondents could choose more than one response. To assess perceived treatment effectiveness, respondents were asked, "In your opinion, how likely is it that Juan's situation will improve with treatment?" Possible responses ranged from 1, not likely at all, to 4, very likely.
We controlled for age, gender, race or ethnicity (black, white, or other race), highest degree (less than high school, college, or graduate degree), and vignette condition (schizophrenia or depression).
Genes, Disease, and Stigma Study
In the GDS study, a random-digit-dial telephone survey targeted adults who lived in households with telephones in the continental United States. Interviews, averaging 20 minutes in duration, were conducted with 1,241 respondents between June 2002 and March 2003. This sample size reflected a 62 percent response rate. All results are weighted to account for poststratification adjustment to national counts by race or ethnicity and differential selection probabilities.
A total of 601 respondents were randomly chosen to hear one of the vignettes described below. Cause of illness (the independent variable of interest) was also randomly assigned to respondents. To improve the generalizability of the findings, the gender, socioeconomic status, and diagnosis (schizophrenia or depression) of the person described in the vignette were also randomly varied. We thought that introducing cross-ethnicity judgments—for example, having white respondents hear vignettes describing a black person and vice versa—would create a complexity that could be analyzed only with a larger sample than the one that was available to us. In addition, we feared that omitting the race or ethnicity of the person described in the vignette would invoke stereotypes about race and mental illness that could affect responses in unmeasurable ways. Thus we matched the race or ethnicity of the person described in the vignette to that of the survey respondent. Here we present the vignette describing a white woman.
One of the schizophrenia vignettes follows: "Anne is a single 25-year-old white woman. Anne went to college for two years and then took a job. Since then, she has been steadily employed and makes a good living. Usually, Anne gets along well with her family and coworkers. She enjoys reading and going out with friends. About a year ago, Anne started thinking that people around her were spying on her and trying to hurt her. She became convinced that people could hear what she was thinking. She also heard voices when no one else was around. Sometimes she even thought people on TV were sending messages specially to her. After living this way for about six months, Anne was admitted to a psychiatric hospital and was told that she had an illness called schizophrenia. She was treated in the hospital for two weeks and was then released. She has been out of the hospital for six months now and is doing OK. Now, let me tell you something about what caused Anne's problem. When she was in the hospital, an expert in genetics said that Anne's problem was due to genetic factors. In other words, her problem had a very strong genetic or hereditary component."
The schizophrenia vignettes varied in the level of education and economic success described for Anne and the degree to which her illness was attributed to genetic factors. In the second version of the vignette, the expert said, "not due to genetic or hereditary factors." In the third version, the expert said that Anne's problem was partly due to genetic or hereditary factors.
The depression vignette was identical to the above except for the description of Anne's problem: "About a year ago, Anne started feeling very down and unhappy. She found it very hard to get out of bed, get dressed, go to work, or do anything. She just didn't get any pleasure out of anything the way she normally would. She often didn't feel like eating, and she had trouble sleeping. Anne also felt completely worthless and even had thoughts about killing herself. After having these problems off and on for about six months, Anne was admitted to a psychiatric hospital and was told that she had an illness called major depressive disorder."
Again, genetic attribution (the independent variable) was experimentally manipulated. Respondents were randomly assigned to hear one of three causal statements. We dichotomized genetic attribution as 1, genetic or partly genetic, or 0, not genetic.
Perceived treatment effectiveness (the dependent variable) was assessed with the question, "In your opinion, how likely is it that a mental health professional, like a psychiatrist, psychologist or social worker can help with problems like Anne has?" Possible responses ranged from 1, not likely at all, to 4, very likely.
The illness described in the vignette (schizophrenia versus depression) was the control variable. Perceived persistence was used as a potential mediating variable. To assess perceived persistence, respondents were asked, "In your opinion, how likely is it that Anne will continue to have problems like the ones I described for her whole life?" Possible responses ranged from 4, very likely, to 1, not likely at all.
Because we are interested in the consequences of believing a mental illness is genetically influenced, we limited the analysis to the 426 respondents (71 percent) who, at the end of the interview, correctly recalled the cause of the problem as described by the expert and agreed with the expert's statement. This approach modifies the random assignment of the independent variable and can introduce confounding. However, in the reduced sample, sociodemographic variables were not significantly associated with the independent variable (genetic attribution), which reduced concerns about confounding.
Results
Treatment recommendations
As can be seen from Table 1, respondents who thought genetic factors contributed to the problem were no more likely to recommend that the individual described in the vignette see a psychiatrist, a therapist, or a general medical practitioner but were significantly more likely to recommend prescription medication (p<.001) and psychiatric hospitalization (p<.01). When other causal beliefs were controlled for, as in previous analyses of these data (10,11), the results were similar but weaker: p<.05 for prescription medication and psychiatric hospitalization. Perceived genetic causes approximately doubled the odds that medication and psychiatric hospitalization would be recommended. We also entered interaction terms to assess whether the associations between perceived genetic causes and treatment recommendations differed for schizophrenia and depression, but they did not.
Perceived treatment effectiveness
The GSS. As can be seen from Table 2, belief in genetic causes was not significantly associated with the belief that the problem would improve with treatment. The association between perceptions of genetic causes and treatment effectiveness did not differ significantly for schizophrenia and depression.
The GDS study. As can be seen in Table 3 (model 1), genetic attribution significantly decreased (p<.05) optimism that a mental health professional could help with the problem. Again, the association between genetic attribution and perceived treatment effectiveness did not differ significantly for schizophrenia and depression.
To this point, our results suggest that genetic attributions for a serious mental illness are related to increased recommendations for certain types of professional treatment but are not related to optimism about treatment success. In fact, in the GDS study, genetic attribution significantly reduced optimism about treatment. We next present data that may help explain the coexistence of these two sets of findings.
Model 2 in Table 3 shows that when the perception that the problem was a chronic one was added as a potentially mediating variable, the coefficient for genetic attribution was reduced by 10 percent, indicating that pessimism about treatment effectiveness may be partly explained by the expectation that a genetically influenced illness will continue throughout life.
Discussion and conclusions
This study was motivated by concerns about underutilization of professional treatment for serious mental illnesses and the role that the genetics revolution might play in increasing help seeking. Two previous studies suggested that genetic explanations might increase at least some forms of professional help seeking (10,11) for mental disorders, defined broadly to include substance use disorders. Focusing on schizophrenia and depression, we assessed the relationship between genetic causal attributions and orientation to professional treatment as fully as we could with available data. Specifically, we used two data sets that employed different designs and measures: a vignette experiment (the GDS study) and a nonexperimental vignette study (the GSS), both embedded in nationally representative surveys.
Our results support the idea that genetic attributions may increase certain types of help seeking—the extreme response of psychiatric hospitalization and the purely biomedical approach of medication—but not consultation with any type of mental health or medical professional (a psychiatrist, a therapist or counselor, or a general medical practitioner). Moreover, when it came to judgments about whether professional help would ameliorate the problem, genetic attributions either had no bearing on optimism about treatment effectiveness or reduced such optimism. In the nonexperimental GSS, the two variables were unrelated, and when genetic attribution was experimentally manipulated in the GDS study, it led to significantly greater pessimism about the ability of a mental health professional to help with the problem. Data from the GDS vignette experiment suggested that pessimism about treatment effectiveness might in part be explained by the belief that genetic factors increase the life-long nature of the problem. All these patterns held for both schizophrenia and depression: No significant interactions were noted between genetic cause and the type of disorder described in the vignettes.
One limitation of both studies is the possibility that real-life reactions to real people would differ from reactions to hypothetical people described in vignettes. However, although many factors influence actual help seeking, it seems likely that the beliefs and orientations observed here would be among those factors. The two data sets differ in several ways and have different strengths and limitations. Both vignette studies, embedded in nationally representative surveys, have good external validity properties. A vignette experiment in which genetic attribution is randomly assigned to respondents has stronger internal validity properties. This stronger internal validity, along with the fact that the GDS study is more current, leads us to place greater weight on those results, which suggest greater pessimism about treatment effectiveness.
However, we know from the GSS data that the types of treatment specified in the GDS question about treatment effectiveness (seeing a mental health professional, such as a psychiatrist, a psychologist, or a social worker) are not the types whose endorsement are most likely to be associated with belief in genetic causes. Thus if the GDS question had specified psychiatric hospitalization or prescription medication, expectations of treatment effectiveness under genetic-cause conditions may not have been as negative. Although the specific results varied somewhat between the studies, the fact that dual methods were used makes it plausible that the true state of affairs lies somewhere within the range of results obtained: Genetic attributions are associated with more recommendations for biomedical and powerful forms of intervention, but expectations that intervention will be effective are either negatively affected or not affected at all by genetic attributions.
Although we did not have all the necessary data to allow us to fully explain the pattern of results observed, the findings of our study are consistent with the following scenario: When a serious mental illness such as schizophrenia or depression is believed to have genetic roots, the problem is seen as a more serious, life-long, and chronic problem (12,14). The perceived seriousness induced by genetic attributions leads to a tendency to seek interventions that are viewed as the most powerful. At the same time, the perceived intractability of a genetic problem leads to pessimism that even these powerful treatments will be effective in the long run. People may believe that the individual must try the most potent treatment possible even though this treatment probably will not be totally effective. Elements of this scenario are supported by findings that deal with a variety of physical and psychiatric problems. House (15) found that psychiatric outpatients who had internal attributions for their problems perceived the problem as more severe, as likely to last longer, and as requiring more extensive treatment. Similarly, Cunningham and colleagues (16) found that people who accepted a disease model of alcoholism thought the problem was more serious, thought treatment was more necessary for recovery, and were more skeptical that recovery was possible. Finally, Weiner and colleagues (17) found that medical treatment was expected to be more effective for physical illnesses that were viewed as more reversible.
If this scenario is correct, it is difficult to predict the impact of the genetics revolution on overall help seeking for mental health problems. One effect that seems likely, on the basis of the GSS findings, is that if genetic explanations become more prominent, help seeking may shift from psychotherapeutic interventions toward more extreme or biomedical interventions, such as psychiatric hospitalization and medication. This possibility is also supported by studies by Whittle (18) and by Isselin and Addis (19), who found that belief in biological causes was related to belief in the importance of and likely effectiveness of more biological treatments for major mental illnesses in clinical and nonclinical samples. Another possibility that must be considered is that, if genetic attributions reduce the expectation of successful treatment, they may lead to a self-fulfilling prophecy of lower actual effectiveness (20,21).
Our results caution against prematurely accepting a connection between genetic attributions and more positive orientations to professional help seeking for serious mental illnesses. Because there is every indication that genetic explanations for mental illnesses will increase in the future—because both studies suggest that genetic attributions are related to beliefs about treatment—and because inadequate treatment seeking for mental health problems is such an important problem, further research should attempt to more fully explain how the ongoing genetics revolution may affect orientations to professional treatment for serious mental illnesses.
The authors are affiliated with the department of sociomedical sciences of Columbia University, 722 West 168th Street, 9th floor, New York, New York 10032 (e-mail, [email protected]).
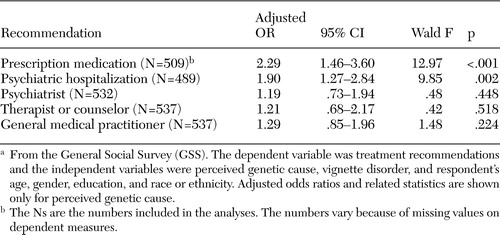 |
Table 1. Logistic regressions of data on recommendations for a hypothetical person with schizophrenia or depression whose illness was described as being caused by genetic factorsa
a From the General Social Survey (GSS). The dependent variable was treatment recommendations and the independent variables were perceived genetic cause, vignette disorder, and respondents age, gender, education, and race or ethnicity. Adjusted odds ratios and related statistics are shown only for perceived genetic cause.
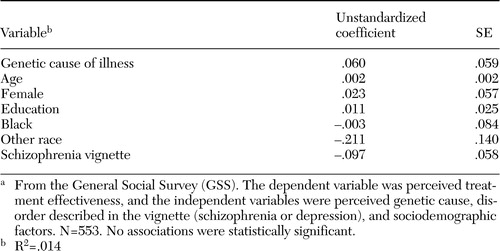 |
Table 2. Linear regression of variables related to perceived treatment effectiveness for a hypothetical person with schizophrenia or depressiona
a From the General Social Survey (GSS). The dependent variable was perceived treatment effectiveness, and the independent variables were perceived genetic cause, disorder described in the vignette (schizophrenia or depression), and sociodemographic factors. N=553. No associations were statistically significant.
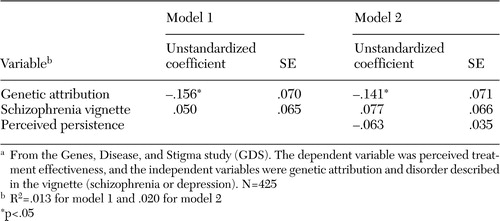 |
Table 3. Linear regression of variables related to perceived treatment effectiveness for a hypothetical person with schizophrenia or depressiona
a From the Genes, Disease, and Stigma study (GDS). The dependent variable was perceived treatment effectiveness, and the independent variables were genetic attribution and disorder described in the vignette (schizophrenia or depression). N=425
1. Kessler RC, Berglund PA, Bruce ML, et al: The prevalence and correlates of untreated serious mental illness. Health Services Research 36:987–1007,2001Medline, Google Scholar
2. Robins L, Regier DA: Psychiatric Disorder in America: The Epidemiological Catchment Area Study. New York, Free Press, 1991Google Scholar
3. Bovasso GB, Eaton WW, Armenian HK: The long-term outcomes of mental health treatment in a population-based study. Journal of Consulting and Clinical Psychology 67:529–538,1999Crossref, Medline, Google Scholar
4. Corrigan P: How stigma interferes with mental health care. American Psychologist 59:614–25,2004Crossref, Medline, Google Scholar
5. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md, US Department of Health and Human Services, Public Health Service, Office of the Surgeon General, 2001Google Scholar
6. Star S: The public's ideas about mental illness. Presented at the annual meeting of the National Association for Mental Health, November 5, 1955, IndianapolisGoogle Scholar
7. Link BG, Phelan JC, Bresnahan M, et al: Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American Journal of Public Health 89:1328–1333,1999Crossref, Medline, Google Scholar
8. Hyman SE: The millennium of mind, brain, and behavior. Archives of General Psychiatry 57:88–89,2000Crossref, Medline, Google Scholar
9. Conrad P: Medicalization, genetics, and human problems, in Handbook of Medical Sociology, 5th ed. Edited by Bird CE, Conrad P, Fremont AM. Upper Saddle River, NJ, Prentice Hall, 2000Google Scholar
10. Schnittker J, Freese J, Powell B: Nature, nurture, neither, nor: black-white differences in beliefs about the causes and appropriate treatment of mental illness. Social Forces 78:1101–1132,2000Crossref, Google Scholar
11. Kuppin S, Carpiano R: Public conceptions of mental illness and substance abuse, its causes and treatments: findings from the 1996 General Social Survey. American Journal of Public Health, in pressGoogle Scholar
12. Phelan JC: Geneticization of deviant behavior and consequences for stigma: the case of mental illness. Journal of Health and Social Behavior 46:307–322,2005Crossref, Medline, Google Scholar
13. Pescosolido BA, Monahan J, Link BG, et al: The public's view of the competence, dangerousness, and need for legal coercion among persons with mental health problems. American Journal of Public Health 89:1339–1345,1999Crossref, Medline, Google Scholar
14. Phelan JC, Cruz Rojas R, Reiff M: Genes and stigma: the connection between perceived genetic etiology and attitudes and beliefs about mental illness. Psychiatric Rehabilitation Skills 6:159–185,2002Crossref, Google Scholar
15. House WC: Outpatients' attributions of the causes of their psychological problems. Journal of Psychology 108:81–84,1981Crossref, Medline, Google Scholar
16. Cunningham JA, Sobell LS, Sobell MB: Are disease and other conceptions of alcohol abuse related to beliefs about outcome and recovery? Journal of Applied Social Psychology 26:773–780,1996Google Scholar
17. Weiner B, Perry R, Magnusson J: An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology 55:738–748,1988Crossref, Medline, Google Scholar
18. Whittle P: Causal beliefs and acute psychiatric hospital admission. British Journal of Medical Psychology 69:355–370,1996Crossref, Medline, Google Scholar
19. Iselin MG, Addis ME: Effects of etiology on perceived helpfulness of treatments for depression. Cognitive Therapy and Research 27:205–222,2003Crossref, Google Scholar
20. Merton RK: The self-fulfilling prophecy, in Social Theory and Social Structure. Edited by Merton RK. New York, Free Press, 1968Google Scholar
21. Rosenthal R, Jacobson L: Pygmalion in the Classroom: Teacher Expectations and Pupils' Intellectual Development. New York, Holt, Rinehart and Winston, 1968Google Scholar



