Comparison of ACT and Standard Case Management for Delivering Integrated Treatment for Co-occurring Disorders
Abstract
OBJECTIVE: Clients with co-occurring severe mental and substance use disorders are at high risk of institutionalization and other adverse outcomes. Although integrated mental health and substance abuse treatment is becoming a standard clinical approach for such clients, the optimal method for delivering integrated treatment remains unclear. METHOD: This study compared integrated treatment delivered within two different models of community-based case management (assertive community treatment and standard clinical case management). A total of 198 clients in two urban sites who had co-occurring disorders and were homeless or unstably housed were randomly assigned to one of two treatment conditions and were followed for three years. RESULTS: Participants in both treatment conditions improved over time in multiple outcome domains, and few differences were found between the two models. Decreases in substance use were greater than would be expected given time alone. At the site that had higher rates of institutionalization, clients who received standard case management were more likely to be institutionalized. However, in the site that had lower rates of institutionalization, no differences in the rate of institutionalization were found between the two treatment conditions. CONCLUSIONS: Integrated treatment can be successfully delivered either by assertive community treatment or by standard clinical case management.
Individuals with severe mental illnesses, such as schizophrenia and bipolar disorder, often abuse alcohol and drugs, with lifetime rates of substance use disorder of approximately 50 percent (1,2) and rates of current substance use disorder of approximately 30 percent (3). For individuals with severe mental illness, substance use disorder is related to a wide range of negative outcomes, including increased risk of relapse and rehospitalization, homelessness, incarceration, violence, family burden, economic hardship, infectious diseases, and higher treatment costs (4,5,6,7). Because of the recognition over the past 25 years of the high prevalence of substance use disorders among people with severe mental illness and because of the havoc that substance use disorders play on their lives, developing effective treatment approaches for individuals with co-occurring disorders has become a priority.
Since the 1980s clinicians and researchers have been aware of the ineffectiveness of treating mental health and substance use disorders with parallel and sequential treatments in separate systems (8,9,10,11). Therefore, a variety of approaches for integrating interventions have been developed, ranging from brief motivational interventions to long-term residential programs (12,13,14,15). Integrated models of treatment emphasize the importance of treating both the mental illness and the substance use disorder at the same time by the same clinician or team of clinicians in an integrated, seamless manner (12,13,15,16). These models also frequently incorporate assertive outreach to engage individuals in treatment, and they eschew confrontational approaches in favor of interventions that are intended to instill motivation to change, such as motivational interviewing (17).
Integrated treatment has been the focus of a growing body of research in recent years, with nearly 30 controlled studies reported between 1994 and 2004 (18). Although many studies have been limited by methodological problems, such as lack of random assignment or failure to measure substance use or mental health outcomes, results in general have been promising. Among randomized controlled trials that compared at least three sessions of integrated outpatient treatment with nonintegrated care, five studies reported better substance use outcomes for the group that received integrated treatment (19,20,21,22,23), one study reported better substance use outcomes for the group that received integrated treatment at 12 but not 18 months (although mental health outcomes favored the group that received integrated treatment at both follow-up points) (24,25), and one study reported no differences between the two conditions (26). Quasi-experimental studies of integrated outpatient treatment have reported similar results supporting integrated over nonintegrated care (27,28,29), although studies of integrated day treatment programs have produced more mixed results (30,31).
Although agreement is not unanimous that integrated treatment is superior to parallel or sequential approaches (32), the approach has garnered significant support and is widely accepted to be an evidence-based practice for persons with severe mental illness (33,34). Policy makers and clinicians have endorsed the use of integrated treatment (34,35,36,37), even as the details and specific forms of integrated treatments remain in development and are being tested (18,38,39). A central remaining question concerns how integrated treatment should be provided—that is, what model of case management is most effective for delivering integrated treatment services?
Because of the strong evidence base for the assertive community treatment model, it deserves special consideration (40,41,42). The model is distinguished from standard clinical case management because of its lower staff-to-client ratio (1:10 to 1:15 for assertive community treatment compared with 1:25 or higher for standard clinical case management), the delivery of most services in the community (rather than the clinic), shared caseloads (rather than an individual caseload for each clinician), 24-hour responsibility for clients, and direct provision of most services (rather than the brokering of services to other providers). The assertive community treatment model was developed for individuals with severe mental illnesses who tend not to use outpatient psychiatric services at their local community mental health centers, who are prone to frequent relapses and rehospitalizations, and who have severe psychosocial impairment. Assertive community treatment has been studied extensively; results from more than 30 randomized controlled trials have demonstrated beneficial effects, such as reduced hospitalizations (the most consistent finding), reduced symptoms, increased housing stability, better quality of life, and greater satisfaction with treatment (43,44,45,46,47,48).
The evidence base clearly supports the effectiveness of assertive community treatment in reducing psychiatric hospitalizations among individuals who are heavy users of hospital services. Assertive community treatment may be more effective than standard clinical case management for delivering integrated services, because clients with co-occurring disorders tend to be hospitalized more frequently (49). Additionally, treating individuals with co-occurring disorders is associated with higher costs (4,50), and assertive community treatment has been found to reduce treatment costs for high service utilizers (48,51,52). At the same time, the studies and reviews cited above document that well-implemented clinical case management can be as beneficial as assertive community treatment in many domains.
Because of the mounting evidence indicating that integrated treatment is more effective than parallel treatment for mental and substance use disorders and because assertive community treatment is cost-effective for clients with severe mental illness who are high service utilizers, two remaining questions face system administrators: What additional benefits, if any, are gained by using assertive community treatment to treat clients with co-occurring disorders? And what would these additional benefits cost? Benefits may include improvements in psychiatric symptoms, reduction or cessation of substance use, increased housing stability, decreased involvement with the criminal justice system, and increased employment. Determining the cost of these benefits is important because implementing and sustaining evidence-based practices—such as assertive community treatment and integrated services—consumes resources, and administrators need to know how to best invest their limited service dollars.
Only one controlled study has specifically compared assertive community treatment and standard clinical case management for delivering integrated treatment (46). This study, conducted in New Hampshire, which is predominantly rural, found that clients in both groups improved on substance use, mental health, and housing outcomes and that assertive community treatment demonstrated statistically significant but clinically modest benefits over standard clinical case management on alcohol use outcomes. Furthermore, within the assertive community treatment model, clients at sites that followed treatment model faithfully had much better outcomes than clients at sites with lower fidelity to the treatment model (53).
An earlier analysis compared baseline data from the study presented here—the Connecticut Co-occurring Disorders Study, which examined individuals in urban areas—with baseline data from the New Hampshire study, which examined individuals in rural areas (46). The study found that individuals in the Connecticut Co-occurring Disorders Study tended to have higher rates of drug use, more housing instability, and more legal system involvement than individuals in the New Hampshire study (54). These differences suggest that clients with co-occurring disorders who live in urban areas may benefit more from assertive community treatment than from standard clinical case management. We conducted a randomized trial that compared assertive community treatment with standard clinical case management for clients with co-occurring disorders.
Methods
The Connecticut Co-occurring Disorders Study was a randomized controlled study that compared two types of case management—assertive community treatment and standard clinical case management—among individuals with co-occurring mental and substance use disorders who received integrated treatment. The study took place at two state-operated outpatient community mental health centers in urban areas of Connecticut that had a large population of residents with income below the poverty line. Assertive community treatment and standard clinical case management services were well established before the study began. However, at start up, two study authors (KM and RD) provided training and technical assistance in implementing integrated treatment.
Participants
Clients were eligible for the study if they had a major psychotic disorder (schizophrenia, schizoaffective disorder, bipolar disorder, or major depression with psychotic features); had an active substance use disorder (abuse or dependence on alcohol or other drugs within the past six months); had high service use in the past two years (two or more of the following: psychiatric hospitalizations, stays in a psychiatric crisis or respite program, emergency department visits, or incarcerations); were homeless or unstably housed; had poor independent living skills; did not have any pending legal charges, medical conditions, or mental retardation that would preclude participation; were scheduled for discharge to community living if they were an inpatient; and were willing to provide written informed consent. (Detailed operational criteria are available from the authors.) We enrolled study participants between August 1993 and July 1998 and followed each study participant for three years.
Programs
Assertive community treatment teams at both study sites were implemented in a previous study by the authors by using a model-guided process of supervision and training (48). Training by study authors (KM and RD) emphasized the essential features of assertive community treatment, as described above. Training also included key components of integrated treatment: direct substance abuse treatment by members of the team, use of a stagewise co-occurring disorders model, treatment groups for clients with co-occurring disorders, and an exclusive team focus on clients with co-occurring disorders (55).
Standard clinical case management teams were composed of clinicians from different disciplines and emphasized a team approach, wherein team members carried individual caseloads but discussed clients and reviewed cases together. As with the assertive community treatment model, the standard clinical case management model delivered at least some services in the community, had clinicians work with the clients' support systems, and vigorously addressed substance use disorders. Because clinicians in the standard clinical case management group had caseloads of approximately twice as many clients as clinicians in the assertive community treatment group, they provided fewer services directly. Both assertive community treatment and standard clinical case management teams received regular training and supervision from study authors (KM and RD) in integrated treatment, including comprehensive assessment, individual motivational interviewing, group treatments, and stagewise interventions (14).
Measures
All of the research interviewers were clinicians, who were trained with videotapes and were paired with seasoned interviewers (clinicians who had conducted interviews for the New Hampshire study for at least three years) before working independently. Ongoing supervision by seasoned interviewers from the New Hampshire study included review of audiotaped interviews and training conferences.
The clinical interviewers established diagnoses of co-occurring severe mental and substance use disorders with the Structured Clinical Interview for DSM-III-R (56). At baseline, the research interview included items from the Uniform Client Data Inventory to assess demographic information (57); the Timeline Follow-Back to assess days of alcohol and drug use over the previous six months (58); the medical, legal, and substance use sections from the Addiction Severity Index (59); detailed chronological assessment of housing history and institutional stays by using a self-report calendar supplemented by outpatient records and hospital records for the year before baseline (60); the Quality of Life Interview to assess objective and subjective dimensions of quality of life (61); and the Expanded Brief Psychiatric Rating Scale to assess psychiatric symptoms over the past two weeks (62).
Follow-up interviews included the same instruments, although they did not reassess demographic and lifetime information. Case managers also provided weekly information on nights spent in nursing homes, hospitals, shelters, jails, and respite units and whether the client stayed with friends, with relatives, or at another place because of a crisis or whether the client had no place to stay.
To increase the validity of self-reported substance use, we supplemented interview data with laboratory measures and clinician ratings. At each assessment point, we conducted urine toxicology screens to detect drugs of abuse and collected saliva swabs to detect alcohol. Case managers rated clients every six months on three rating scales: the Alcohol Use Scale (AUS), the Drug Use Scale (DUS), and the Substance Abuse Treatment Scale (SATS). The AUS and the DUS are 5-point scales that are based on DSM-III-R criteria for severity of substance use disorder; a score of 1 indicates abstinence; 2, use without impairment; 3, abuse; 4, dependence; and 5, severe dependence (63). The SATS is an 8-point scale that indicates progressive movement toward treatment involvement, remission, and recovery from substance use disorders (64). Independent raters, blind to the study condition, considered all available data on substance use to establish consensus ratings on all three scales, with good demonstrated reliability (65). Remission was defined as a score of less than 3 on both the AUS and the DUS, which indicated no use or use without problems during the previous six months.
We also obtained information on service use from the state management information systems, including Medicaid claims data; data on time spent in correctional facilities were from the state Department of Corrections database.
Procedures
The protocol was approved by the institutional review boards of the Connecticut Department of Mental Health and Addiction Services, the Southwest Connecticut Mental Health System, Dartmouth College, and the University of Connecticut. Case managers identified and referred clients who had co-occurring mental and substance use disorders and who met the criteria for being a high service user. After providing written informed consent for the research procedures, study participants completed baseline assessments and were randomly assigned within the two sites to either assertive community treatment or standard clinical case management. Randomization was managed centrally by using separate computer-generated randomization streams for each site. At study entry (baseline) and every six months throughout the three-year follow-up, researchers assessed each participant by conducting urine toxicology tests and alcohol saliva swab tests, administering 1.5-hour structured interviews, and collecting clinician ratings of substance use. Participants received $15 for each interview and an additional $5 for each urine and saliva sample that they provided.
Statistical analyses
We used SAS to conduct most of the statistical analyses. Exceptions were using SPSS to analyze total institutional days and fidelity to assertive community treatment and using MIXOR to examine institutional days through time. We assessed whether the two treatment groups and the two sites were equivalent at baseline by using analysis of variance and chi square tests. Similar methods were used to compare persons who dropped out of the study with those who completed it. We evaluated longitudinal outcomes with mixed-effects regression models (66,67). We treated time as a continuous variable, on the basis of interview month, whereby single-subject lines were fit over time and group trajectories were interpreted (68). Because plots of some of the outcomes over time showed curvilinear patterns, we fit models with both linear and quadratic time effects. To handle correlations among repeated assessments, we left the covariance matrix unstructured. We evaluated treatment effects primarily through the group-by-time interactions, because the equivalent groups at baseline were expected to diverge over time, and we included site as a factor in all analyses.
For substance use, we first examined five dimensional measures: researchers' ratings on the SATS, AUS, and DUS and clients' reports of days of alcohol and drug use on the six-month Timeline Follow-Back calendar. We applied log transformation to days of use, because these variables were highly skewed. We analyzed SATS ratings for all clients, because this scale includes both alcohol and drug use within the single rating. For other substance use outcomes, we analyzed clients with an alcohol use disorder or a drug use disorder separately. That is, when examining outcomes related to alcohol use, we selected only the clients who were given a diagnosis of an alcohol use disorder at baseline, and when examining outcomes related to drug use, we selected only those who were given a diagnosis of a drug use disorder at baseline. Some clients had both alcohol and drug use disorders. In addition to random regression models, we examined institutional outcomes (that is, hospital and incarceration days) by using nonparametric tests (Mann-Whitney U) to compare the two treatment conditions on cumulative institutional days over the three-year study.
Results
Of the 382 clients who were referred by their clinicians, 244 met screening criteria and were eligible for the study. A total of 215 consented to join the study, and 205 completed the baseline interview and were randomly assigned to one of the treatment groups within the two sites. Seven of these clients left the study for different administrative reasons (were given an early transfer to a forensic team, were given a different diagnosis upon re-evaluation, moved out of state, or refused to accept treatment assignment). Thus the study group size was 198, with 99 participants randomly assigned to each condition.
Overall, the study group was predominantly male (142 participants, or 72 percent), young (mean±SD of 36.5±7.8 years), unemployed (178 participants, or 90 percent), from a racial or ethic minority group (108 African Americans, or 55 percent; 28 Hispanics, or 14 percent; and seven participants from another minority group, or 4 percent). Most of the group had never been married (145 participants, or 73 percent). Approximately half the sample (98 participants, or 49 percent) were high school graduates. Most were given a diagnosis of schizophrenia or schizoaffective disorder (151 participants, or 76 percent), and others had mood disorders (33 participants, or 17 percent) or other axis I disorders (12 participants, or 6 percent). Alcohol use disorder (147 participants, or 74 percent) was only slightly less common than disorders involving other substances (161 participants, or 81 percent).
During the three years of the study, 19 of the original 198 clients (10 percent) were lost to follow-up: five withdrew from the study or refused to participate, six died, and eight relocated to other states without further contact. The remaining 179 clients (90 percent) participated in the research assessments every six months for three years, with 145 (73 percent) completing every assessment. Completion rates for individual follow-ups ranged from 86 to 90 percent and did not differ by treatment group. These completion percentages include in the denominator all participants, including those who died during the study, and hence they are conservative.
Attrition and group comparability
As shown in Table 1, we compared the assertive community treatment and standard clinical case management groups at baseline on several variables: demographic, psychiatric, and clinical characteristics; quality of life; alcohol and drug use; and residential status. The two treatment groups differed significantly on clinician's rating of substance use (p<.05). The assertive community treatment group was rated by clinicians as having less treatment involvement toward remission and recovery from substance use, corresponding to lower ratings on the Substance Abuse Treatment scale, compared with the standard clinical case management group. Also, differences between the two sites were found at baseline on a number of variables in the demographic and substance use domains (Table 2), but we did not find any interactions between the treatment condition and site.
As shown in Table 2, demographic differences were found at baseline between the two sites. Compared with site 2, site 1 had more whites and fewer African Americans, more individuals who were married, and more individuals with affective diagnoses. In the year before the baseline interview, clients at site 1 also reported more hospitalization and reported less time in stable housing. Individuals in site 1 also displayed somewhat greater alcohol use symptoms and, hence, were in an earlier stage of treatment than those in site 2. Because attrition was low and because mixed-effects regression procedures use all available data, few data were missing and no statistical differences were found between the recruited and retained study groups.
Fidelity to the assertive community treatment model
To ensure high fidelity to the assertive community treatment model and to check that the standard clinical case management model was offering a distinct service, throughout the study we regularly reviewed data from the management information systems. Specifically, we considered the integrity of contacts (that is, frequency and duration); shared caseload (the extent to which clients received services from multiple team members); and mobility of the team (the percentage of time spent in community locations).
Although one of the assertive community treatment teams spent less time in the community than ideal, the assertive community treatment teams were generally very faithful to the model, and the two treatment groups were distinct from each other. For example, at site 1, clients who were assigned to the assertive community treatment team received significantly more of their services in the community per month (mean percentage of monthly contact for the first 12 months: 47±19 percent for the assertive community treatment team compared with 10±11 percent for the standard clinical case management team; Mann-Whitney U=98, p<.001). At site 2, clients assigned to the assertive community treatment team averaged 19±19 percent of their services in the community per month for the first 12 months and clients assigned to the standard clinical case management team averaged 13±15 percent, although this difference was not significant.
Longitudinal outcomes
Tables 3 and 4 show the mixed-effects regression results. Overall, there were few statistically significant group-by-time interactions, and only one of these was not modified by site. However, both groups showed improvement over time (linear and quadratic) on most measures.
Substance use.Figure 1 shows the longitudinal patterns for scores on the SATS for the treatment groups at each site. [A table presenting data for the major outcome variables at each of the six follow-up points by treatment condition and site is available in the online version of this article at ps.psychiatryonline.org.] A different pattern of the group-by-time interaction within each site created a significant three-way interaction of group, site, and time.
For the SATS ratings, in site 1, treatment groups showed steady and similar improvement over time. In site 2, initially, the assertive community treatment group showed more rapid improvement than the standard clinical case management group. However, the standard clinical case management group in site 2 showed steady improvement throughout the three years of the study, and the two treatment groups did not differ by the end of the study.
Among clients with an alcohol use disorder at baseline (a score of 3 or higher on the AUS), groups did not differ over time with respect to researchers' average AUS ratings, although all clients improved. However, groups differed significantly over time (quadratic) with regard to log of self-reported days of drinking; the assertive community treatment group showed initial gains that eroded slightly and the standard clinical case management group showed a pattern of more steady gains. Among clients with drug use disorder at baseline (a score of 3 or higher on the DUS), a greater difference between groups over time favoring assertive community treatment at site 2 but not at site 1 produced a marginal three-way interaction for DUS ratings. Groups did not differ in self-reported days of drug use, and reported days of use declined by about one-third overall. Three years after randomization to the groups, about one-third of study participants achieved substance use remission.
Residential status. Statistically significant differences in residential status between groups emerged at site 2. Compared with the assertive community treatment group, the standard clinical case management group averaged significantly more days in the hospital (a mean of 41±60 days compared with 32±91 days for the assertive community treatment group) and significantly more days institutionalized (hospitalized or incarcerated) (158±254 days compared with 139±262 days; Mann-Whitney U=713, p=.002 and Mann Whitney U=800, p=.02, respectively, for the hospital and institutional days). At site 1 differences between the standard case management and assertive community treatment groups were not significant for either hospital days (12±28 and 15±27 days, respectively) or institutional days (68±147 and 98±172 days, respectively). [Figures illustrating these differences are available in the online version of this article at ps.psychiatryonline.org.]
Mixed regression estimates that used a three-way model (group by site by time) yielded a significant result for time (Z=2.30, p<.05), for group by time (Z=-2.27, p<.05), and for site by time (Z=3.67, p<.001), but not for group by site by time. The standard clinical case management group at both sites showed an increase in the likelihood of being institutionalized. However, the assertive community treatment group in site 2 showed a less rapid increase in the likelihood of being institutionalized, and the assertive community treatment group in site 1 showed a decline in the likelihood. When we examined days in stable housing, results were similar.
It is important to note that participants experienced approximately three times as many days incarcerated as in the hospital during the three years of follow-up. The reasons for the 331 incarcerations, in decreasing order of frequency, were violation of probation (52 incarcerations, or 16 percent), failure to appear in court (37 incarcerations, or 11 percent), possession of narcotics (26 incarcerations, or 8 percent), breach of peace (20 incarcerations, or 6 percent), larceny (19 incarcerations, or 6 percent), low-level sexual assault (17 incarcerations, or 5 percent), criminal trespass (14 incarcerations, or 4 percent), prostitution (13 incarcerations, or 4 percent), threatening behavior (12 incarcerations, or 4 percent), and interfering with or resisting an officer (12 incarcerations, or 4 percent). The remaining 109 incarcerations (33 percent) resulted from a variety of charges, most of which were crimes associated with the possession and sale of illegal substances, driving under the influence, and theft.
Other outcome domains. Treatment groups did not differ with respect to severity of psychiatric symptoms or general life satisfaction, but overall, clients experienced improvements in each of these domains. We did not observe any significant changes in global functioning over the course of the study.
Discussion
In settings in which both assertive community treatment and standard clinical case management provided integrated mental health and substance abuse treatment, clients in each treatment group showed steady and comparable reductions in substance use. A significant advantage for assertive community treatment services was seen only at the site that had relatively higher rates of institutionalization—clients in the assertive community treatment condition were less likely to be institutionalized and spent fewer days institutionalized over the course of the three-year follow up. This finding suggests that administrators in systems with low rates of institutionalization would have a greater positive impact on the lives of clients with co-occurring disorders by investing in implementing integrated treatment for individuals with co-occurring disorders rather than in assertive community treatment teams.
Four possible circumstances may have interacted to explain our findings. First, community programs have improved, and standard clinical case management has incorporated many of the values and interventions of assertive community treatment. Therefore, differences in outcomes between assertive community treatment and standard services have been attenuated in comparison with early studies (42), in which the assertive community treatment intervention was compared with standard services that were, in effect, limited to the psychiatric hospital and a traditional outpatient clinic providing office-based treatment.
Second, many clients in this study were incarcerated as a result of their involvement in illegal activity, which is consistent with the national trend and sometimes described as criminalization of persons with mental illness (69). Previous studies of assertive community treatment have not shown consistent effects on criminal justice outcomes (45), and the interventions needed to prevent institutionalization in jails and prisons may differ fundamentally from those that prevent institutionalization in hospitals. That is, community-based mental health teams may need to focus much more on developing diversion programs and collaborative relationships with the police, court systems, and judges (70).
Third, one must always question whether the intervention models under study were implemented faithfully. Both the assertive community treatment and standard clinical case management groups appeared to do a good job of delivering integrated treatment. The standard clinical case management clinicians appeared to provide high-quality, individual, clinical case management. The assertive community treatment teams showed good fidelity to the range of components of the model, with the exception of, perhaps, a lower-than-ideal rate of in-community service delivery (in part a function of the provision of in-clinic groups as part of the stagewise treatment model). It may be that increasing the delivery of services in the community (rather than in the clinic) might have reduced institutionalization further for clients who were in the assertive community treatment teams. However, the site in which the assertive community treatment team decreased institutional days was the site that had significantly fewer services in the community.
Fourth, differences between the two sites in the clinical features of clients or rates of institutional use may have affected outcomes. One site had participants with less severe alcohol use disorder and more self-reported days in stable residence in the year before baseline (Table 2). Reductions in substance use favored assertive community treatment minimally at both sites, although these differences were not statistically significant, suggesting that assertive community treatment may have a small advantage over standard clinical case management in helping clients reduce their substance use more rapidly. However, the substance use outcomes were good for all groups, and integrated treatment appeared to be effective within both treatment conditions, a finding that is similar to the New Hampshire study in which, in contrast to the present study, the sites were rural and alcohol was the primary substance of abuse (46).
An alternative explanation—that the reductions in substance use could be attributed to temporal effects rather than to treatment effects—is contradicted by several other studies. The substance use outcomes in the study reported here were comparable to the results found for an equivalently disadvantaged group of clients who received integrated treatment in Washington, D.C., and superior to the nonintegrated comparison treatment in that study (27). Furthermore, several longitudinal studies have shown assertive community treatment teams that did not provide integrated treatment did not reduce substance use among clients with severe mental illnesses (53,71,72). The recent literature continues to document that, for clients with co-occurring disorders, substance use persists in the absence of an intervention. For example, in the recent Collaborative Program to Prevent Homelessness, six programs provided mental health care and housing supports for clients with severe mental illnesses and co-occurring substance use disorders (73). Even though housing status and psychiatric symptoms improved, these studies did not find overall reductions in substance use outcomes (74).
The study reported here had significant strengths, including its randomized design, validity of substance use ratings, and high retention rate of study participants through the three-year follow-up period. The treatment interventions were faithful to their respective models and did not drift over the course of the study. One weakness was that reliability testing for interviewers was limited to training. In addition, because interviewers had to interact with clinicians, interviewers were not blind to which treatment condition group the client was in. The impact of these limitations was minimized by gaining access to outcome data from service records in management information systems—for example, hospital days and days incarcerated. This study compared the effectiveness of assertive community treatment with only one type of clinical case management. Future studies should examine the effectiveness of different types of case management interventions and how the effectiveness of these approaches may vary for clients with different characteristics—for example, type and extent of substance use, mental health diagnosis, and stage of readiness for treatment.
Four important policy implications emerge. First, for clients with both a serious mental illness and a substance use disorder, integrated treatment is critically important. Integrated treatment should be provided by whatever route it can be implemented and sustained, whether that is with an assertive community treatment team or with clinically adept, mobile, individual case managers. Both the assertive community treatment and standard clinical case management interventions can deliver successful integrated treatment. Therefore, whichever intervention can be mounted at less cost may be most preferable.
The structural model for service delivery is less important than developing and maintaining the necessary skill sets among treatment staff. These results support the findings of the Robert Wood Johnson Foundation program on chronic mental illness (75) and previous randomized trials that examined the effectiveness of assertive community treatment (46,48). These studies found that the structural organization of case management services was less important for improving substance use outcomes than the quality of the services provided. However, assertive community treatment may be the preferred model for delivering integrated treatment if standard clinical case management is delivered by clinicians in an overburdened system in which individual case managers are office-bound paraprofessionals with high caseloads. The quality of the clinical care matters, independent of the structural approach used to deliver services.
Second, assertive community treatment appears to be superior to standard clinical case management in preventing hospitalization only in settings characterized by relatively high hospital use. This was the case even though the clients assigned to the assertive community treatment teams had been recent users of hospital or crisis services.
Third, assertive community treatment and standard clinical case management may need to focus not only on the effective treatment of co-occurring disorders but also on outreach to the criminal justice system to prevent institutionalization by way of incarceration. Clients with co-occurring disorders, many of whom have previous incarcerations, are particularly vulnerable to involvement with the criminal justice system and are at high risk of multiple incarcerations. Hence, increased outreach from the mental health system to the criminal justice system may help divert individuals from incarceration. Given the modest nature of many of the charges that resulted in incarceration, this outreach may benefit not only the individual but also an overburdened criminal justice system.
Fourth, implementing and sustaining high-fidelity integrated treatment required ongoing monitoring and intervention at each of the sites in this study. For example, over a one-year period, two of the authors (KM and RD) provided more than 30 direct hours of clinical consultation and training at one of the sites, which resulted in more than 200 hours of staff training time. Over a five-year period, the mental health centers shifted from receiving clinical training and supervision from outside experts to having this expertise in house. Nevertheless, study personnel continued to monitor the interventions for fidelity throughout the study, intervening when drift seemed to be occurring (76). Systems introducing either assertive community treatment as an approach to client care or integrated treatment, whether delivered by way of assertive community treatment or standard clinical case management, should develop a means to monitor the interventions to be certain that they are occurring and, when drift appears, provide appropriately skilled clinical supervision.
Conclusions
Integrated treatment for individuals with co-occurring disorders can be successfully delivered either with assertive community treatment or standard clinical case management. Administrators in systems with low rates of institutionalization may have a greater positive effect on clients' lives by implementing integrated treatment for individuals with co-occurring disorders rather than implementing assertive community treatment teams, if neither form of treatment is already in place.
Acknowledgments
This work was supported by U.S. Public Health Services grants R01-MH-52872 and R01-MH-63463 from the National Institute of Mental Health, R01-AA-10265 from the National Institute on Alcohol Abuse and Alcoholism, and UD3-SM51560, UD3-SM51802, and UD9-MH51958 from the Substance Abuse and Mental Health Services Administration. The authors thank the following persons for facilitating the research: Carmen Abraham, M.S.W., Steve Atkins, M.D., Deb Bailey, M.S., Linda Dunakin, M.A.L.S., Lindy Fox, M.A., C.A.D.A.C., Melissa Garman, M.S.W., Barbara Helmstetter, B.A., Nannette Latremouille, M.A., Ken Marcus, M.D., Keith Miles, M.P.A., Joan Packard, B.A., Steven Pierce, Psy.D., Nydia Rios-Benitez, M.A., Eleni Rodis, M.S., Gary Savill, Ph.D., Diane Schiavo, B.A., Ed Schlager, Ph.D., Lynette Simpson, R.N., Lillian Tamayo, M.S.W., Lou Tufano, Ph.D., and Rosemarie Wolfe, M.S. The authors also acknowledge support from the psychology department and the A. J. Pappanikou Center at the University of Connecticut in Storrs. This article does not express the views of the Connecticut Department of Mental Health and Addiction Services or the State of Connecticut. The views and opinions expressed herein are those of the authors.
Dr. Essock is affiliated with the department of psychiatry at Mount Sinai School of Medicine, Box 1230, 1 Gustave L. Levy Place, New York, New York 10029-6574 (e-mail, [email protected]) and with the Mental Illness Research, Education, and Clinical Center at the Department of Veterans Affairs New York Healthcare System in Bronx, New York. Dr. Mueser, Dr. Drake, and Dr. McHugo are with the department of psychiatry at Dartmouth Medical School in Hanover, New Hampshire, and with the New Hampshire-Dartmouth Psychiatric Research Center in Lebanon, New Hampshire, with which Ms. Swain is affiliated. Dr. Covell, Dr. Frisman, Dr. Jackson, and Dr. Townsend are with the department of psychology at the University of Connecticut in Storrs and with the research division at the Connecticut Department of Mental Health and Addiction Services in Hartford, with which Dr. Kontos was affiliated at the time of the study.
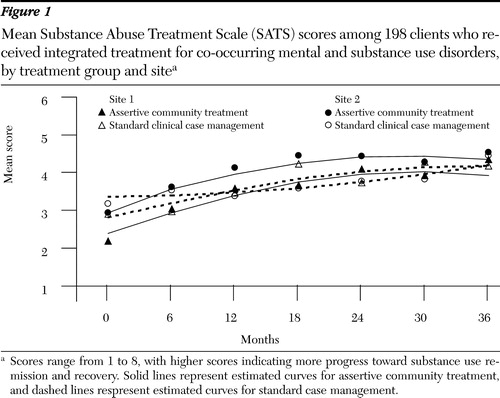
Figure 1. Mean Substance Abuse Treatment Scale (SATS) scores among 198 clients who received integrated treatment for co-occurring mental and substance use disorders, by treatment group and sitea
a Scores range from 1 to 8, with higher scores indicating more progress toward substance use remission and recovery. Solid lines represent estimated curves for assertive community treatment, and dashed lines respresent estimated curves for standard case management.
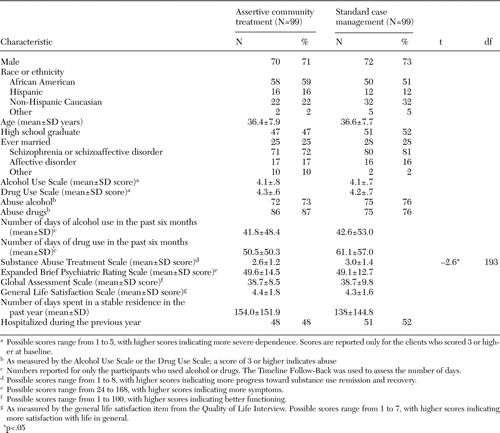 |
Table 1. Baseline characteristics of 198 clients who received integrated treatment for co-occurring mental and substance use disorders, by treatment group
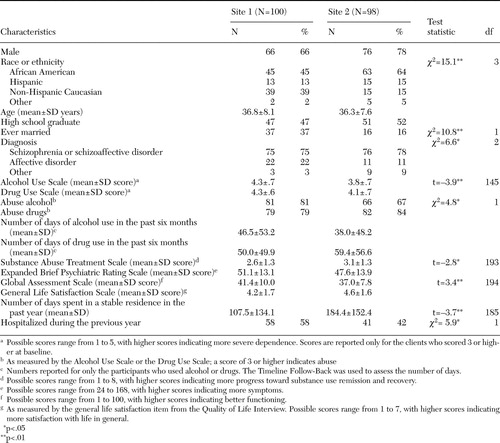 |
Table 2. Baseline characteristics of 198 clients who received integrated treatment for co-occurring mental and substance use disorders, by site
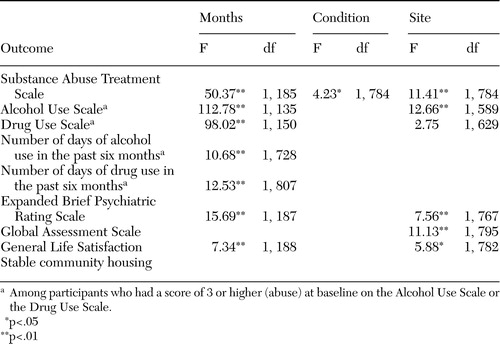 |
Table 3. Mixed-effects regression results for primary outcomes by treatment condition, site, and linear time
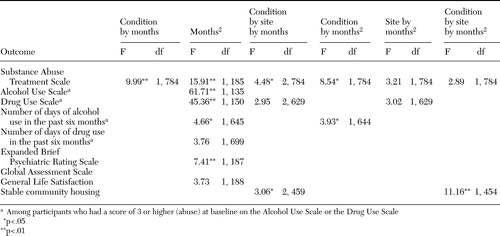 |
Table 4. Mixed-effects regression results for primary outcomes by treatment condition, site, and quadratic time (months squared) and interaction effects
1. Mueser KT, Yarnold PR, Rosenberg SD, et al: Substance use disorder in hospitalized severely mentally ill psychiatric patients: prevalence, correlates, and subgroups. Schizophrenia Bulletin 26:179–192,2000Crossref, Medline, Google Scholar
2. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. JAMA 264:2511–2518,1990Crossref, Medline, Google Scholar
3. Rosenberg SD, Drake RE, Wolford GL, et al: The Dartmouth Assessment of Lifestyle Instrument (DALI): a substance use disorder screen for people with severe mental illness. American Journal of Psychiatry 155:232–238,1998Abstract, Google Scholar
4. Dickey B, Azeni H: Persons with dual diagnoses of substance abuse and major mental illness. American Journal of Public Health 86:973–977,1996Crossref, Medline, Google Scholar
5. Drake RE, Brunette MF: Complications of severe mental illness related to alcohol and other drug use disorders, in Recent Developments in Alcoholism: Consequences of Alcoholism: Vol 14. Edited by Galanter M. New York, Plenum, 1998Google Scholar
6. Rosenberg SD, Goodman LA, Osher FC, et al: Prevalence of HIV, hepatitis B, and hepatitis C in people with severe mental illness. American Journal of Public Health 91:31–37,2001Crossref, Medline, Google Scholar
7. Swartz MS, Swanson JW, Hiday VA, et al: Taking the wrong drugs: the role of substance abuse and medication noncompliance in violence among severely mentally ill individuals. Social Psychiatry and Psychiatric Epidemiology 33:S75-S80, 1998Google Scholar
8. El-Guebaly N: Substance abuse and mental disorders: the dual diagnoses concept. Canadian Journal of Psychiatry 35:261–267,1990Crossref, Medline, Google Scholar
9. Polcin DL: Issues in the treatment of dual diagnosis clients who have chronic mental illness. Professional Psychology: Research and Practice 23:30–37,1992Crossref, Google Scholar
10. Ridgely MS, Osher FC, Goldman HH, et al: Chronic Mentally Ill Young Adults With Substance Abuse Problems: A Review of Research, Treatment, and Training Issues: Executive Summary. Baltimore, University of Maryland School of Medicine, 1987Google Scholar
11. Ridgely MS, Goldman HH, Willenbring M: Barriers to the care of persons with dual diagnoses: organizational and financing issues. Schizophrenia Bulletin 16:123–132,1990Crossref, Medline, Google Scholar
12. Carey KB: Substance use reduction in the context of outpatient psychiatric treatment: a collaborative, motivational, harm reduction approach. Community Mental Health Journal 32:111–134,1996Crossref, Google Scholar
13. Minkoff K: An integrated treatment model for dual diagnosis of psychosis and addiction. Hospital and Community Psychiatry 40:1031–1036,1989Abstract, Google Scholar
14. Mueser KT, Noordsy DL, Drake RE, et al: Integrated Treatment for Dual Disorders: A Guide to Effective Practice. New York, Guilford, 2003Google Scholar
15. Ziedonis D, Fisher W: Assessment and treatment of comorbid substance abuse in individuals with schizophrenia. Psychiatric Annals 24:477–483,1994Crossref, Google Scholar
16. Drake RE, Bartels SJ, Teague GB, et al: Treatment of substance abuse in severely mentally ill patients. Journal of Nervous and Mental Disease 181:606–611,1993Crossref, Medline, Google Scholar
17. Miller WR, Rollnick S (eds): Motivational Interviewing: Preparing People for Change, 2nd ed. New York, Guilford, 2002Google Scholar
18. Drake RE, Mueser KT, McHugo GJ, et al: Review of treatments for persons with severe mental illnesses and co-occurring substance use disorders. Psychiatric Rehabilitation Journal 27:360–374,2004Crossref, Medline, Google Scholar
19. Carmichael D, Tackett-Gibson M, O'Dell L, et al: Texas Dual Diagnosis Project Evaluation Report 1997-1998. College Station, Tex, Texas A&M University, Public Policy Research Institute, 1998Google Scholar
20. Godley SH, Hoewing-Roberson R, Godley MD: Final MISA Report. Bloomington, Ill, Lighthouse Institute, 1994Google Scholar
21. Graeber DA, Moyers TB, Griffith G, et al: A pilot study comparing motivational interviewing and an educational intervention in patients with schizophrenia and alcohol use disorders. Community Mental Health Journal 39:189–202,2003Crossref, Medline, Google Scholar
22. James W, Preston NJ, Koh G, et al: A group intervention which assists patients with dual diagnosis reduce their drug use: a randomized controlled trial. Psychological Medicine 34:983–990,2004Crossref, Medline, Google Scholar
23. Kavanagh DJ, Young R, White A, et al: A brief motivational intervention for substance misuse in recent-onset psychosis. Drug and Alcohol Review 23:151–155,2004Crossref, Medline, Google Scholar
24. Barrowclough C, Haddock G, Tarrier N, et al: Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. American Journal of Psychiatry 158:1706–1713,2001Link, Google Scholar
25. Haddock G, Barrowclough C, Tarrier N, et al: Cognitive-behavioural therapy and motivational intervention for schizophrenia and substance misuse:18–month outcomes of a randomized controlled trial. British Journal of Psychiatry 183:418-426,2003Google Scholar
26. Hellerstein DJ, Rosenthal RN, Miner CR: A prospective study of integrated outpatient treatment for substance-abusing schizophrenic outpatients. American Journal on Addictions 4:33–42,1995Crossref, Google Scholar
27. Drake RE, Yovetich N, Bebout RR, et al: Integrated treatment for homeless, dually diagnosed adults. Journal of Nervous and Mental Disease 185:298–305,1997Crossref, Medline, Google Scholar
28. Ho AP, Tsuang JW, Liberman RP, et al: Achieving effective treatment of patients with chronic psychotic illness and comorbid substance dependence. American Journal of Psychiatry 156:1765–1770,1999Abstract, Google Scholar
29. Jerrell JM, Ridgely MS: Comparative effectiveness of three approaches to serving people with severe mental illness and substance use disorders. Journal of Nervous and Mental Disease 183:566–576,1995Crossref, Medline, Google Scholar
30. Burnam MA, Morton SC, McGlynn EA, et al: An experimental evaluation of residential and nonresidential treatment for dually diagnosed homeless adults. Journal of Addictive Diseases 14:111–134,1995Crossref, Medline, Google Scholar
31. Penn PE, Brooks AJ: Comparing Substance Abuse Treatments for Dual Diagnosis: Final Report. Tucson, Ariz, La Frontera Center, 1999Google Scholar
32. Ley AJ: Cochrane review of treatment outcome studies and its implications for future developments, in Substance Misuse in Psychosis: Approaches to Treatment and Service Delivery. Edited by Graham HL, Copello A, Birchwood MJ, et al. Chichester, England, John Wiley, 2003Google Scholar
33. Drake RE, Essock SM, Shaner A, et al: Implementing dual diagnosis services for clients with severe mental illness. Psychiatric Services 52:469–476,2001Link, Google Scholar
34. Report to Congress on the Prevention and Treatment of Co-occurring Substance Abuse and Disorders and Mental Disorders. Rockville, Md, US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, 2002Google Scholar
35. Onken LS, Blaine JD, Genser S, et al: Treatment of Drug-Dependent Individuals With Comorbid Mental Disorders. NIDA research monograph 172. Bethesda, Md, National Institute of Drug Abuse, 1997Google Scholar
36. President's New Freedom Commission on Mental Health: Achieving the Promise: Transforming Mental Health Care in America. Washington, DC, Department of Health and Human Services, 2003Google Scholar
37. Mental Health: A Report of the Surgeon General. Washington, DC, Department of Health and Human Services, US Public Health Services, 1999Google Scholar
38. Brunette MF, Mueser KE, Drake RE: A review of research on residential programs for people with severe mental illness and co-occurring substance use disorders. Drug and Alcohol Review 23:471–481,2004Crossref, Medline, Google Scholar
39. Mueser K, Drake R, Sigmon S, et al: Psychosocial interventions for adults with severe mental illnesses and co-occurring substance use disorders: a review of specific interventions. Journal of Dual Diagnosis 1:57–82,2005Crossref, Google Scholar
40. Allness DJ, Knoedler WH: The PACT Model of Community-Based Treatment for Persons With Severe and Persistent Mental Illness: A Manual for PACT Start-Up. Arlington, Va, National Alliance for the Mentally Ill, 1998Google Scholar
41. Stein LI, Santos AB: Assertive Community Treatment of Persons with Severe Mental Illness. New York, Norton, 1998Google Scholar
42. Stein LI, Test MA: Alternative to mental hospital treatment: I. Conceptual model, treatment program, and clinical evaluation. Archives of General Psychiatry 37:392–397,1980Crossref, Medline, Google Scholar
43. Bond GR, Drake RE, Mueser KT, et al: Assertive community treatment for people with severe mental illness: critical ingredients and impact on clients. Disease Management and Health Outcomes 9:141–159,2001Crossref, Google Scholar
44. Mueser KT, Drake RE, Noordsy DL: Integrated mental health and substance abuse treatment for severe psychiatric disorders. Practical Psychiatry and Behavioral Health 4:129–139,1998Crossref, Google Scholar
45. Mueser KT, Bond GR, Drake RE, et al: Models of community care for severe mental illness: a review of research on case management. Schizophrenia Bulletin 24:37–74,1998Crossref, Medline, Google Scholar
46. Drake RE, McHugo GJ, Clark RE, et al: Assertive community treatment for patients with co-occurring severe mental illness and substance use disorder: a clinical trial. American Journal of Orthopsychiatry 68:201–215,1998Crossref, Medline, Google Scholar
47. Burns BJ: Links between research findings and the future of assertive community treatment: a commentary. American Journal of Orthopsychiatry 68:261–264,1998Crossref, Medline, Google Scholar
48. Essock SM, Frisman LK, Kontos NJ: Cost-effectiveness of assertive community treatment teams. American Journal of Orthopsychiatry 68:179–190,1998Crossref, Medline, Google Scholar
49. Swofford CD, Kasckow JW, Scheller-Gilkey G, et al: Substance abuse: a powerful predictor of relapse in schizophrenia. Schizophrenia Research 20:145–151,1996Crossref, Medline, Google Scholar
50. Bartels SJ, Teague GB, Drake RE, et al: Substance abuse in schizophrenia: service utilization and costs. Journal of Nervous and Mental Disease 181:227–232,1993Crossref, Medline, Google Scholar
51. Latimer E: Economic impacts of assertive community treatment: a review of the literature. Canadian Journal of Psychiatry, 44:443–454,1999Crossref, Medline, Google Scholar
52. Test MA, Stein LI: Practical guidelines for the community treatment of markedly impaired patients. Community Mental Health Journal 12:72–82,1976Crossref, Medline, Google Scholar
53. McHugo GJ, Drake RE, Teague GB, et al: The relationship between model fidelity and client outcomes in the New Hampshire Dual Disorders Study. Psychiatric Services 50:818–824,1999Link, Google Scholar
54. Mueser KT, Essock SM, Drake RE, et al: Rural and urban differences in patients with a dual diagnosis. Schizophrenia Research 48:93–107,2001Crossref, Medline, Google Scholar
55. Teague GB, Drake RE, Ackerson TH: Evaluating use of continuous treatment teams for persons with mental illness and substance abuse. Psychiatric Services 46:689–695,1995Link, Google Scholar
56. Spitzer RL, Williams JBW, Gibbon M, et al: Structured Clinical Interview for DSM-III-R-Patient Version (SCID-P). New York, New York State Psychiatric Institute, Biometric Research Department, 1988Google Scholar
57. Tessler RC, Goldman HH: The chronically mentally ill: assessing community support programs. Cambridge, Mass, Ballinger, 1982Google Scholar
58. Sobell MB, Maisto SA, Sobell LC, et al: Developing a prototype for evaluating alcohol treatment effectiveness, in Evaluating Alcohol and Drug Abuse Treatment Effectiveness. Edited by Sobell LC, Sobell MB, Ward E. New York, Pergamon, 1980Google Scholar
59. McLellan AT, Luborsky L, O'Brien CP, et al: An improved evaluation instrument for substance abuse patients: the Addiction Severity Index. Journal of Nervous and Mental Disease 168:826–833,1980Crossref, Google Scholar
60. Clark RE, Ricketts SK, McHugo GJ: Measuring hospital use without claims: a comparison of patient and provider reports. Health Services Research 31:153–169,1996Medline, Google Scholar
61. Lehman AF: A quality of life interview for the chronically mentally ill. Evaluation and Program Planning 11:51–62,1988Crossref, Google Scholar
62. Lukoff D, Nuechterlein KH, Ventura J: Manual for expanded Brief Psychiatric Rating Scale (BPRS). Schizophrenia Bulletin 12:594–602,1986Google Scholar
63. Drake RE, Osher FC, Noordsy DL, et al: Diagnosis of alcohol use disorders in schizophrenia. Schizophrenia Bulletin 16:57–67,1990Crossref, Medline, Google Scholar
64. McHugo GJ, Drake RE, Burton HL, et al: A scale for assessing the stage of substance abuse treatment in persons with severe mental illness. Journal of Nervous and Mental Disease 183:762–767,1995Crossref, Medline, Google Scholar
65. Drake RE, Mueser KT, McHugo GJ: Using clinician rating scales to assess substance use among persons with severe mental illness, in Outcomes Assessment in Clinical Practice. Edited by Sederer LI, Dickey B. Baltimore, Williams and Wilkins, 1995Google Scholar
66. Jennrich RI, Schluchter MD: Unbalanced repeated-measures models with structured covariance matrices. Biometrics 42:805–820,1986Crossref, Medline, Google Scholar
67. McLean RA, Sanders WL, Stroup WW: A unified approach to mixed linear models. American Statistician 45:54–64,1991Google Scholar
68. Gibbons RD, Hedeker G, Elkin I, et al: Some conceptual and statistical issues in analysis of longitudinal psychiatric data. Archives of General Psychiatry 50:739–750,1993Crossref, Medline, Google Scholar
69. Abram KM, Teplin LA: Co-occurring disorders among mentally ill jail detainees: implications for public policy. American Psychologist 46:1036–1045,1991Crossref, Medline, Google Scholar
70. Fisher WH (ed): Community Based Interventions for Criminal Offenders With Severe Mental Illness. Greenwich, Conn, Jai Press, 2003Google Scholar
71. Bond GR, McDonel EC, Miller LD, et al: Assertive community treatment and reference groups: an evaluation of their effectiveness for young adults with serious mental illness and substance abuse problems. Psychosocial Rehabilitation Journal 15(2):31–43,1991Google Scholar
72. Morse GA, Calsyn RJ, Allen G, et al: Experimental comparison of the effects of three treatment programs for homeless mentally ill people. Hospital and Community Psychiatry 43:1005–1010,1992Abstract, Google Scholar
73. Rickards LD, Leginshi W, Randolph FL, et al: Cooperative agreements for CMHS/CSAT collaborative program to prevent homelessness: an overview. Alcoholism Treatment Quarterly 17:1–15,1999Crossref, Google Scholar
74. Sacks JY, Drake RE, Williams V, et al: Utility of the Time-Line Follow-Back to assess substance use among homeless adults. Journal of Nervous and Mental Disease 191:145–153,2003Medline, Google Scholar
75. Goldman HH, Morrissey JP, and Ridgely MS: Evaluating the Robert Wood Johnson Foundation Program on Chronic Mental Illness. Milbank Quarterly, 72:37–47,1994Crossref, Medline, Google Scholar
76. Torrey WC, Drake RE, Dixon L, et al: Implementing evidence-based practices for persons with severe mental illnesses. Psychiatric Services 52:45–60,2001Link, Google Scholar



