Special Section on Seclusion and Restraint: Pennsylvania State Hospital System's Seclusion and Restraint Reduction Program
Abstract
OBJECTIVES: This study examined the use of seclusion and mechanical restraint from 1990 to 2000 and the rate of staff injuries from patient assaults from 1998 to 2000 in a state hospital system. METHODS: Records of patients older than 18 years who were civilly committed to one of the nine state hospitals in Pennsylvania were included in the analyses. Two databases were used in each of the nine hospitals: one identified date, time, duration, and justification for each episode of seclusion or restraint and the other identified when a patient was hospitalized and the demographic characteristics and the diagnosis of the patient. Rate and duration of seclusion and restraint were calculated. Reports from compensation claims were used to determine staff injuries from patient assaults. RESULTS: The rate and duration of seclusion and mechanical restraint decreased dramatically during this period. From 1990 to 2000, the rate of seclusion decreased from 4.2 to .3 episodes per 1,000 patient-days. The average duration of seclusion decreased from 10.8 to 1.3 hours. The rate of restraint decreased from 3.5 to 1.2 episodes per 1,000 patient-days. The average duration of restraint decreased from 11.9 to 1.9 hours. Patients from racial or ethnic minority groups had a higher rate and longer duration of seclusion than whites. Seclusion tended to be less likely, but longer, during the night shift. Patients were restrained less often during the night shift, but for a longer duration. The rate of restraint was higher during the week than during weekends and holidays. Younger patients were more likely to be secluded and restrained, but older patients remained secluded and restrained longer. No significant changes were seen in rates of staff injuries from 1998 to 2000. CONCLUSIONS: Many factors contributed to the success of this effort, including advocacy efforts, state policy change, improved patient-staff ratios, response teams, and second-generation antipsychotics.
The use of seclusion and restraint in psychiatric hospitals to control people with disturbed or violent behaviors has been occurring for centuries. The literature is replete with examples of how clinicians have struggled with the ethical issues involved with the use of these interventions (1,2,3,4). The literature has also provided the rationale for the continued use of physical controls in modern psychiatric settings, much like it did in the past for asylums (4,5,6). More recent research has questioned the need to use these practices and pointed to studies showing inconsistency in the application of seclusion and restraint (6,7). An international review of these procedures found the same inconsistencies in the use of seclusion and restraint with psychiatric patients and the same struggles with the ethics of these practices (8). Seclusion and restraint has prevailed internationally as the primary approach to managing violent behaviors, although the degree of use depends on the country or geographical location (9,10,11,12).
Since 1990 the Pennsylvania state hospital system has experienced constant changes that have resulted in remarkable outcomes in reducing the use of seclusion and restraint. The Pennsylvania state hospital system, one of the oldest in the country, serves adults within a civil and forensic inpatient setting who have severe and persistent mental illnesses. During most of its history the hospital system provided direct admission services. However, during the study period, the admission of civilly committed patients was limited to referrals from local psychiatric acute care settings for individuals who were unable to be stabilized within a 30-day acute care stay.
The purpose of this study was to systematically report changes in patterns of seclusion and mechanical restraint over an 11-year period (1990 to 2000) that took place within Pennsylvania's nine state hospitals. Because so many changes were implemented during this period it was not possible to isolate and analyze the effects of a single variable. Changes that influenced the reduction of seclusion and restraint are discussed.
Methods
The data used for this study were taken from two sources maintained by each of the nine hospitals. The first database identified date, time of day, duration, and justification for each event of seclusion or restraint. The second database identified when a patient was present in the hospital and supplied basic demographic and diagnostic information. All data were merged and reformatted by using an anonymous patient identifier for analysis. Only adults 18 years and older who were served on civil units of the hospitals were included in this study. In addition, only the use of seclusion and mechanical restraint was evaluated.
An individual annual rate was calculated as the total number of events divided by the total number of days in the hospital that year multiplied by 1,000 (referred to as rate per 1000 patient-days). If a patient was not restrained during that year's stay in the hospital, they were assigned a rate of zero. For the year-specific average rate, the individual rates were averaged across all patients in the hospital that year. Duration was defined as hours per event. An individual annual duration was calculated if the patient had one or more events that year. For the year-specific average duration time, the individual means were averaged across patients who had at least one event during that year.
The Jonckheere-Terpstra test (13) was used to compare the ordinal differences of the seclusion and restraint rates over time or among different classes. The generalized estimating equations (GEE) method (14) was employed to perform various hypothesis tests, including testing whether the overall duration or rate of one factor depends on the level of the other factor. The GEE method is a useful extension of the generalized linear models for continuous and categorical data that does not require the exact knowledge of variance-covariance structure of the repeated outcomes. The GEE is favored over multivariate analysis of variance (MANOVA) because our study consists of double repeated measurements from hospitals and patients nested under hospitals over the 11-year period. Estimation of the covariance structure using MANOVA proves to be problematic sometimes.
For the purpose of analysis, the sample was divided into four age groups: 25 years and younger, 26 to 40 years, 41 to 65 years, and 66 years and older. Race and ethnicity were considered in terms of whites and all racial and ethnic minority groups. The events were categorized in terms of hospital work shift (day shift, 7 a.m. to 3 p.m.; evening shift, 3 p.m. to 11 p.m.; and night shift, 11 p.m. to 7 a.m.) and by weekday compared with weekend or holiday. The Jonckheere Terpstra test was used to evaluate data derived from the annual census data from the hospital system. All other analyses were evaluated by using the GEE method (14).
Data on staff injuries from patient assaults were available only for 1998 to 2000. We examined the number of events in which employees lost time from work as a result of injuries from assaults and events in which first aid only was needed as a result of an assault. Each hospital's compensation claims were used for this analysis. The counts were not duplicated within these measures. To determine the rate of change each year, these events were calculated per 1,000 patient-days of care.
Results
The annual census for the hospital system during this 11-year period decreased 56 percent, from about 6,300 to about 2,800. During this time the gender ratio remained constant (53 percent men and 47 percent women), and representation of racial or ethnic minority groups increased slightly (p=.03). This change was consistent with changes in the size of the population of racial or ethnic minority groups in Pennsylvania.
As shown in Table 1, the rate of seclusion decreased from a high of 7.2 episodes per 1,000 patient-days in 1991 to .3 episodes per 1,000 patient-days in 2000. The average rate of seclusion was similar for men and women, and this rate significantly decreased during the study period (p<.01). The rate of seclusion was greater for persons in racial or ethnic minority groups than for whites (4.3 episodes per 1,000 patient-days compared with 2.5 episodes per 1,000 patient-days, p<.01). Over the study period, the rate of seclusion decreased to a greater degree among persons from racial or ethnic minority groups (p<.05). The rate of seclusion was inversely associated with age—that is, the youngest group had the highest rate (6.0 episodes per 1,000 patient-days for the youngest age group compared with .3 episodes per 1,000 patient-days for the oldest age group, p<.01). The rate of seclusion was lowest during the night shift (1.4, 1.5, and .4 episodes per 1,000 patient-days, for the day, evening, and night shifts, respectively, p<.01) and higher during the week than during weekends and holidays (2.5 episodes per 1,000 patient-days compared with .6 episodes per 1,000 patient-days, p<.01).
The average duration of seclusion decreased from a high of 11.6 hours in 1991 to 1.3 hours in 2000 (Table 1). The duration of seclusion was longer for men than for women (8.7 hours compared with 7.4 hours, p<.01) and was shorter for whites than for persons from a racial or ethnic minority group (7.6 hours compared with 9.8 hours, p<.01). Older patients were secluded longer than younger patients (8.7 hours for the oldest age group compared with 5.0 hours for youngest age group, p<.01). The duration for seclusion tended to be longer during the night shift (8.0, 8.4, and 10.7 hours, for the day, evening and night shifts, respectively, p<.01) and shorter during the week than during weekends or holidays (8.0 hours compared with 9.5 hours, p<.01).
The rate of mechanical restraint decreased from a high of 6.4 episodes per 1,000 patient-days in 1991 to 1.2 episodes per 1,000 patient-days in 2000 (Table 1). The rate of restraint was about the same for women and men and for whites and persons from a racial or ethnic minority group. The rate of mechanical restraint was inversely associated with age. The youngest group had the highest rate (8.2 episodes per 1,000 patient-days compared with 1.2 episodes per 1,000 patient-days for the oldest age group, p<.01). The rate of mechanical restraint tended to be lowest during the night shift (1.8, 1.5, and .5 episodes per 1,000 patient-days, for the day, evening, and night shifts, respectively, p<.01). The rate was higher during the week than during weekends and holidays (2.7 episodes per 1,000 patient-days compared with .7 episodes per 1,000 patient-days, p<.01).
The average duration of mechanical restraint decreased from a high of 12.1 hours in 1992 to 1.9 hours in 2000 (Table 1). The duration of mechanical restraint remained similar for women and men and for whites and persons from a racial or ethnic minority group. Older patients tended to be in mechanical restraint longer than younger patients (11.4 hours for the oldest age group compared with 5.0 hours for youngest age group, p<.01). Patients tended to be in mechanical restraint for longer periods during the night shift (8.0, 8.0, and 15.4 hours for the day, evening, and night shifts, respectively, p<.01). The duration was about the same during the week and during weekends or holidays (8.5 hours during the week compared with 8.9 hours during weekends or holidays).
Data on staff injuries from patient assaults were available only from 1998 to 2000. Even though major reductions in the use of seclusion and restraint had already occurred, it is valuable to consider this measure, because it is common for health care workers to be concerned about staff injury when the use of these procedures is reduced. The rate of staff injuries did not change during this period. In 1998 the overall rate of staff injuries involving lost work time from a patient assault was .1 episodes per 1,000 patient-days and in 2000 the rate was .13 episodes per 1,000 patient-days. The overall rate of staff injuries from assault involving first aid only was .21 episodes per 1,000 patient-days in 1998 and .23 episodes per 1,000 patient-days in 2000.
Changes that influenced reduction in seclusion and restraint
Leadership. The nonrestraint movement within the Pennsylvania state hospital system predates the period covered by this study. Most of the dramatic reductions occurred from 1993 to 1997 and are credited to direct care staff at local hospitals (aides, nurses, doctors, and program staff) and community advocates (for example, parents and representatives of the National Alliance for the Mentally Ill and Pennsylvania Protection and Advocacy, Inc.). When these groups applied their values through individual and group leadership, they were successful in changing the culture of restraint that existed within the hospital system in the early 1990s. Staff arguments at the unit level for and against the use of restraint, sometimes during the crisis itself, were common. It was common for advocates to complain to hospital and state officials about the unnecessary use of restraint or seclusion. Staff and advocates worked with the system internally and externally to change the culture of restraint in hospitals.
During the study period, five different individuals served as the deputy secretary for the State Office of Mental Health and Substance Abuse Services (OMHSAS), and three different individuals served as chief psychiatrist for OMHSAS. All of them played a role in reducing seclusion and restraint. However, it was Charles Curie, OMHSAS deputy secretary from 1996 to 2001, who challenged the status quo by establishing new standards that further limited the use of these restrictive procedures. In 1997 he announced that the use of seclusion and restraint represented "treatment failure" and challenged the system to eliminate their use and find more positive ways of supporting a person in crisis. According to Curie, consumers and their families, as well as the Pennsylvania advocacy community, provided support for this important change. He added that the use of restraint and seclusion conflicted with the recovery approach (15) that was being implemented statewide (personal communication, Curie C, 2003).
The importance of this announcement cannot be overstated. At the time, the debate over the nonrestraint approach was growing. Some clinicians argued that it was a psychiatric decision if and when to use seclusion or mechanical restraint. They felt that seclusion and restraint were important tools that were required to manage a crisis and that without them the hospital environment would become more violent and unsafe. Curie's "treatment failure" announcement did not ban the use of seclusion or restraint. However, the announcement served as a challenge to the system to find more positive ways of supporting a person in crisis. The announcement put to rest arguments occurring at the hospital level between clinicians and administrators on the restraint issue and established direction for further systemwide changes.
Curie attributed the continued decrease in the use of seclusion and restraint to improved data collection and greater transparency in the way information is shared and used to compare restraint rates between the hospitals. He also credited statewide performance improvement projects that focused on ways to reduce the use of these restrictive procedures. This effort led to greater emphasis on staff training in the areas of crisis management and nonoffensive skill development that reinforced verbal deescalation techniques.
Finally, during the study period there were several facility closures across the state. These closures increased the number of new staff who entered the hospital system. These closures affected every hospital and typically involved staff from the state mental retardation centers who challenged the long-standing treatment concepts of the hospital system. This group of workers, using behavioral support principles, helped decrease dependence on the use of restrictive procedures. Their contributions to this change, at all levels of the hospital system, were invaluable.
Advocacy efforts. Organized advocacy efforts to reduce the use of seclusion and restraint in the state hospital system started long before the study period. Often led by parents and former patients who represented local and state chapters of the National Alliance for the Mentally Ill, the Pennsylvania Mental Health Consumers Association, Pennsylvania Protection and Advocacy, Inc., and others, these efforts were instrumental in challenging the system's dependence on these restrictive procedures (personal communication Banks J, Madigan P, 2003).
These groups were particularly active in the southeast region of the commonwealth, where they regularly engaged the leadership of Allentown, Haverford, Norristown, and Philadelphia state hospitals with complaints involving the misuse and overuse of seclusion and restraint (personal communication, Rehrman M, 2003). Additionally, by 1995 state government had independent advocates assigned to each hospital. These facility-level advocates provided a needed layer of protection for the patient on a day-to-day basis (personal communication, Zuber B, 2003).
At the state level there were constant questions by these groups about the hospital system's use of seclusion and restraint. Demands were made for regular reports on the use of these procedures that led to improved data collection. They also pushed for more effective staff training that would make the use of seclusion or restraint an intervention of last resort.
Although these groups never joined together to pressure the state government to decrease the use of these procedures, they were effective at addressing individual patient issues and challenging the leadership of OMHSAS to monitor and reduce the use of seclusion and restraint. Deputy Secretary Curie's announcement in 1997 that the use of seclusion and restraint constituted treatment failure was a credit to their individual efforts.
State policy change. State policy on the use of restrictive procedures in the state hospitals changed three times during the study period. After Curie's "treatment failure" announcement the policy was revised to further limit the circumstances in which restrictive procedures could be used. This change defined physical restraint, mechanical restraint, protective restraint, and seclusion as extreme measures and limited their use to emergency situations. It also defined chemical restraint as the use of medication for the specific purpose of controlling aggressive behavior, which restricts a person's freedom of movement by rendering him or her in a semistupor or unable to attend to personal needs, and the policy prohibited its use.
The policy also established guidelines for annual staff training sessions. The policy change included procedures for patient and staff debriefing sessions after the use of restraint or seclusion. It also required, with consent, the notification of a person's family after the use of a restrictive procedure. New physician protocols were also part of this change, which limited orders for restraint and seclusion to no more than 60 minutes and required that the person be seen within 30 minutes of a phone order. Each hospital's performance improvement programs were required to monitor the ongoing use of these procedures (16). Finally, the policy change limited to eight the number of approved restraint devices that could be used: one-, two-, three-, and four-point soft Velcro restraint devices; soft mitts; and two-, three-, and four-point leather restraint devices.
Psychiatric emergency response teams (PERTs). The concept of presenting a large show of staff support at the scene of a psychiatric crisis to ensure safety has been around for more than 200 years. In 1794 Philippe Pinel, a French psychiatrist, was one of earliest to write about the effectiveness of teamwork as a procedure in managing a psychiatric emergency (1,4).
PERTs bring together a large group of workers at the scene of the crisis in a short period. The goal of PERTs is to manage a crisis by using conflict resolution, mediation, therapeutic communication, and violence-prevention skills to diffuse and safely resolve a crisis.
This approach was first implemented by Allentown State Hospital in 1993 during its peak year of seclusion and restraint use. PERTs are credited for eliminating the use of seclusion and dramatically decreasing the use of restraint in Allentown. This method evolved out of a similar program that was used at the Department of Veterans Affairs Medical Center in Coatesville, Pennsylvania, but includes many enhancements.
PERTs involve a core group of about 40 volunteer nursing and program services staff who work during the day and evening shifts. Teams of seven, led by a captain, serve on-call PERT duty about twice a week. If insufficient volunteers are available, nursing staff are assigned to the team on a rotating basis.
When a crisis occurs the staff member at the scene announces a "code orange" and the location of the emergency over the pager system. When PERT members receive the page, they stop what they are doing and report to the area. As team members arrive they are met by the PERT captain, who determines which approach to take with the person in crisis on the basis of personal observation and treatment team input. Unless the person presents an immediate danger to self or others, the initial PERT response focuses on clearing the area. Next, the PERT members, under the direction of the captain, attempt to engage the person in a therapeutic conversation directed at identifying the underlying reasons for the crisis. The focus of this meeting is to help the individual understand what needs to occur for him or her to regain control (17). Once the crisis has been resolved, a debriefing session is held with staff to critique the response and review the outcome. A separate debriefing session is conducted with the patient when he or she is calm. The Allentown model also involves a PERT assist process that is used in anticipation of a possible crisis with people who have a history of aggression.
Data on the effectiveness of PERT in Allentown were available from 1998 to 2000. During this time PERT has successfully managed 70 percent of its crises without resorting to the use of a restrictive procedure.
During the study period, all hospitals were required to upgrade the quality and quantity of their training on crisis management and verbal deescalation techniques, making it an annual requirement for all clinical, nursing, and program staff (16).
Unit size and patient-to-staff ratios. The average number of people served on a typical hospital unit during the study period decreased from more than 36 in 1990 to 32 or less in 2000. In 1990 the typical hospital unit for 36 civilly committed individuals was staffed with one licensed nurse and three psychiatric aides during the day and evening shifts. During 2000, the average staffing for a 32-bed unit increased to two licensed nurses and four psychiatric aides during the day and evening shifts.
The smaller units were made possible through the state-funded Community Hospital Integration Project Program (CHIPP) that supports the discharge of people with two or more years of inpatient hospital care. During the study period, more than 1,600 people were discharged through this program. CHIPP is credited with expanding the capacity of local communities to support people with severe mental illnesses while decreasing dependence on state hospital services (18).
Pennsylvania's experience since 1990 reinforces the belief that having fewer patients on a unit allows more sensitive care and a safer, restraint-free hospital.
Incident management system. Before 1998 the state hospital system used a basic network database that recorded the application of any restrictive procedures used for a patient in the hospital system. The reporting and tracking system required a cause for each use of a restrictive procedure (19). Most of the aggregate data used in this study were taken from this system. However, the complexities of this database made it difficult for hospitals to use. These difficulties meant that staff at the unit level saw little of the comparative information or the history of individual patients that this system contained.
In July 1998 a new application was implemented statewide that increased the number of performance indicators on which the hospitals would report. The application was designed to enable staff at the unit level to request reports on any of the 35 performance indicators. Enhanced at least twice since its original design, the system now enables measurement of physical hands-on restraint to the second and mechanical restraint use by type of device type. It also tracks the psychiatric use of PRN (as needed) and STAT (immediate) medications administered as a result of a reportable incident. These data are summarized each month and shared with the hospital system and external advocates. The report provides comparative tables, by type of care, on the use of restrictive measures. This application also provides the state hospital system's national benchmarking data (20).
Second-generation antipsychotics. Another significant change that occurred during this period was the introduction of second-generation antipsychotics. A central state formulary for all hospitals was developed in 1993 in conjunction with the creation of a joint pharmacy, therapeutics, and formulary committee. To this day the committee maintains the formulary and develops drug usage policies and procedures (21). All second-generation antipsychotics were added to the formulary as soon as they were released. Additionally, there were no restrictions on their use. As of December 31, 2000, among people who had been given a diagnosis of schizophrenia in the state hospitals, 85 percent were given a prescription for second-generation antipsychotics.
The impact of second-generation antipsychotics on the use of seclusion and restraint in the state hospital system cannot be isolated from the other changes that occurred during this period (22). Second-generation antipsychotics have been shown to reduce aggression and hostility as well as seclusion and restraint (23,24,25). Studies from Mayview State Hospital in Pennsylvania suggest that clozapine and risperidone reduced the use of these procedures (26,27). However, the authors of these studies acknowledged that among the weaknesses of their research was the failure to control for the many other changes that occurred during this period.
Increase in the quantity and quality of treatment. Another significant change in the hospital culture during the study period was an increase in the quantity and quality of active patient treatment. This change was implemented in 1995 and involved greater emphasis on functional programming—such as vocational services, paid work, money management skills, and training in the self-administration of medication—that would be needed to prepare a person for discharge. The increase in the quantity and quality of therapies was made possible by the reduced unit size and improved patient-to-staff ratios.
By 1997 there was a shift from the practice of providing therapy for the "cooperative few" to providing therapy for all patients by using small and large group approaches to programming. Program centers were established to move therapy away from the unit whenever possible. Much of this change was driven by the need to provide patients with more functional programs and activities that reinforced the skills that they would need for their recovery (personal communication, Storm R, 2003).
The impact of this change on reducing the hospital's use of seclusion and restraint has been difficult to measure. However, anecdotal evidence reinforces the belief that "the more you do with your patients, the less you have to do to them" (personal communication, O'Dea RM, 1995).
Discussion
The Pennsylvania movement toward a nonrestraint approach to the care and treatment of people with severe mental illnesses predates the period covered by this study. The dramatic decreases in the use of these restrictive procedures by state hospital systems were the result of many changes. It did not occur through litigation or a sentinel event. Nor did it happen at the same rate for each hospital. The nine hospitals used similar approaches, although they applied them in different ways and at different times. Rates of staff injury from patient assaults from 1998 to 2000 suggest that the transition from a restraint culture did not put staff at greater risk of assault.
Because this is one of the larger studies on restrictive procedure use in a large hospital system, our findings were generally consistent with the data published thus far. Differences in the use of these restrictive measures between the three shifts (day and evening shifts compared with night shift) may be attributed to reduced levels of stimuli that would cause agitation and trigger aggression. Anecdotal evidence suggests that as patients became engaged in more purposeful activity during the day and evening hours, sleep patterns improved and there were fewer nocturnal behaviors. The same can be said of the variances between the use of these procedures during the week compared with weekends and holidays.
Our study did not show any racial, ethnic, or gender differences in the use of mechanical restraint throughout this study period. The rate of seclusion during the early years of this review was higher for racial or ethnic groups than for whites. However, as the rate of seclusion declined, the use of seclusion among racial and ethnic groups reduced at a faster rate. This difference and change may be attributed to increased attention to the data and more sensitivity by staff toward the overall use of seclusion.
Personal leadership by direct care staff who applied their nonrestraint values helped to change the culture of restraint within the system. The Pennsylvania advocacy community challenged the hospital system at the highest levels of state government to reduce the use of seclusion and restraint. Increased monitoring by staff and advocates in the day-to-day use of restrictive procedures, PERTs, policy changes, increased quantity and quality of patient programming, reduced unit size, and improved patient-to-staff ratios coupled with effective leadership at all levels of the hospital accounted for this transformation.
OMHSAS Deputy Secretary Curie's 1997 announcement that the use of seclusion and restraint constituted treatment failure was pivotal, because this announcement, when coupled with the resulting policy change, ended all debate within the hospital system about the nonrestraint approach. Curie stated, with hindsight, that if he had it to do all over again, he would have started sooner, pressed harder for this important change, and given greater credit to the direct care staff for the tremendous job that they did.
A challenge to Pennsylvania's seclusion and restraint reduction program is the perceived difference between the type of patients served in a state hospital system and those in other psychiatric acute care settings. Differences such as a lack of familiarity with patients who have shorter lengths of stays and the frequency at which a patient is in crisis somehow justifies, for some staff, greater dependence on the use of a restrictive procedure. Although this issue deserves further review, PERTs and similar response team programs that are designed to manage psychiatric crises in a nonoffensive manner have proven their effectiveness, regardless of a patient's length of stay. We recognize the need to work with other psychiatric acute care settings to obtain data and further study these differences.
Other issues that hospitals need to consider and measure are the effects that these changes will have on patient-to-patient and patient-to-staff assaults. Khadavi and colleagues (28) found an increase in "other-directed patient violence" during a 12-month study of three acute inpatient psychiatric units when seclusion and restraint were reduced. However, the authors acknowledge that their findings are at variance with previous reports. Owen and colleagues (29) found that the use of seclusion led to a significant number of violent incidents. Some warning sign preceded three-quarters of the serious violent incidents that they studied. They also found that the relationship between staffing level and violence was not clear. More female staff, more staff without psychiatric training or aggression management training, and more staff absenteeism had a positive relationship with violence, whereas younger staff and staff with high levels of psychiatric experience had a negative relationship with violence.
A study done in Norway found that most staff believed that using restraint or seclusion made patients calmer and did not cause aggression or anxiety. However, 70 percent of these same workers reported having been assaulted by patients in places where these interventions were used (30). Deescalation strategies are an essential part of minimizing the use of seclusion and restraint while preventing and managing aggressive behavior (31). Although one study suggested that fewer on-duty staff resulted in decreased use of seclusion (32), many studies have shown that increased staff-to-patient ratios with staff trained in recognizing the early signs of aggression and managing aggression result in reduced use of seclusion and restraint and a more therapeutic milieu (33,34,35,36,37,38,39,40,41,42).
It will also be important to measure and monitor the effect that these changes have on the use of STAT and PRN medications during emergencies. Additionally, seclusion and restraint may place a demand for more one-to-one patient-staff assignments.
Conclusions
In 2000 the Ford Foundation, in conjunction with Harvard University's John F. Kennedy School of Government, recognized the Pennsylvania state hospital system for its seclusion and restraint reduction program with the Innovations in American Government Award. Many factors contributed to the success of this effort, including improved patient-staff ratios and response teams. However, the nonrestraint values of hospital staff and community advocates with the administrative recognition that seclusion and restraint are not treatment modalities but treatment failures were the major reasons for the changes in attitude, culture, and environment within Pennsylvania's state hospital system.
Since the end of this study period the Pennsylvania state hospital system, civil and forensic, has continued to decrease its dependence on the use of these restrictive procedure. Currently, five of the nine hospitals have eliminated the use of seclusion. Danville State Hospital has gone more than two years without using mechanical restraint or seclusion. Since January 2005 the hospital system, which averages more than 60,000 days of care each month, has used seclusion only 19 times for a total of 18 hours. Mechanical restraint has been used 143 times for a total of 160 hours. This past spring the hospital system established a goal eliminating the use of mechanical restraint and seclusion by January 1, 2006.
Acknowledgments
This research project was funded, in part, by an award from the Ford Foundation in conjunction with Harvard University's John F. Kennedy School of Government and the Council for Excellence in Government through an Innovations in American Government Award. The authors thank Mary Ellen Rehrman, B.S., Charles Curie, M.S.W., Feather O. Houstoun, M.B.A., Joan L. Erney, J.D., and Estelle B. Richman, M.S., for their support of this transformational initiative. Finally, the authors gratefully acknowledge the work of Richard M. O'Dea, M.S., R.N.
Mr. Smith, Dr. Davis, Dr. Altenor, Ms. Altenor, Ms. Hardentstine, and Mr. Kopchick are affiliated with the Office of Mental Health and Substance Abuse Services of the Commonwealth of Pennsylvania in Harrisburg. Dr. Bixler and Dr. Lin are with the Pennsylvania State University School of Medicine in Hershey. Send correspondence to Mr. Smith at Allentown State Hospital, 1600 Hanover Avenue, Allentown, Pennsylvania 18109-2498 (e-mail, [email protected]). This article is part of a special section on the use of seclusion and restraint in psychiatric treatment settings.
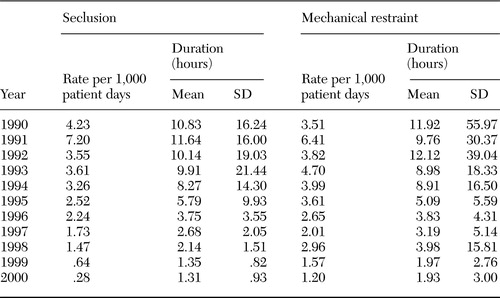 |
Table 1. Prevalence and duration of seclusion and mechanical restraint among adults who were civilly committed to state hospitals in Pennsylvania
1. Weiner DB: Phillippe Pinel's "Memoir of Madness" of December 11, 1794: a fundamental text of modern psychiatry. American Journal of Psychiatry 149:725–732,1992Link, Google Scholar
2. Soloff PH, Gutheil TG, Wexler DB: Seclusion and restraint in 1985: a review and update. Hospital and Community Psychiatry 36:652–657,1985Abstract, Google Scholar
3. Gutheil T: Observations on the therapeutic bases for seclusion of the psychiatric inpatient. American Journal of Psychiatry 135:325–328,1978Link, Google Scholar
4. Tomes N: The Art of Asylum-Keeping: Thomas Story Kirkbride and the Origins of American Psychiatry. Philadelphia, Penn, University of Pennsylvania Press, 1994Google Scholar
5. American Psychiatric Association Task Force Report 22: Seclusion and Restraint: The Psychiatric Uses. Washington, DC, American Psychiatric Association, 1985Google Scholar
6. Fisher WA: Seclusion and restraint: a review of the literature. American Journal of Psychiatry, 151:1584–1591,1994Link, Google Scholar
7. Busch AB, Shore MF: Seclusion and restraint: a review of recent literature. Harvard Review of Psychiatry 8:261–269,2000Crossref, Medline, Google Scholar
8. Mason T: Seclusion: an international comparison. Medicine, Science, and the Law 34(10):54–60,1994Google Scholar
9. Wynn R: Medicate, restrain, or seclude? Strategies for dealing with violent and threatening behavior in a Norwegian University Hospital. Scandinavian Journal of Caring Sciences 16:287–292,2002Crossref, Medline, Google Scholar
10. Cannon ME, Sprivulis P, McCarthy J: Restraint practices in Australasian emergency departments. Australian and New Zealand Journal of Psychiatry 35:464–467,2001Crossref, Medline, Google Scholar
11. Needham I, Abderhalden C, Dassen T, et al: Coercive procedures and facilities in Swiss psychiatry. Swiss Medical Weekly 132:253–258,2002Medline, Google Scholar
12. Dabrowski S, Frydman L, Zakowsha-Dabrowski T: Physical restraints in Polish psychiatric facilities. International Journal of Law and Psychiatry 8:369–382,1986Crossref, Medline, Google Scholar
13. Stokes ME, Davis CS, and Koch GG: Categorical Data Analysis Using the SAS System, 2nd ed. SAS Institute, Cary, NC, 2000.Google Scholar
14. Heagerty P, Liang K-Y, Zeger S, et al: Analysis of Longitudinal Data, 2nd ed. Oxford University Press, New York, 2002Google Scholar
15. Anthony WA: A recovery-oriented service system: setting some system level standards. Psychiatric Rehabilitation Journal 24:159–168,2000Crossref, Google Scholar
16. Pennsylvania Mental Health and Substance Abuse Bulletin on the Use of Restraints. Seclusion and Exclusion in State Mental Hospitals and Restoration Center, Jul 1, 2001. Harrisburg State Hospital, Harrisburg, Penn, 2001Google Scholar
17. Allentown State Hospital Policy Memorandum A-124, Psychiatric Emergency Response Plan, Allentown State Hospital, Allentown, Penn, 2002Google Scholar
18. Pennsylvania Community Hospital Integration Projects Program. Harrisburg State Hospital, Harrisburg, Penn, 1999Google Scholar
19. Slawich S, Leitzel L, Martin R: Manual for the Exclusion, Restraint, Protection, and Seclusion Reporting and Tracking System, Office of Mental Health, Allentown State Hospital, Allentown, Penn, 1995Google Scholar
20. Pennsylvania Mental Health and Substance Abuse Services Bulletin: Management of Incidents: SI-815 Incident Reporting and Risk Management Policy and Procedural Changes, SMH-03. Allentown State Hospital, Allentown, Penn, Jun 1, 2003Google Scholar
21. Fiorello S: Developing and implementing a statewide formulary system: one state's experience. Formulary 30:808–811,1995Medline, Google Scholar
22. Spivak B, Shabash E, Sheitman B, et al: The effects of clozapine versus haloperidol on measures of impulsive aggression and suicidality in chronic schizophrenia patients: an open, nonrandomized, 6-month study. Journal of Clinical Psychiatry 64:755–760,2003Crossref, Medline, Google Scholar
23. Citrome L, Volavaka J, Czobar P, et al: Effects of clozapine, olanzapine, risperidone, and haloperidol on hostility among patients with schizophrenia. Psychiatric Services 52:1510–1514,1995Link, Google Scholar
24. Chiles JA, Davidson P, McBride D: Effects of clozapine on use of seclusion and restraint at a state hospital. Hospital and Community Psychiatry 45:269–271,1994Abstract, Google Scholar
25. Mallya AR, Roos PD, Roebuck-Colgan K: Restraint, seclusion, and clozapine. Journal of Clinical Psychiatry 53:395–397,1992Medline, Google Scholar
26. Chengappa KNR, Levine J, Ulrich R, et al: Impact of risperidone on seclusion and restraint at a state psychiatric hospital. Canadian Journal of Psychiatry 45:827–832,2000Crossref, Medline, Google Scholar
27. Chengappa KNR, Vasile J, Levine J, et al: Clozapine: its impact on aggressive behavior among patients in a state psychiatric hospital. Schizophrenia Research 53:1–6,2002Crossref, Medline, Google Scholar
28. Khadivi A, Patel R, Atkinson A, et al: Association between seclusion and restraint and patient-related violence. Psychiatric Services: 55:1311–1312,2004Link, Google Scholar
29. Owen C, Tarantello C, Jones M, et al: Violence and aggression in psychiatric units. Psychiatric Services 49:1452–1457,1998Link, Google Scholar
30. Wynn R: Staff's attitudes to the use of restraint and seclusion in a Norwegian university psychiatric hospital. Nordic Journal of Psychiatry 57:453–459,2003Crossref, Medline, Google Scholar
31. Policy statement on the management of aggressive behavior in psychiatric institutions with special reference to seclusion and restraint. Washington, DC, American Academy of Child and Adolescent Psychiatry Council, Oct 24, 2000Google Scholar
32. Morrison EF: Violent psychiatric inpatients in a public hospital. Scholarly Inquiry for Nursing Practice: An International Journal 4:65–82,1990Medline, Google Scholar
33. Position Paper on Seclusion and Restraint. Alexandria, Va, National Association of State Mental Health Program Directors, Jul 1999Google Scholar
34. Schwartz T, Park T: Assaults by patients on psychiatric residents: a survey and training recommendations. Psychiatric Services 50:382–383,1999Link, Google Scholar
35. Kostecka M, Zardecka M: The use of physical restraints in Polish psychiatric hospitals in 1989 and 1996. Psychiatric Services 50:1637–1638,1999Link, Google Scholar
36. Leiberman R: CHARPP Seclusion and Retrain Update. Corvallis, Oreg, Child and Adolescent Residential Psychiatric Programs, 2003Google Scholar
37. D'Orio B, Purselle D, Stevens S, et al: Reduction of episodes of seclusion and restraint in a psychiatric emergency service. Psychiatric Services 55:581–583,2004Link, Google Scholar
38. Fisher WA: Elements of successful restraint and seclusion program and their application in a large, urban, state psychiatric hospital. Journal of Psychiatric Practice 9:7–15,2003Crossref, Medline, Google Scholar
39. Donovan A, Siegel L, Zera G, et al: Seclusion and restraint reform: an initiative by a child and adolescent psychiatric hospital. Psychiatric Services 54:958–966,2003Link, Google Scholar
40. Donat D: An analysis of successful efforts to reduce the use of seclusion and restraint at a public psychiatric hospital. Psychiatric Services 54:1119–1123,2003Link, Google Scholar
41. Jonikas J, Cook J, Rosen C, et al: A program to reduce use of physical restraint in psychiatric inpatient facilities. Psychiatric Services 55:818–820,2004Link, Google Scholar
42. SAMHSA action plan seclusion and restraint fiscal years 2004 and 2005. Washington, DC, Substance Abuse and Mental Health Services Administration, Jun 2004Google Scholar



