How Adolescents Perceive the Stigma of Mental Illness and Alcohol Abuse
Abstract
OBJECTIVES: Research among adults has yielded three sets of conclusions about the stigma of mental illness. First, people with mental illness are stigmatized more severely than those with physical health conditions; those who abuse alcohol are viewed more harshly than those with mental illness. Second, stereotypes of mental illness related to responsibility and dangerousness lead to negative emotional reactions and discriminatory behaviors. Third, familiarity with people with mental illness tends to diminish stigma. This study attempted to validate these findings with a large and diverse sample of adolescents. METHODS: A total of 303 adolescents completed a revised version of the Attribution Questionnaire (rAQ) that presented four vignettes, each describing a different type of peer: a peer with mental illness, with mental illness caused by a brain tumor, with alcohol abuse problems, and with leukemia. The rAQ comprises seven Likert scale items of agreement that research participants rated for each vignette. Items included pity, danger, fear, responsibility, anger, help, and avoidance. Participants also completed a revised Level of Contact Report to assess their familiarity with mental illness. RESULTS: As with adults, adolescents stigmatized peers who abuse alcohol most severely, followed by those with mental illness. Peers with leukemia were treated more benignly than the other groups. Having a brain tumor mediated the stigmatizing effect of mental illness. Adolescents who agreed that persons with mental illness are responsible for their illness and are dangerous demonstrated more discrimination toward these persons. However, this finding was not supported for alcohol abuse. Familiarity yielded an unexpected effect among adolescents; those who reported more familiarity with mental illness were more likely to endorse stigma of mental illness. CONCLUSIONS: Adolescents tended to discriminate among conditions, viewing substance abuse more harshly than the other disorders. Blame and dangerousness were important variables leading to discrimination, and contact with persons with mental illness led to more discrimination.
Research has shown that adults tend to stigmatize people with mental illness and people who abuse alcohol more harshly than they do those with other health conditions. Missing from this research has been studies that have examined this pattern among adolescents, which should be a research priority for several reasons. First, advocacy and government groups have argued that modifying negative attitudes among children and adolescents might stop them from developing into adults who stigmatize persons with mental illness, which can lead to full-blown social injustice (1,2). Second, differences in cognitive development between adolescents and adults challenge the simple extrapolation of findings from adult to adolescent samples.
Despite the importance of this topic, little research has been done. A recent review by Wahl (3) summarized studies done since 1980. Research was mostly descriptive, failing to test any of the better developed models of stigma. The studies lacked a clear definition of mental illness, failing to distinguish the stigma of this kind of condition from that of substance abuse. Sample sizes varied from 50 to 150, which are too small for path analytic strategies to be used. The goal of this study was to examine three aspects of mental health stigma, which have been fairly well substantiated among adults, in a large and diverse sample of adolescents.
The first aspect of the stigma of mental illness is that it is worse than that of other health conditions. Research has shown that people with mental illness are viewed as being more responsible for their condition than those with cancer or heart disease (4,5). People who abuse substances have been shown to be perceived as more blameworthy than those with mental illness. Findings from a nationwide probability sample showed that respondents viewed people with mental illness as being more dangerous than those with physical illnesses; people who abused alcohol were viewed as being more dangerous than those with mental illness (6,7). Extending these findings to our study, we hypothesized that adolescents will stigmatize peers who abuse alcohol more harshly than the other groups, followed by teens with mental illness. Individuals with cancer will be viewed more benignly.
Other work has sought to extend basic findings about differences in stigma across health conditions to examine how specific stereotypes lead to discriminatory behavior. One model, based on Weiner's attribution theory (8), posits that individuals who view people as responsible for their mental illness or alcohol abuse will likely be angry with them and will not be willing to help them. Conversely, members of the general public who view people as victimized by their mental illness or alcohol abuse will be likely to experience pity and be willing to help. We applied Weiner's model to mental illness and validated it with a large sample of adults (9).
Another, equally important stereotype related to mental illness and alcohol abuse is dangerousness. On the basis of existing studies (10,11), we argued that viewing people who have mental illness or abuse alcohol as dangerous would lead to fear, which in turn would yield social avoidance. We validated this assumption with a large sample of adults (9) and hoped to repeat the study with adolescents. Models that examine whether feelings of responsibility and dangerousness lead to stigmatization of alcohol abuse have not been previously tested. Hence, the study reported here represents the first application of these models to the stigma of alcohol abuse.
The third aspect of the stigma of mental illness that we investigated is that familiarity with mental illness mediates stigma. Attitudinal and emotional responses toward persons with mental illness, including beliefs about responsibility and dangerousness, are likely to be influenced by familiarity with serious mental illness. Previous research has found familiarity to be inversely associated with prejudicial attitudes about mental illness (12,13,14,15). Other research has found that contact with persons with mental illness reduces fear (16). In the study reported here, we considered the role of familiarity as a moderator of stereotypes about responsibility and dangerousness. Note that at the time we conducted this study, we had only a validated measure of familiarity with mental illness, so these models were tested for stigma of mental illness and not for stigma of alcohol abuse.
Methods
Approximately 750 students from three high schools in Southern California were recruited as part of a larger study that examined the impact of an antistigma program that was conducted by the National Mental Health Awareness Campaign from October to December 2003. Data from a subsample of 303 students who had completed all measures relevant to our hypotheses were included in our analyses. These data were originally collected as part of a program evaluation conducted by another group. This group collected information from 408 students (57 percent) before the presentation on an antistigma program and from 303 students (43 percent) after the presentation. Issues related to confidentiality and other protections for participants were worked out between school principals and program evaluators. The investigators used the secondary data to test the hypotheses outlined in this paper and received approval from the institutional review boards at Evanston Northwestern Healthcare and the University of Maryland in Baltimore.
Research participants completed the revised Attribution Questionnaire (rAQ), an instrument that measures the seven factors of interest: responsibility, pity, anger, dangerousness, fear, help, and avoidance (17). The original AQ consisted of a brief statement about Harry, a 30-year-old single man with schizophrenia. The vignette is very brief to better represent the respondent's reaction to the schizophrenia label rather than to other information. The original AQ consisted of 27 items on a 9-point agreement scale. Three items were written to represent each of the seven factors. The factor structure and reliability of the AQ were validated in two confirmatory factor analyses (9,18).
The original AQ was revised for this study. First, the vignette was changed to represent a youth: "Brandon is a new student in your class. Before his first day, your teacher explained that Brandon is mentally ill and is transferring from a special school." Second, three additional parallel forms of the AQ were written with equally short vignettes: Joshua who "has a drinking problem," Tyler who "has a brain tumor that makes him act like he has a mental illness sometimes," and Ryan who "has leukemia, a cancer of the blood." Finally, the rAQ reduced the number of items to generate a short test of stigma. On the basis of results from our previous confirmatory factor analyses, the single item that loaded most highly into the seven factors was incorporated into the rAQ (9). Hence, participants were asked to complete a 9-point Likert scale of agreement for seven items immediately after reading each of the four vignettes. The scale ranged from 1, not at all, to 9, very much.
Research participants also completed a revised version of the Level of Contact Report (14) to assess familiarity with mental illness. The original Level of Contact Report lists 12 situations that vary in intimacy with persons with mental illness. These situations were adapted from other scales used in stigma research (19,15) and varied from least intimate contact ("I have never observed a person that I was aware had a serious mental illness") to high intimacy ("I have a mental illness"). The reliability and validity of the measure have been demonstrated in three studies (12,13,14). Situations for the adolescent version of the scale were reduced to eight and made relevant to that age group—for example, "I have a person in my class with mental illness." Scores on the revised version ranged from 0 to 7, with higher scores showing higher familiarity with mental illness. The index for familiarity in this study was the rank score of the most intimate situation indicated by the participant. For example, a research participant who checked two situations from the test—"A friend of the family has a severe mental illness" (score of 4) and "I live with a person who has a severe mental illness" (score of 6)—would receive a score of 6 because "Living with a person who has a severe mental illness" is the most intimate of the checked situations.
Results
Participants
The subsample consisted of 171 females (56 percent), and participants varied in age from 13 to 19 years (mean±SD age, 16.4±2.5 years). In terms of race or ethnicity, 18 participants (6 percent) reported that they were Asian American, 19 (6 percent) were black, 39 (13 percent) were Hispanic, two (1 percent) were Native American, and 186 (61 percent) were white. The remaining 39 (13 percent) identified two or more racial or ethnic groups.
Differences in stigma across health conditions
Mean scores on the seven items from the rAQ across the four vignettes are summarized in Table 1. Results of subsequent repeated-measures analyses of variance for each of the rAQ items yielded highly significant (p<.001) and similar findings across all items. Post hoc contrasts showed that alcohol abuse was stigmatized significantly more than the other illnesses. Leukemia was judged more benignly. Mental illness was stigmatized more than leukemia for pity, dangerousness, fear, help, and avoidance. These findings largely correspond with those of Pescosolido and colleagues (6). Stating that the mental illness was caused by a brain tumor moderated stigmatizing effects. Compared with the vignette describing a teen with mental illness without an organic cause, the vignette describing a teen with a brain tumor had lower stigma scores for pity, dangerousness, and fear.
Path models of responsibility and dangerousness
Path analysis with manifest variables was used to test theoretical models because it is one of the more robust data analytic strategies to determine the size and direction of associations among a set of variables. All analyses were conducted with the SAS system's covariance analysis of linear structural equations (20), used the maximum likelihood method of parameter estimation, and were performed on the variance-covariance matrix.
Table 2 presents goodness-of-fit indexes for the various path models. Path models described responsibility, dangerousness, responsibility mediated by familiarity, and dangerousness mediated by familiarity. The chi square statistic included in this table provides a test of the null hypothesis, which states that the reproduced covariance matrix has the specified model structure. Nonsignificant chi square statistics support good fit; however, the statistic is sensitive to sample size and departures from multivariate normality and may often result in the rejection of a well-fitting model. Alternatively, goodness of fit has been supported when the chi square to df ratio is below 2.0.
Table 2 also includes three additional fit indexes: the comparative fit index, the nonnormed fit index, and the normed fit index (21,22). Scores on these indexes vary from 0 to 1 and are considered to support fit when they are greater than .90. Finally, Table 2 includes standardized coefficients that represent the size of the association of individual paths within each model. T values for individual coefficients that are greater than 1.96 are significant (p<.05).
Table 2 summarizes the responsibility path model for mental illness. Chi square statistics for the model were nonsignificant, which indicated that the model was a good fit. Moreover, the chi square to df ratio was less than 2.0 and the comparative fit index, the nonnormed fit index, and the normed fit index were greater than .90. Standardized coefficients for the elements of all the models were significant. Combined, these findings suggest that the data fit the model adequately. Table 2 also shows the individual path coefficients, which demonstrate the strength of the relationships between individual elements of the path model. Willingness to help was positively associated with pity and inversely associated with anger. Responsibility inversely predicted pity and directly predicted anger.
Table 2 also summarizes indexes for the dangerousness path model that predicted avoidance for mental illness. Fit indicators were mixed for this model. Chi square analysis did not support a good fit. However, the comparative fit index and the normed fit index supported a good fit, and the nonnormed fit index approached .90. The two standardized path coefficients were significant. Fear was positively associated with avoidance (R2=.26), and danger was positively correlated with fear (R2=.53).
Goodness-of-fit indicators for the path model that represented responsibility attributions for alcohol abuse were mixed. As summarized in Table 2, the chi square statistic was highly significant (p<.001), and the chi square to df ratio was well above 2.0. However, two of the three remaining fit indicators exceeded .90; the third one was close to .90. Despite the lack of good fit, path coefficients showed that the relationship between responsibility and alcohol abuse were similar to the relationship between responsibility and mental illness. Responsibility was inversely associated with pity and directly associated with anger. In turn, pity was directly associated with help. Anger and help were inversely related.
Goodness-of-fit indicators did not support the dangerousness path model for alcohol abuse. Neither chi square statistics nor the remaining fit indicators met criteria for a good fit. Nevertheless, the path coefficients were significant and similar to those found in the dangerousness path model for mental illness.
The moderating effect of familiarity
Table 3 shows the number of adolescents who responded yes to each of the familiarity items on the revised Level of Contact Report. Only 11 percent of the sample reported never observing a person with mental illness. Twenty-eight percent of the sample reported having friends or relatives with serious mental illness.
Table 2 also summarizes the responsibility and dangerousness path models with familiarity as a moderating variable. This analysis was limited to the stigma of mental illness because familiarity with alcohol abuse was not assessed in our study. The chi square statistic was nonsignificant, and the chi square to df ratio was below 2.0 for the responsibility model with familiarity as a moderating value. The remaining fit indicators were all above .90. Combined, these statistics suggest that the responsibility path model with familiarity as a moderating variable adequately fit the data. The path coefficients show a small but significant relationship between familiarity and responsibility. Interestingly, this relationship is in the opposite direction than expected. Namely, adolescents who reported higher familiarity were likely to attribute greater responsibility to people for their mental illness.
Fit indicators for the dangerousness path model with familiarity as a moderating variable were mixed. The chi square test was significant, and the chi square to df ratio was above 2.0. However, two of the other fit indicators—comparative fit index and normed fit index—were above .90; the third indicator approached .90. The path coefficient between familiarity and dangerousness was significant, although small (R2=.005). Once again, the direction of this relationship is counterintuitive; adolescents with more familiarity were likely to view peers with mental illness as more dangerous.
We examined whether race or ethnicity or gender interacted with familiarity to influence the path models. Analyses did not find any significant role for these demographic characteristics.
Discussion
This study sought to extend models of stigma of mental illness and alcohol abuse that had been validated with adults to adolescents. Results showed that adolescents tended to differentiate among health conditions in a manner similar to those of adults. Specifically, peers who abuse alcohol were viewed more negatively than those with mental illness or leukemia, especially in terms of blame, anger, and dangerousness. Adolescents with leukemia were viewed more benignly than adolescents in the other groups. Stigma ratings of mental illness typically fell between the other two health conditions. Interestingly, stigma diminished when mental illness was reported to be caused by a brain tumor. Research participants rated the teen with the brain tumor as less dangerous, less likely to be feared, more worthy of help, and less likely to be avoided than the teen with mental illness without organic cause. One might think that this difference is due to blaming the teen with the brain tumor less. However, our results showed no difference between the two groups on responsibility attributions. Future research is needed to determine what might account for this difference.
In addition to the analysis of group differences, path analyses from our study with adolescents also seemed to validate the dangerousness path models for mental illness and the responsibility path model for mental illness with familiarity as a moderating value. Goodness-of-fit indicators were sufficient, and path coefficients were significant. As expected, adolescents who viewed peers as responsible for their mental illness tended to have less pity and be angrier. Pity was directly linked to helping, whereas anger showed an inverse relationship to helping. In terms of dangerousness, adolescents who viewed peers as dangerous tended to fear and avoid them.
Results were less clear for the responsibility and dangerousness path models for alcohol abuse. Many of the goodness-of-fit indicators did not support the models. However, all the individual path coefficients from the path models for alcohol abuse mirrored those found for mental illness and were markedly higher in some cases. Adolescents who blamed peers for alcohol abuse tended to be angry, less sympathetic, and less likely to offer help than adolescents who blamed peers for mental illness. Similarly, research participants who viewed teens who abuse alcohol as dangerous tended to fear and avoid them.
The difference between the findings for the path models for mental illness and alcohol abuse, which was implied by differences in fit indicators and path coefficients, suggests that there are additional moderating or mediating variables that might explain why the path model for alcohol abuse did not have sufficient goodness of fit. Two such variables that are positively associated with both responsibility and dangerousness are conservative political preference and authoritarian personality (23). Future research needs to determine which among a set of variables like these better fit the models for alcohol abuse. Alternatively, limited fit indicators may represent restricted range on some of the rAQ items. Several indicators seemed to show a floor effect. In addition, limited fit indicators and restricted range may reflect some of the nebulous quality of these measures of stigma. Given the mixed evidence on violence and mental illness—that is, some studies have suggested that people with mental illness are more violent than the general population, whereas others have implied that public perception of dangerousness far exceeds any real difference (24,25)—it is not unequivocally true that endorsing rAQ items about dangerousness necessarily means the participant was endorsing false, stigmatizing attitudes.
Data on familiarity provided some interesting findings. Adolescents seem to have a fair amount of contact with people with mental illness. About half the sample was aware of at least one classmate who had a serious mental illness. Interestingly, the impact of familiarity on stigma did not correspond to the pattern found among adults. Namely, teens who reported being more familiar with mental illness endorsed greater attributions of responsibility and dangerousness to those with mental illness. Rather than diminish stigma, contact seemed to increase it.
This finding may represent a statistical artifact. Although the path coefficients were significant for the models, their effect size was very small. In addition, the range of scores on the revised Level of Contact Report was restricted, thereby limiting the power of analyses. Data from the sample in this study are tainted because some of the students were exposed to the antistigma program. Future research needs to obtain a cleaner data set.
Assumptions about familiarity having a moderating effect need to be reconsidered in future research. It is alternatively conceivable that familiarity could mediate already strong connections between responsibility and help or between dangerousness and avoidance. For example, perhaps adolescents who avoid people with mental illness because they believe they are dangerous would mediate those beliefs after they meet "docile" peers with mental illness. Future research needs to examine alternative path models that examine the relationship between familiarity and responsibility or dangerousness.
However, if this effect is replicated in future research it may suggest an effect that is caused by cognitive development. Compared with adults, adolescents have less information and more tentatively formed attitudes about people with mental illness. Hence, contact may not stimulate accommodation because the teen has less preexisting information as a base on which to develop feelings of accommodation. Alternatively, research has shown that the effects of familiarity and contact vary with the type of contact. Meeting people who challenge the stereotypes of mental illness can lessen stigma, and interacting with people who reinforce the stereotype—for example, a peer with psychosis who needs to be hospitalized to protect his family—can worsen the stereotype. Absent from our research was information about the kind of contact experienced by research participants. Perhaps experience of the teens in this study was consistent with the stereotypes—for example, they met a violent person with mental illness.
Some additional limitations of this study need to be considered in future research. Although the study recruited a large and diverse group, it was limited because it did not include a probability sample. Future research should attempt to use population strategies to replicate these findings. Note that although the generalizability of findings is limited, this is not a fatal flaw because the goals of this study were to test hypotheses and not to provide descriptive analyses. Future research should also examine the role of demographic characteristics—for example, gender and race or ethnicity of the respondent—as well as area-level descriptors—for example, type of school or neighborhood—in path models.
A final concern: the purpose of this study was to determine whether characteristics of adolescence, such as cognitive development, accounted for a different pattern of stigma from that found among adults. Future research could more directly test the role of cognitive development by including an independent measure of the construct. Moreover, future research needs to further extend this discussion by examining how children who are even younger perceive mental illness.
Conclusions
Research like this is a necessary first step for developing antistigma programs meant to target American teens. For example, information showed that teens tended to discriminate among psychiatric conditions, viewing substance abuse more harshly; that they tended to view blame and dangerousness as important variables leading to discrimination; and that contact may have had a paradoxical effect on them. This kind of information provides a starting point for developing programs to diminish stigma. With this kind of information, researchers and advocates can join forces to strategically evaluate these plans for antistigma programs.
Dr. Corrigan, Ms. Slopen, and Dr. Medasani are affiliated with the Center for Psychiatric Rehabilitation at Evanston Northwestern Healthcare, 1033 University Place, Evanston, Illinois 60201 (e-mail, [email protected]). Ms. Lurie is with Mental Health Media Partnership in Los Angeles. Dr. Goldman is with the department of psychiatry at the University of Maryland in Baltimore. Mr. Phelan is with the School of Public Health at the University of Minnesota in Minneapolis.
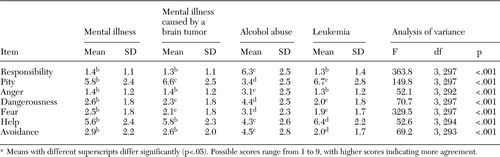 |
Table 1. Scores of 303 adolescents on items of the revised Attribution Questionnaire to measure their feelings toward peers with illness, by health condition of the peersa
a Means with different superscripts differ significantly (p<.05). Possible scores range from 1 to 9, with higher scores indicating more agreement.
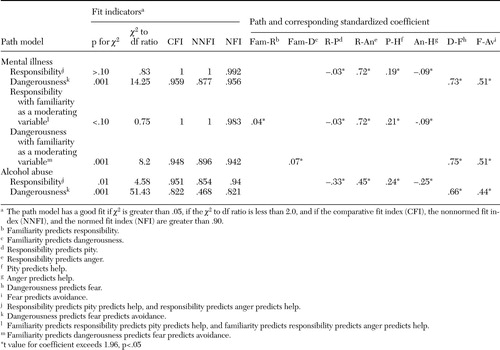 |
Table 2. Summary of structural equation models for responsibility attribution and dangerousness describing the feelings of 303 adolescents toward peers with illness
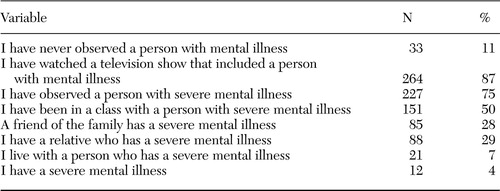 |
Table 3. Participants who responded affirmatively to questions about familiarity with mental illness among 303 adolescents, as measured by the modified Level of Contact Report
1. National Mental Health Awareness Campaign. Available at www.nostigma.orgGoogle Scholar
2. Mental Health: A Report of the Surgeon General. Washington, DC, Department of Health and Human Services, Office of the Surgeon General, 1999Google Scholar
3. Wahl OF: Children's views of mental illness: a review of the literature. Psychiatric Rehabilitation Skills 6:134–158, 2002Crossref, Google Scholar
4. Corrigan PW, River L, Lundin RK, et al: Stigmatizing attributions about mental illness. Journal of Community Psychology 28:91–102, 2000Crossref, Google Scholar
5. Weiner B, Perry RP, Magnusson J: An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology 55:738–748, 1988Crossref, Medline, Google Scholar
6. Pescosolido BA, Monahan J, Link BG, et al: The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problem. American Journal of Public Health 89:1339–1345, 1999Crossref, Medline, Google Scholar
7. Phelan JC, Link BG, Stueve A, et al: Public conceptions of mental illness in 1950 and 1996: what is mental illness and is it to be feared? Journal of Health and Social Behavior 41:188–207, 2000Google Scholar
8. Weiner B: Judgments of Responsibility: A Foundation for a Theory of Social Conduct. New York, Guilford Press, 1995Google Scholar
9. Corrigan PW, Markowitz FE, Watson AC, et al: An attribution model of public discrimination towards persons with mental illness. Journal of Health and Social Behavior 44:162–179, 2003Crossref, Medline, Google Scholar
10. Edwards JM, Endler NS: Appraisal of stressful situations: personality and Individual Differences 10:7–10, 1989Crossref, Google Scholar
11. Paterson RJ, Neufeld RW: Clear danger: situational determinants of the appraisal of threat. Psychological Bulletin 101:404–416, 1987Crossref, Medline, Google Scholar
12. Corrigan PW, Edwards AB, Green A, et al: Prejudice, social distance, and familiarity with mental illness. Schizophrenia Bulletin 27:219–225, 2001Crossref, Medline, Google Scholar
13. Corrigan PW, Green A, Lundin R, et al: Familiarity with and social distance from people who have serious mental illness. Psychiatric Services 52:953–958, 2001Link, Google Scholar
14. Holmes E, Corrigan PW, Williams P, et al: Changing attitudes about schizophrenia. Schizophrenia Bulletin 25:447–456, 1999Crossref, Medline, Google Scholar
15. Penn DL, Guynan K, Daily T, et al: Dispelling the stigma of schizophrenia: what sort of information is best? Schizophrenia Bulletin 20:567–578, 1994Google Scholar
16. Link BG, Cullen FT: Contact with the mentally ill and perceptions of how dangerous they are. Journal of Health and Social Behavior 27:289–302, 1986Crossref, Medline, Google Scholar
17. Watson AC, Otey E, Westbrook A, et al: Challenging middle schooler's attitudes about mental illness through science education. Schizophrenia Bulletin 30:563–572, 2004Crossref, Medline, Google Scholar
18. Corrigan PW, Rowan D, Green A, et al: Challenging two mental illness stigmas: personal responsibility and dangerousness. Schizophrenia Bulletin 28:293–310, 2002Crossref, Medline, Google Scholar
19. Link BG, Cullen FT, Frank J, et al: The social rejection of former mental patients: understanding why labels matter. American Journal of Sociology 92:1461–1500, 1987Crossref, Google Scholar
20. Hatcher L: A Step-by-Step Approach to Using the SAS System for Factor Analysis and Structural Equation Modeling. Cary, NC, SAS Institute, Inc, 1994Google Scholar
21. Bentler PM: EQS Structural Equations Program Manual. Los Angeles, BMDP Statistical Software, 1989Google Scholar
22. Bentler PM, Bonett DG: Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin 88:588–606, 1980Crossref, Google Scholar
23. Watson AC, Corrigan PW, Angell B: What motivates public support for legally mandated mental health treatment? Manuscript submitted to Social Work Research, in pressGoogle Scholar
24. Swanson JW, Holzer CE, Ganju VK, et al: Violence and psychiatric disorder in the community: evidence from the Epidemiological Catchment Area surveys. Hospital and Community Psychiatry 41:761–770, 1990Abstract, Google Scholar
25. Monahan J, Arnold J: Violence by people with mental illness: a consensus statement by advocates and researchers. Psychiatric Rehabilitation Journal 19:67–70, 1996Crossref, Google Scholar



