Datapoints: Use of Prescription Psychiatric Drugs and Religious Service Attendance
Over their lifetime, persons with mental disorders seek initial treatment from clergy more frequently than from psychiatrists or general medical doctors, and a majority who seek treatment from clergy do so to the exclusion of other providers (1). However, little is known about the relationship between religion and use of the mental health care system.
We examined the use of prescription mental health medications and religious service attendance. Persons who attend more frequently may be more likely to seek help from clergy than from mental health professionals. We focus on medications to reduce ambiguity about the religious affiliation of mental health providers.
We used data from the 2003 National Survey on Drug Use and Health (NSDUH) (2). We measured rates of medication use among adults (unweighted N= 10,126) who had one or more symptoms of mental disorders in the past year. Symptoms of mental disorders were measured by using questions adapted from the Composite International Diagnostic Interview-Short Form (3).
We estimated that 32 percent of those with a symptom of mental disorders used a prescription medication to treat a mental or emotional problem in the past year. Table 1 shows the relationship between attendance and prescription use. We did not find any statistically significant variation in the rate of medication use across attendance categories. We also did not find any evidence that number of disorder symptoms played a mediating role in the association between attendance and medication use.
Some have expressed concern that reliance on clergy may prevent or delay the appropriate use of mental health care (1). However, our data do not support the notion that frequent religious participation is associated with barriers to the use of the formal mental health system.
Acknowledgments
This work was supported by the Substance Abuse and Mental Health Services Administration and by a Research Career Development Award (RCD-03-036) from the Department of Veterans Affairs. This report does not necessarily represent the policies or positions of the Substance Abuse and Mental Health Services Administration or the Department of Veterans Affairs.
Dr. Harris and Dr. Larson are affiliated with the Office of Applied Studies at the Substance Abuse and Mental Health Services Administration, 1 Choke Cherry Lane, Rockville, Maryland 20857 (e-mail, [email protected]). Dr. Edlund is with the Center for Mental Healthcare and Outcomes Research at the Central Arkansas Veterans Healthcare System. Harold Alan Pincus, M.D., and Terri L. Tanielian, M.A., are editors of this column.
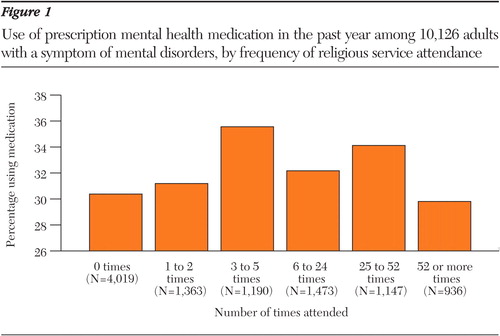
Figure 1. Use of prescription mental health medication in the past year among 10,126 adults with a symptom of mental disorders, by frequency of religious service attendance
1. Wang P, Berglund P, Kessler R: Patterns and correlates of contacting clergy for mental disorders in the United States. Health Services Research 38:647–673, 2003Crossref, Medline, Google Scholar
2. Results From the 2003 National Survey on Drug Use and Health: National Findings. National Survey on Drug Use and Health series H-25, DHHS pub no SMA 04–3964. Substance Abuse and Mental Health Services Administration, Office of Applied Studies, Rockville, Md, 2004Google Scholar
3. Kessler R, Andrews G, Mroczek D, et al: The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). International Journal of Methods in Psychiatric Research 7:171–185, 1998Crossref, Google Scholar



