Disparities in Depression Treatment for Latinos and Site of Care
Abstract
OBJECTIVE: This study examined the impact of patient characteristics and source of care on differences between whites and Latinos in use and quality of depression treatment in managed primary care settings. METHODS: Data were examined for 1,175 patients (398 Latinos and 777 whites) in 46 managed primary care practices who screened positive for probable depressive disorder. Patient baseline assessments were used to compile sociodemographic and clinical characteristics and to derive variables for receipt of any depression care and depression care that met minimum guidelines (antidepressant use or specialty counseling) in the past six months. Clinics were classified by the percentage of their patient population that consisted of Latinos to determine whether patients in highly Latino clinics reported lower rates of care. Predictors of use and quality of depression care were examined by using logistic regression. RESULTS: Rates of receipt of any depression care and guideline-level depression care were low, and Latinos were less than half as likely as whites to receive such care, even after the analyses controlled for independent predictors (that is, younger age, higher educational level, current unemployment, more comorbid medical illness, and a diagnosis of a depressive or anxiety disorder). The likelihood of receiving any care or care that met guidelines did not significantly vary according to whether clinics served a low, moderate, or high percentage of Latinos. CONCLUSIONS: Disparities in depression care for Latinos were not attributable to sociodemographic and clinical characteristics, and they were not attributable to receiving care in clinics that served ethnically similar or dissimilar clientele. These findings suggest that other patient or provider factors may be responsible.
The recent Supplement to the Report of the Surgeon General on Mental Health found that in the United States Latinos with mental disorders are much less likely than whites to use mental health care (1). Fewer than one in 11 Latinos with mental disorders seeks care from mental health care specialists, and fewer than one in five seeks care from general health care providers (2). These rates are even lower for immigrants with mental disorders, with one in 20 seeing a mental health specialist and one in ten seeing a general health care provider (3).
Although poor access through lack of insurance has been one explanation for low rates of care (4), evidence suggests that even among patients with insurance and a regular source of care, Latinos are still less likely than whites to be given a diagnosis of depression and to receive depression care (5,6). Latinos with depressive or anxiety disorders who have seen a health care provider in the previous year are less likely than whites with similar disorders to receive treatment concordant with evidence-based practice guidelines, regardless of insurance status (24 percent of Latinos compared with 34 percent of whites in a national survey) (6).
These disparities may be related to patient and clinic factors. Patient factors may include differences in sociodemographic characteristics (for example, education and income), clinical status (for example, depression severity and comorbid disorders), or attitudes (for example, problem recognition, illness beliefs, and social norms). The clinics that Latinos frequent may have fewer resources for programs that offer depression care or culturally relevant services (7,8,9,10,11,12).
We conducted a secondary analysis of baseline data from Partners in Care (PIC), a national quality improvement intervention for depression that was implemented in managed primary care settings (13,14). We sought to determine whether differences in use and quality of depression care continue to exist among depressed primary care patients by studying a sample of patients who were in managed care plans and had access to a regular source of care. We first examined the demographic and clinical characteristics of the patients and the characteristics of clinics that serve low, moderate, and high proportions of Latino clientele. We then examined whether potential disparities in depression care for Latinos in the sample were associated with these factors.
Methods
We used baseline data from PIC, a group-level randomized controlled trial described in detail elsewhere (13,14) and funded by the Agency for Healthcare Research and Quality (AHRQ). The study was approved by the institutional review boards of all participating institutions and RAND, and informed consent was obtained from all patients and clinicians.
Participants
Organizations, clinics, and providers. Six nonacademic managed care organizations were selected that were diverse in geography and organizational structure. Mexican Americans were oversampled. Participating organizations were located in Los Angeles; San Antonio; Twin Cities, Minnesota; San Luis Valley, Colorado; and Columbia, Maryland. These organizations included various types of practices—prepaid, staff model, mixed fee-for-service and prepaid, and network model—as well as rural, managed public health clinics. Among the 48 primary care practices within participating regions with at least two clinicians, 46 participated (96 percent). Among the 183 providers within these clinics, 181 (99 percent) participated, 167 (92 percent) of whom completed a 20-minute, self-administered clinician background questionnaire.
Patients. Consecutive patient visitors were screened over a five- to seven-month period between June 1996 and March 1997. Patients were eligible for the study if they were aged 18 years or older, intended to use the clinic as their main source of care for the next year, and had current depressive symptoms according to a six-item screening instrument that included the four stem items for major depressive and dysthymic disorders from the 12-month Composite International Diagnostic Interview (CIDI), edition 2.1 (15). Also included were two parallel items, written in CIDI format, to assess the presence of depression in the past month. Persons with positive responses to both a 12-month and a 30-day item were scored as having a possible depressive disorder. Patients with an acute medical emergency, who did not speak either English or Spanish, or who did not have insurance or a public-pay arrangement that covered the study intervention were excluded.
Among the 27,332 patients screened, 3,918 (14 percent) were potentially eligible for the study, but many of these patients left the clinic before completing the multistage enrollment process. Among the 2,417 patients who were asked to hear about the study and were present to confirm their insurance eligibility, 296 were not eligible for the study. Among the remaining patients, 1,356 (64 percent) were eventually enrolled; these analyses were restricted to the 398 Latinos (29 percent) and the 777 whites (57 percent) who identified themselves as such on one item asking them if they were Latino/Latina/Latin American/Hispanic; Asian; black/African American; Native American/American Indian/Indigenous People; Pacific Islander; or white. Although countries of origin were not assessed at baseline, among the 294 Latinos (74 percent) who completed the 18-month study assessment, 216 (73 percent) were Mexican or Mexican American, 21 (7 percent) were Caribbean, seven (2 percent) were Central American, five (2 percent) were South American, and the remaining 45 (15 percent) did not specify. A majority of Latino patients were from Southern California, Texas, and Colorado.
Enrolled patients completed the CIDI affective disorders section to determine depressive diagnoses. They also completed a telephone interview to determine the presence of comorbid anxiety disorders (as determined by the CIDI anxiety disorders section) as well as to gather data on income, wealth, and employment. Self-administered mail surveys were also obtained at baseline. Survey response rates were 95 percent for the telephone interview and 88 percent for the baseline survey. Data were weighted for both the probability of enrollment and survey response.
Measures
Use and quality of depression care. Information from the patient baseline surveys was used to construct variables for any use of care and minimum quality care. Any use of care in the previous six months was defined as taking any antidepressant medication or having any counseling from a mental health specialist. Minimum quality care variables were derived by using AHRQ treatment guidelines (16,17). Effective dosage ranges for the newer antidepressants that were not included in the guidelines were developed. Minimum quality care in the previous six months was thus defined as receiving any antidepressant medication at a daily dosage concordant with guidelines (that is, at or above the minimum daily dosage) for at least 25 of the past 30 days or having at least four specialty mental health visits that used an active cognitive-behavioral component (for example, engaging in pleasant activities and solving problems).
Patient sociodemographic and clinical characteristics. Sociodemographic and clinical factors included gender; age; marital status; education; employment status; net worth, as calculated by summing the net value of the home and other assets (18); and number of chronic medical diseases. Acculturation was measured with a 12-item adaptation of a measure from the Hispanic Health and Nutrition Examination Survey (19); possible mean scores range from 1, low acculturation, to 5, high acculturation. Depressive symptom severity was measured with the Center for Epidemiologic Studies Depression Scale (20). The CIDI was used to determine depressive diagnoses. Patients were then classified into two groups: the first included patients with current major depression, dysthymia, or both, and the second included those with current depressive symptoms that did not meet diagnostic criteria. The presence of an anxiety disorder was defined as meeting CIDI criteria for panic disorder, agoraphobia, social phobia, or generalized anxiety disorder in the past year. Alcohol abuse was defined as having a score of 8 or higher on the Alcohol Use Disorders Identification Test (21), and drug use was determined by whether patients reported using any drug of abuse either on their own or not as prescribed by their doctor. Patients were not compensated for participating in the interview.
Provider characteristics. The clinician background questionnaire was used to measure age, gender, ethnicity, Spanish-speaking ability, specialty, board certification status, number of years in practice, mean number of clinic visits per week, mean number of minutes for both new and follow-up visits, depression knowledge (based on a 13-item battery that assessed knowledge of AHRQ guidelines), any participation in the past three years in continuing medical education that dealt with depression, and the extent to which clinicians perceived that lack of access to mental health providers limited their treatment of depression (does not limit, limits somewhat, and limits a great deal).
Ethnicity of the clinic population. Information about ethnicity from the 27,332 patients who completed the initial screening process was used to characterize the 46 individual clinics according to the percentage of their population that was made up of Latino patients. The clinics ranged from less than 1 percent Latino to more than 96 percent Latino. At 13 clinics (28 percent) less than 10 percent of patients were Latino, at 20 (43 percent) between 11 and 49 percent were Latino, and at 13 (28 percent) 50 percent or more were Latino.
Data analysis
We conducted patient-level analyses to compare the sociodemographic and clinical characteristics of Latino and white medical patients and their use of depression care, using chi square analyses and t tests to examine significant differences between the two groups. We also conducted analyses using chi square analyses and F test statistics, as appropriate, to compare clinician characteristics in clinics serving low, moderate, or high proportions of Latinos. Logistic regression models were used to examine patient-level predictors of receipt of any depression care or quality depression care, including ethnicity as the main independent variable as well as sociodemographic and clinical variables that differed between the two groups as covariates. A logistic regression model was also used to examine the relationship between the proportion of Latinos served by clinics and the likelihood that patients received any depression care or depression care that met guideline criteria. The model included ethnicity, the presence of a currently diagnosable depressive or anxiety disorder (to control for need), a continuous variable representing the percentage of Latinos in each clinic, and an interaction term of ethnicity by percentage of Latinos in each clinic. Cluster adjustments for within-class correlations at the provider and clinic levels were included in the analyses. To account for missing data, we imputed five data sets, averaged responses, and adjusted standard errors for uncertainty caused by imputation.
Results
Demographic and clinical characteristics and depression care
The sociodemographic and clinical characteristics of the Latino and white patient subgroups are presented in Table 1. Compared with whites, Latinos were significantly younger, had less formal education, were less likely to be employed, and reported less household wealth. The mean±SD acculturation score for Latinos was 3.12±.97. Only 19 percent of the Latino patients chose to complete study assessments in Spanish. Clinically, Latinos were significantly more likely than whites to have comorbid anxiety disorders and less likely to have reported illicit use of drugs during the previous six months.
Although all patients were in managed care, Latinos were significantly less likely than whites to receive any depression care or depression care that met the guideline criteria. Within the past six months, only 31 percent of Latinos, compared with 50 percent of whites, had received any antidepressants or attended any specialty counseling. In terms of the quality of care, only 19 percent of Latinos had received the minimum level of antidepressant treatment or counseling, compared with 36 percent of whites.
Clinic characteristics
Table 2 describes the characteristics of providers in clinics with low, moderate, and high proportions of Latino patients. Among the three groups, significant differences were seen in the percentage of clinicians who spoke Spanish, were from a racial or ethnic minority group, or were board certified; significant differences were also seen in clinicians' age and mean number of visits per week. Differences in years in practice approached statistical significance.
Patient-level predictors of use and quality of care
Table 3 depicts the regression model used to examine predictors of differences in depression care between Latinos and whites. Even after the analyses controlled for sociodemographic and clinical differences, Latinos remained less than half as likely as whites to receive any depression care or depression care that met the guideline criteria.
Clinic-level predictors of use and quality of care
As seen in Table 4, neither the percentage of Latinos in the clinics nor the interaction of this variable and Latino ethnicity were associated with differences in receiving any depression care or with the quality of depression care.
Discussion
In a national sample of depressed primary care patients, all of whom had insurance and a regular source of care, rates of any depression care and the quality of depression care were low. However, Latinos were significantly less likely than whites to report receiving any recent depression care (31 percent of Latinos compared with 50 percent of whites) or any depression care that met minimum treatment guideline criteria (19 percent compared with 36 percent). Indeed, even when the analyses controlled for sociodemographic and clinical differences between Latino and white patients, Latinos continued to be less than half as likely as whites to report receiving any depression care or depression care that met guideline criteria. We found that rates of care did not vary according to the ethnic composition of the clinic patient population, despite some differences in clinician characteristics among clinics.
Because treatment differences in our sample were not accounted for by access to care, sociodemographic characteristics, clinical characteristics, or source of care, other patient- and provider-level factors may be driving low rates of depression care among Latinos. Because of the lack of depression treatment experienced by Latinos, they may have less knowledge and different attitudes about depression care. In some Latino primary care samples, patient-level barriers have included lack of recognition of depression as an illness requiring medical care, not knowing where to go for care, and misconceptions about antidepressants (Lagomasino IT, Dwight-Johnson M, Aisenberg E, et al, unpublished data, 2005). Patients with less knowledge about depression are less likely to want active depression treatment (22). Furthermore, low rates of care in Latino communities may result in greater stigma associated with mental health care and few opportunities to find support and encouragement for entering depression treatment (Lagomasino IT, Dwight-Johnson M, Aisenberg E, et al, unpublished data, 2005).
Poor provider-patient communication may also result in lower rates of care among Latinos. Providers may have difficulty recognizing and diagnosing depression among Latinos because of differences in language, culture, or symptom expression. Furthermore, patient participation in care may be diminished by cultural values of respeto (exceptional respect for authority figures) and familismo (heightened importance and centrality of family) (23,24,25), which may prevent patients from being assertive with medical professionals and from making individual treatment decisions without family consultation. Unfortunately, provider discrimination cannot be excluded as a factor in low rates of care among Latinos. However, we did not find that Latino patients in clinics that served mostly Latino clientele had higher rates of depression care, despite the fact that providers in these clinics were more likely to speak Spanish.
Our study findings imply that improving current disparities in depression care will likely require addressing patient- and provider-level barriers in a variety of settings. Interventions may include culturally appropriate patient education and efforts to help affect knowledge, attitudes, and social norms and to empower patients as active participants in their care. Including families in education and decision making may also improve entry into and retention in care. Providers may need further training in diagnosing depression among Latino patients and providing culturally appropriate depression care for them.
Several limitations to this study should be noted. Sample loss during enrollment may have affected results. All measures, including use of depression treatments, were self-reported, although recent work supports the superiority of similar assessments of antidepressant use over studies based on pharmacy data (26). There has also been some concern about Latinos having a higher false-positive rate for depression on the CIDI, which would bias our findings toward less adequate care for Latinos (27). However, the CIDI was designed for use in cross-cultural studies, and in this sample, whites and Latinos did not significantly differ on depressive symptom severity as measured by the Center for Epidemiologic Studies Depression Scale. Our clinic-level variable of percentage of Latinos served in each clinic was meant to be representative of resource differences among clinics, but specific measures of organization and resources were not explicitly used in regression models. However, our analysis of clinic- and provider-level characteristics did not reveal consistent differences among clinics that might affect quality of care. This lack of significant differences among clinics suggests that further subanalyses that used more detailed clinic characteristics would not have been fruitful. A similar variable has been used to examine the impact of community ethnic composition on perceived access to health care, which has shown that Latinos and blacks reported greater access to health care services when residing in counties with more than 40 percent of residents with similar ethnic background (28).
We included sociodemographic and clinical factors in our analyses that are commonly believed to account for health care disparities. These factors were not found to account for differences in care between Latinos and whites in this sample; the precise characteristics that account for the differences were not measured and can only be speculated about. Although we were examining disparities in a managed care sample, it is important to note that low rates of insurance among Latinos in the general population may result in their greater use of resource-poor public-sector systems. These clinics may not be able to deliver the same level of care as managed care clinics, producing even greater disparities in care between Latinos and whites. Our sample was predominantly Mexican American and was moderately to well acculturated; thus findings may not be generalizable to all Latino primary care populations.
Conclusions
Despite these limitations, the results of this study suggest that disparities in depression care between Latinos and whites exist, even among insured patients with a regular source of primary care and even when the analyses controlled for sociodemographic and clinical characteristics. These differences were not attributable to the ethnic composition of clinic clientele. Further research is needed to identify patient and provider factors that may contribute to poor rates of depression care in order to address current disparities.
Acknowledgments
This work was funded by grant R01-HS-08349 from the Agency for Healthcare Research and Quality and grants P30-MH-68639 and P01-MH-59876 from the National Institute of Mental Health.
Dr. Lagomasino is affiliated with the department of psychiatry and behavioral sciences at University of Southern California Keck School of Medicine, 1520 San Pablo Street, Suite 4100, Los Angeles, California 90033 (e-mail, [email protected]). Dr. Dwight-Johnson is with the department of psychiatry and behavioral sciences at the University of Washington in Seattle. Dr. Miranda, Ms. Zhang, Ms. Liao, Dr. Duan, and Dr. Wells are with the Health Services Research Center at the University of California, Los Angeles. Dr. Wells is also with RAND in Santa Monica.
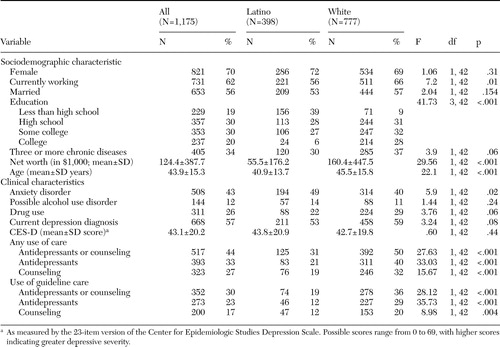 |
Table 1. Sociodemographic and clinical characteristics and use of depression care among Latino and white patients in managed care settings
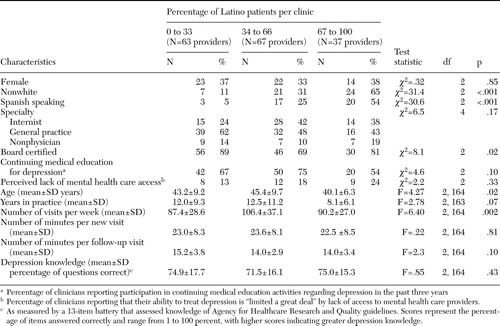 |
Table 2. Clinic and provider characteristics for primary care clinics with low, moderate, and high proportions of Latino patients
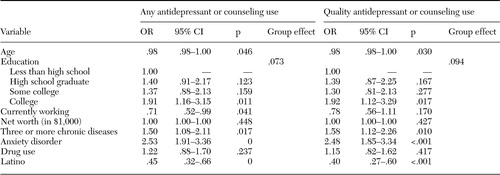 |
Table 3. Logistic regression analysis of predictors of use of depression care by socioeconomic and clinical characteristic differences among Latino and white patients in managed care settings
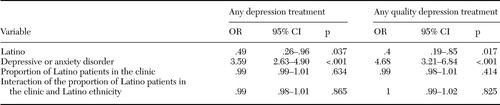 |
Table 4. Logistic regression analysis of predictors of depression care by proportion of Latino patients served by clinics
1. Mental Health: Culture, Race, and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville, Md, Center for Mental Health Services, 2001Google Scholar
2. Hough RL, Landsverk JA, Karno M, et al: Utilization of health and mental health services by Los Angeles Mexican Americans and non-Hispanic whites. Archives of General Psychiatry 44:702–709,1987Crossref, Medline, Google Scholar
3. Vega WA, Kolody B, Aguilar-Gaxiola S, et al: Gaps in service utilization by Mexican Americans with mental health problems. American Journal of Psychiatry 156:928–934,1999Link, Google Scholar
4. Health Insurance Coverage and Access to Care Among Latinos: Key Facts Report. Washington, DC, Henry J Kaiser Family Foundation, 2000Google Scholar
5. Sclar DA, Robison LM, Skaer TL, et al: Ethnicity and the prescribing of antidepressant pharmacotherapy:1992–1995. Harvard Review of Psychiatry 7:23–36,1999Google Scholar
6. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55–61,2001Crossref, Medline, Google Scholar
7. Brown PA: Differential utilization of the health care delivery system by members of ethnic minorities. Journal of Sociology and Social Welfare 3:516–523,1976Google Scholar
8. Greenblatt M, Norman M: Hispanic mental health and use of mental health services: a critical review of the literature. American Journal of Social Psychiatry 2:25–31,1982Google Scholar
9. Woodward AM, Dwinell AD, Arons BS: Barriers to mental health care for Hispanic Americans: a literature review and discussion. Journal of Mental Health Administration 19:224–236,1992Crossref, Medline, Google Scholar
10. Rogler LH: Culturally sensitizing psychiatric diagnosis: a framework for research. Journal of Nervous and Mental Disease 181:401–408,1993Crossref, Medline, Google Scholar
11. Ruiz P: Access to health care for uninsured Hispanics: policy recommendations. Hospital and Community Psychiatry 44:958–962,1993Abstract, Google Scholar
12. Snowden LR: Ethnic minority populations and mental health outcomes. New Directions for Mental Health Services 71:79–87,1996Crossref, Medline, Google Scholar
13. Wells KB: The design of Partners in Care: evaluating the cost-effectiveness of improving care for depression in primary care. Social Psychiatry and Psychiatric Epidemiology 34:20–29,1999Crossref, Medline, Google Scholar
14. Wells KB, Sherbourne C, Schoenbaum M, et al: Impact of disseminating quality improvement programs for depression in managed primary care. JAMA 283:212–220,2000Crossref, Medline, Google Scholar
15. Composite International Diagnostic Interview (CIDI), Version 2.1. Geneva, Switzerland, World Health Organization, 1995Google Scholar
16. Depression in Primary Care: Vol 1: Detection and Diagnosis. AHCPR pub no 93–0550. Rockville, Md, US Department of Health and Human Services, Agency for Health Care Policy and Research, Depression Guidelines Panel, 1993Google Scholar
17. Depression in Primary Care: Vol 2: Treatment of Major Depression. AHCPR pub no 93–0551. Rockville, Md, US Department of Health and Human Services, Agency for Health Care Policy and Research, Depression Guidelines Panel, 1993Google Scholar
18. Smith JP: Racial and ethnic differences in wealth in the Health and Retirement Study. Journal of Human Resources 30 (suppl):S158-S183, 1995Google Scholar
19. Burnam MA, Hough RL, Karno M, et al: Acculturation and lifetime prevalence of psychiatric disorders among Mexican Americans in Los Angeles. Journal of Health and Social Behavior 28:89–102,1987Crossref, Medline, Google Scholar
20. Radloff LS: The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement 1:385–401,1977Crossref, Google Scholar
21. Bohn MJ, Babor TF, Kranzler HR: The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol 56:423–432,1995Crossref, Medline, Google Scholar
22. Dwight-Johnson M, Sherbourne CD, Liao D, et al: Treatment preferences among depressed primary care patients. Journal of General Internal Medicine 15:527–534,2000Crossref, Medline, Google Scholar
23. Latino Health Beliefs: A Guide for Health Care Professionals. Washington, DC, National Council of la Raza, 1998Google Scholar
24. Flaskerud JH, Kim S: Health problems of Asian and Latino immigrants. Nursing Clinics of North America 34:359–380,1999Medline, Google Scholar
25. Resnicow K, Baranowski T, Ahluwalia JS, et al: Cultural sensitivity in public health: defined and demystified. Ethnicity and Disease 9:10–21,1999Medline, Google Scholar
26. Kwon A, Bungay KM, Pei Y, et al: Antidepressant use: concordance between self-report and claims records. Medical Care 41:368–374,2000Google Scholar
27. Minsky S, Vega W, Miskimen T, et al: Diagnostic patterns in Latino, African American, and European American psychiatric patients. Archives of General Psychiatry 60:637–644,2003Crossref, Medline, Google Scholar
28. Haas JS, Phillips KA, Sonneborn D, et al: Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual's county of residence. Medical Care 42:707–714,2004Crossref, Medline, Google Scholar



