Demand for Mental Health Care and Changes in Service Use Patterns in the Netherlands, 1979 to 1995
Abstract
OBJECTIVE: Mental health services appear increasingly incapable of satisfying the demand for care, which may cause some segments of the population to be less effectively reached. This study investigated the rates of use of mental health services in the Netherlands from 1979 to 1995 and examined whether particular sociodemographic groups made greater or lesser relative use of these services over time. METHODS: Data were derived from the Facilities Use Surveys, a series of Dutch cross-sectional population studies that have recorded household characteristics and service use since 1979. More than 28,000 households were included in the analyses. RESULTS: The overall use of mental health services virtually doubled from 1979 to 1995; a particularly steep rise was seen in the first half of the 1980s. Households that had one parent, that had low income, that were dependent on benefits, and that were younger all had greater odds of using both specialized mental health care (for example, prevention programs for mental health problems and psychotherapeutic and social psychiatric treatment offered by psychologists, psychotherapists, or psychiatrists) and social work services (for example, psychosocial counselling and practical support offered by social workers to people with social problems, such as housing, finances, and psychosocial issues). Households with low education were less likely to use specialized mental health care but were more likely to use social work services. Nonreligious households and urban households were more likely to use specialized mental health care and were equally likely to use social work services. Overall, these relative use patterns did not change over time. CONCLUSIONS: Despite greater pressures on mental health services and the many changes in service delivery in recent decades, relative patterns of help seeking and referral to mental health services have not varied systematically over time.
The demand for mental health care is rising in many places throughout the world (1). Reasons for this trend include increased recognition of mental disorders by the general public and by primary care providers, the development of effective treatments for common mental disorders, declines in social support and other coping resources in the community, and possibly a rising overall prevalence of major depression (2,3,4). Given the limited resources available, a growing demand for services may lead to shifts in which segments of the population are being reached. Knowledge about long-term trends in service use patterns can help to identify any such shifts and plan an adequate allocation of scarce resources.
Data on this topic are still very sketchy. Kulka and colleagues (5) found that education and income differences in the use of specialized mental health care in 1957 generally persisted in 1976, although the difference between income groups seemed to narrow. Olfson and colleagues (4) found no variations between demographic groups in their rates of outpatient mental health treatment from 1987 to 1997. However, the Olfson group (6) found significant increases in psychotherapy use in that period by adults aged 55 to 64 years and by unemployed adults. Weisner and colleagues (7) found that men, especially younger ones aged 18 to 29 years, made increasing use of alcohol-related treatment from 1979 to 1990, but they concluded that the overall treatment patterns of specific groups changed little.
To our knowledge, few countries exist in which reliable longer-term data on service use by the general public have been charted by using consistent research designs and instruments. In the Netherlands such data are available from the Facilities Use Surveys (FUS) of the Social and Cultural Planning Office, a series of cross-sectional population studies conducted periodically since 1979 that are representative of the general population. This article is based on that data.
This study addresses two research questions: Did an increase occur in the use of mental health services in the Netherlands from 1979 to 1995? Did particular sociodemographic groups make greater or less relative use of these services over time? We addressed these questions separately for two important types of mental health care provision—specialized mental health care (represented here by services provided by regional institutes for ambulatory mental health care—for example, prevention programs for mental health problems and psychotherapeutic and social psychiatric treatment; programs and treatment offered by psychologists, psychotherapists, or psychiatrists) (8) and social work services (for example, psychosocial counselling and practical support offered by social workers to people with social problems, such as housing, finances, and psychosocial issues). Dividing mental health care in this way enabled us to examine whether trends and variations in use patterns varied according to the sector in which help was sought.
Social work services, as well as services provided by general practitioners, are major sources of primary mental health care in the Netherlands. Clients may contact them directly. Regional ambulatory mental health care institutes are major sources of secondary care. Clients may contact them only after referral by a general practitioner. Both types of services are publicly funded, and virtually no financial barriers exist to obtaining access to either type of care (9).
Methods
Sample
The FUS periodically investigate the use of social, cultural, and health facilities in the Netherlands. The surveys are based on nationwide household samples and contain information on all household members. FUS have been conducted every four years since 1979. The data analyzed in our study included all household members aged 16 to 74 years covered by the five FUS conducted between 1979 and 1995 (10). All FUS had comparable research designs. About 6,000 households were interviewed each time, with responses just over 40 percent in 1991; around 60 percent in 1979, 1983, and 1987; and 70 percent in 1995. The samples were representative of households of the noninstitutionalized population in terms of household composition (gender, age, and marital status) and urbanicity of residence. In 1987 one-person households and families with grown children were slightly underrepresented (11). Despite the varying response rates between surveys, these variations showed no association with any of the trends found in service use or help seeking. It therefore seems unlikely that nonresponse compromised our results.
All the FUS applied a relatively straightforward, random sampling procedure. A sample of private households (addresses) was drawn from postal registers in proportion to the population of each municipality included. The households were sent a letter of introduction with an explanatory leaflet. Shortly afterwards, they were contacted by the interviewers. If necessary, interviewers made several calls or visits to a given address at different times to make contact. If they succeeded, they interviewed one member of each participating household at home, generally the head of household. They also left behind extensive questionnaires for each household member aged six or older, returning to collect these later. At addresses with multiple households (which were rare), up to three families were interviewed. Respondents received no remuneration. Informed consent was obtained under prevailing Dutch regulations, and review board approval was secured from the Central Commission for Statistics (12).
Measures
Mental health service use. Service use was determined by the question "In the past 24 months, have you been to any of the following organizations for problems of your own or of any of your household members?" The list included organizations that provided specialized mental health and social work services. The question was posed to all household members aged 16 years and older. We dichotomized answers into 0, no use, and 1, use by at least one member. Service use was assessed at the household level, because it was not known within households who had mental health problems and who received help for them.
Household characteristics. Household composition was divided into five categories: two partners living with children, two partners living without children, one person without a partner living with children, one person living alone, and other.
Household income refers to the net income of the primary breadwinner and partner (if any), excluding child allowance (that is, regular payment by the state to the parents of a child up to a certain age) and income from working children. We recoded household income into four ordinal categories, low to high (categories were created by placing 25 percent of the households in each income group). Missing answers were relatively frequent (21 percent). To avoid a serious reduction of the effective sample size, we treated these missing data as a separate category in the analyses.
Social position of primary breadwinner and partner (if any) was broken down into seven household categories on the basis of principal daily activities: employed, student, retired, dependent on benefits, housewife or househusband, employed breadwinner with a partner who was a housewife or househusband, and other.
Education of primary breadwinner and partner (if any) refers to the highest educational attainment. Categories ranged from primary school to higher professional or university education. Couples whose education levels differed by more than 1 point on this 4-point scale were defined as heterogamous couples (37 percent).
Religious identification of primary breadwinner and partner (if any) was determined by the question "What church or what religious group do you mainly feel part of?" and was dichotomized in terms of identifying with (1) or not identifying with (0) a religious group. Couples who differed were classified as heterogamous (9 percent).
Other characteristics included the mean age of primary breadwinner and partner (if any) and the urbanicity of household location. Urbanicity ranged from rural, score of 1, to highly urbanized, score of 5.
Statistical analysis
After deleting cases with missing values on relevant items, we performed separate analyses for the two types of services—specialized mental health care and social work services—comparing the households that used the type of service with those that did not.
The aim of our study was to show a trend of service use from 1979 to 1995. For this analysis, we used as the reference category the (weighted) average service use of all households over the entire period. The analyses for mental health care used data for 28,264 households, and the analyses for social work services used data for 28,274 households. This approach, which is commonly used in demographic research (13), is unusual in the study of service use. Therefore, a more detailed description of our methods will be given.
First, we constructed contingency tables to calculate the percentage of households that used the two types of services in each of the five years that the survey was given. We then calculated whether these percentages differed from the overall mean percentages of all households that used the services over the entire study period. These analyses addressed whether service use increased over time. A trial use of weighting in the calculations did not result in a different conclusion.
Second, we pooled the data and performed seven stepwise multiple logistic regression analyses for both types of service use. For each of the seven household characteristics (for example, household composition) we explored whether its particular household categories (for example, two partners living with children) made greater or less relative use of these services over time. In addressing this question, we used interaction terms in our stepwise multiple logistic regression analyses (in particular, a household characteristic with its particular household categories multiplied the study years). In the first step of our multiple logistic regression analyses we entered two variables: a certain household characteristic and the study year. In the second step we entered interaction terms between these two variables by using forward selection: the particular household categories multiplied by the study years. As the reference category we used the weighted average service use of all household categories over the entire study period (14).
For each of the seven household characteristics we performed two multiple logistic regression analyses. In each analysis for a particular household characteristic—for example, household composition—we explored the presence of interaction effects (that is whether the odds of using a service varied for the particular household categories over time) and reported only the significant interaction effects.
If there was no significant interaction term between one of the particular household categories and a study year, we presented the odds ratios for each of the household categories while controlling for the effect of study year.
If there was a significant interaction term between a household category and study year, we calculated the particular odds ratio for that household category in that particular year. We present this odds ratio as well as the one in the other years for the particular household categories. In this way it becomes clear to what extent the odds of making use of the services can fluctuate over time for household categories compared with the average household.
Finally, we performed one stepwise multiple logistic regression analysis for both types of service use, using the method described above. We adjusted not only for the study year but also for other household characteristics. In the first step of our multiple logistic regression analysis we entered all household characteristics and study year simultaneously. In the second step we entered interaction terms between these variables by using forward selection: all household categories by study years. As a reference category we again used the weighted average service use of all household categories over the entire study period. Results of these analyses were not tabulated here, because they did not differ substantially from those presented.
All statistical analyses were performed with SPSS version 12.0 for Windows.
No results were weighted, as we were seeking to explain, rather than describe, the interrelationships between determinants and service use. The necessity of adjusting for sampling characteristics in analytic studies is the subject of ongoing debate. Most of the time overall conclusions do not substantially change when sample weights are used (15,16).
Results
Trends in the use of mental health services
Figure 1 shows the general increases in the use of specialized mental health care and social work services over time. In 1979 household use of specialized mental health was 3.4 percent for all households; this percentage rose to 5.7 percent by 1995. The trend was significant from 1979 to 1983 in particular (two-tailed testing procedures with .05 alpha levels). The use of social work services more than doubled until the mid-1980s, from 2.0 percent in 1979 to 5.5 percent in 1987, but subsequently remained stable around 5.6 percent.
Household characteristics and use of mental health services
Table 1 shows the correlates of each household characteristic with service use, after adjustment for study year and any interactions between that household characteristic and the study year. The numbers indicate that households that had one parent, that had the lowest income, and that were dependent on benefits were more likely than the average household to have used some type of mental health service in the study period. For example, households with one parent were approximately three times as likely as the average household to use specialized mental health care and social work services. Couples not living with children, households in which one member of a couple worked and the other kept house, and older households were less likely than the average household to use either type of care.
Education had contrasting effects on specialized care and social work services. Households whose primary breadwinner and partner (if any) had primary school education only were less likely to use specialized care but were more likely to use social work services, compared with the average household. Households identified as nonreligious and households in highly urbanized areas were more likely than average to use specialized care but were equally likely to use social work services.
Change in use of mental health services
Some household categories showed significant fluctuations in their likelihood of service use, as seen in the interactions of some household characteristics with particular study years. However, none of these variations reflected consistent shifts over time. For example, in 1991 households in the third income category were less likely than the average household to use specialized mental health care, but they were equally likely to use it in other years. In 1987 and 1991 the effect of benefit dependence was significantly weaker than in other years. That is, compared with average households, benefit-dependent households had 1.56 times greater odds of using specialized care in 1987 and 1.47 greater odds in 1991; however, these households had an odds ratio of 2.58 for all other survey years. Households headed by students were another category that was less likely to use specialized care in 1987 than in other years. Employed households and households in which one member of a couple worked and the other kept house had elevated use of specialized care in a single study year. Other fluctuations in the relative service use of particular household categories were seen for social work services, but only for 1983 (Table 1).
These results seem to indicate that no major overall shifts occurred in the relative service use of particular sociodemographic groups, or in the existing inequalities between them, during the 17 years examined here.
Discussion
Data on trends and patterns of the use of mental health services are of vital importance for both public health and for the adequate allocation of mental health resources. Few representative data are available that enable a long-term analysis of trends. We made use of large-scale surveys that have been conducted in the Netherlands every four years since 1979 and that are representative of the population at large.
Increased pressure on mental health services
The overall use of mental health services by Dutch households virtually doubled from 1979 to 1995, with a particularly steep rise in the first half of the 1980s. In absolute terms, service use grew even more sharply, by virtue of a 32 percent increase in the total number of households in that period (from 4,911,000 to 6,469,000). Client registry data confirm the increasing pressure on both primary and secondary mental health provisions (17). In the first half of the 1980s a major change in the provision of specialized mental health care took place: within each region different institutes for ambulatory mental health care merged to create one regional institute for ambulatory mental health care, which offered various types of ambulatory care. This change made mental health care more available and accessible.
Relative changes in households using services
Greater pressures on mental health services and changes in their delivery—including stepped-care strategies in primary care, more efficient procedures for diagnosing mental disorders, and a greater use of medications (1) and behavior therapies in specialized care—did not alter the relative pattern of help seeking or referral to mental health services. Any year-to-year variations in the relative service use by particular household categories during the 17 years studied were neither substantial nor sustained. Such fluctuations might even be chance outcomes of the many tests we carried out. Our conclusion that all households equally took advantage of the increased availability of specialized mental health care services concurs with several previous international studies (4,5,7).
Reasons for use of mental health services
Households that had one parent, that had low income, and that were dependent on benefits all had greater odds of using specialized mental health care and social work services during the study period. This finding seems consistent with several previous individual-level studies that investigated the effects of single motherhood, social support, or income sources on the use of primary care or mental health care (18,19,20,21,22,23). Households in these categories may have more emotional disorders than the average household, less access to various types of support, or less capability of solving problems or avoiding economic distress. Mental health care may then serve as a partial substitute for social or personal resources.
Households whose primary breadwinner and partner (if any) had completed no more than primary school were less likely than the average household to use specialized mental health care but were more likely to use social work services. Badawi and colleagues (24) analyzed service use by household type and found, as we did, that the lower the education level, the less likelihood of using mental health services; their analysis adjusted for mental disorder, other individual characteristics, and household type (25). Two other studies suggest that less educated people have a lower propensity to seek specialized mental health care (26,27). It would thus appear that people's attitudes toward using care as a means of solving problems is one additional factor that could explain differences in service use.
Older households were less likely than the average household to have used either type of service, which could be interpreted as an age or a cohort effect (28,29,30). Although such effects cannot be assessed with our data (31), this finding is in line with those of previous studies. Badawi and colleagues (24) found less service use by people aged 65 years or older and higher service use by those aged 30 to 44 years, after adjustment for mental disorder, other individual characteristics, and household type.
Strengths and limitations
We believe that a major strength of this study is its long-term perspective. Large samples of households, representative of the population, were surveyed by using comparable methods. Some potential limitations may also be noted. First, there was considerable nonresponse in all surveys, although the samples still remained representative of the population at the household level. Response rates varied between surveys, but they showed no association with any of the trends found in service use or help seeking. It therefore seems unlikely that nonresponse compromised our results.
Second, recall problems could have affected household members' estimations of service use in the previous two years, although it is difficult to gauge what effect that might have had on our results. Conceivably, people might have underreported service use for mild mental problems, in which case the trends we identify would underestimate the situation.
Third, no data were available on the use of Dutch mental health services other than from the regional institutes for ambulatory mental health care and social work agencies, such as psychiatric clinics, private practices, and general practitioners. However, because these regional institutes and social agencies are major sources of secondary and primary mental health care, we believe that our results are generalizable to other such services.
Conclusions
Notwithstanding these potential limitations, we conclude that although mental health service use increased sharply during the 17-year period, no relative changes occurred in the help-seeking patterns among the sociodemographic groups examined. Service output statistics also indicate higher workloads for professionals (17). The number of client contacts per staff position (expressed in full-time equivalents) increased by 17 percent in specialized mental health from 1983 to 1995 and by 16 percent in social work services from 1987 to 1995. Thus, although care services became more heavily burdened, referral patterns and intake criteria remained relatively unchanged. Apparently, considerations related to substantive care weighed more heavily in the provision and use of services than professional workloads, which seems to indicate stable patterns of help seeking and referral to mental health services.
Acknowledgments
This research was funded by the Netherlands Mental Health Fund [Nationaal Fonds Geestelijke Volksgezondheid, NFGv].
Dr. ten Have, Dr. Beekman, and Dr. Vollebergh are affiliated with the monitoring and epidemiology department of the Netherlands Institute of Mental Health and Addiction, P.O. Box 725, Utrecht, 3500 AS, the Netherlands (e-mail, [email protected]). Dr. Beekman is also with the department of psychiatry at Vrije Universiteit Amsterdam in the Netherlands. Dr. Meertens is with the department of sociology and Dr. Scheepers and Dr. te Grotenhuis are with the department of social science research methods at the University of Nijmegen in the Netherlands.
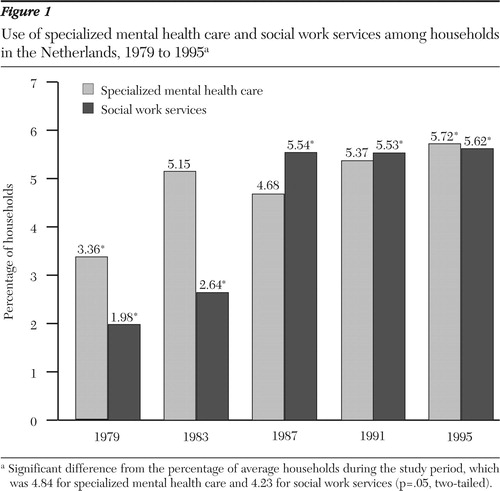
Figure 1. Use of specialized mental health care and social work services among households in the Netherlands, 1979 to 1995a
aSignificant difference from the percentage of average households during the study period, which was 4.84 for specialized mental health care and 4.23 for social work services (p=.05, two-tailed).
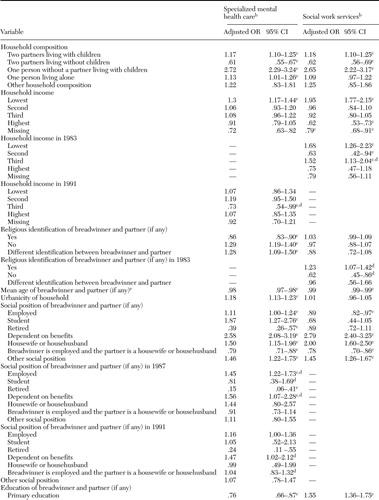 |
Table 1. Multiple logistic regression analyses of determinants of the use of specialized mental health care and social work services in households in the Netherlands, 1979 to 1995a
aThe analyses for mental health care used data for 28,264 households, and the analyses for social work services used data for 28,274 households. The effects of each household characteristic are adjusted for the influence of study year and, if applicable, the interaction between the household characteristic and study year. The reference group is the weighted average household of the pooled data set. To compute the deviation of a particular household category from the average household in the use of specialized mental health care or social work services (and thereby the odds ratio), the method devised by Sweeney and Ulveling (12) was used. Data for individual study years are shown only if significant differences were found between the average of all study years and the particular study year (that is, if one or more interaction terms were present).
1. Tanielian TL, Marcus SC, Suarez AP, et al: Trends in psychiatric practice, 1988–1998: II. Caseload and treatment characteristics. Psychiatric Services 52:880,2001Link, Google Scholar
2. Meredith WG, Klerman GL, Lavori PW: Are secular trends in major depression an artifact of recall? Journal of Psychiatric Research 25:141–151,1991Google Scholar
3. Oldehinkel AJ: Time trends in mental health care utilization in a Dutch area, 1976–1990. Social Psychiatry and Psychiatric Epidemiology 33:181–185,1998Crossref, Medline, Google Scholar
4. Olfson M, Marcus SC, Druss B, et al: National trends in the outpatient treatment of depression. JAMA 287:203–209,2002Crossref, Medline, Google Scholar
5. Kulka RA, Veroff J, Douvan E: Social class and the use of professional help for personal problems:1957 and 1976. Journal of Health and Social Behavior 20:2–17,1979Google Scholar
6. Olfson M, Marcus SC, Druss B, et al: National trends in the use of outpatient psychotherapy. American Journal of Psychiatry 159:1914–1920,2002Link, Google Scholar
7. Weisner C, Greenfield T, Room R: Trends in the treatment of alcohol problems in the US general population, 1979 through 1990. American Journal of Public Health 85:55–60,1995Crossref, Medline, Google Scholar
8. Schene AH, Faber AME: Mental health care reform in the Netherlands. Acta Psychiatrica Scandinavica 104(suppl 410):74–81,2001Google Scholar
9. Alegria M, Bijl RV, Lin E, et al.: Income differences in persons seeking outpatient treatment for mental disorders: a comparison of the United States with Ontario and the Netherlands. Archives of General Psychiatry 57:383–391,2000Crossref, Medline, Google Scholar
10. Have M ten, Grotenhuis M te, Meertens V, et al: Upward trends in the use of community mental health and social work services in the Netherlands between 1979 and 1995: are particular sociodemographic groups responsible? Acta Psychiatrica Scandinavica 108:447–454,2003Google Scholar
11. Social and Cultural Planning Office of the Netherlands. Aanvullend Voorzieningengebruik Onderzoek (AVO) [Facilities Use Surveys (FUS)]. Available at www.scp.nl/onderzoek/avo99/default.htm (information in Dutch)Google Scholar
12. Data Services. Social and Cultural Planning Office of the Netherlands. Available at www.scp.nl/english/resources/data-services/index.htmlGoogle Scholar
13. Grotenhuis M te, Scheepers P, Eisinga R: The method of purging applied to repeated cross-sectional data: practical applications using logistic and linear regression analysis. Quality and Quantity 38:1–16,2004.Crossref, Google Scholar
14. Sweeney RE, Ulveling EF: A transformation for simplifying the interpretation of coefficients of binary variables in regression analysis. American Statistician 26:30–32,1972Google Scholar
15. Ingram DD, Makuc DM: Statistical issues in analyzing the NHANES I Epidemiologic Followup Study. Series 2: Data evaluation and methods research. Vital Health Statistics 121:1–30,1994Google Scholar
16. Korn EL, Graubard BI: Epidemiologic studies utilizing surveys: accounting for the sampling design. American Journal of Public Health 81:1166–1173,1991.Crossref, Medline, Google Scholar
17. Statline. Statistics Netherlands. Available at http://statline.cbs.nl/statweb/start.asp?la=en&dm=slen&lp=search%2fsearchGoogle Scholar
18. Bebbington PE, Meltzer H, Brugha TS, et al: Unequal access and unmet need: neurotic disorders and the use of primary care services. Psychological Medicine 30:1359–1367,2000Crossref, Medline, Google Scholar
19. Bijl RV, Ravelli A: Psychiatric morbidity, service use, and need for care in the general population: results of the Netherlands Mental Health Survey and Incidence Study. American Journal of Public Health 90:602–607,2000Crossref, Medline, Google Scholar
20. Cairney J, Wade TJ: Single parent mothers and mental health care service use. Social Psychiatry and Psychiatric Epidemiology 37:236–242,2002Crossref, Medline, Google Scholar
21. Ten HM, Vollebergh W, Bijl R, et al: Combined effect of mental disorder and low social resources on care service use for mental health problems in the Dutch general population. Psychological Medicine 32:311–323,2002Crossref, Medline, Google Scholar
22. Lin E, Goering P, Offord DR, et al: The use of mental health services in Ontario: epidemiologic findings. Canadian Journal of Psychiatry 41:572–577,1996Crossref, Medline, Google Scholar
23. Sherbourne CD: The role of social support and life stress in use of mental health services. Social Science and Medicine 27:1393–1400,1988Crossref, Medline, Google Scholar
24. Badawi M, Kramer M, Eaton W: Use of mental health services by households in the United States. Psychiatric Services 47:376–380,1996Link, Google Scholar
25. Have M ten, Oldehinkel A, Vollebergh W, et al: Does educational background explain inequalities in care service use for mental health problems in the Dutch general population? Acta Psychiatrica Scandinavica 107:178–187,2003Google Scholar
26. Leaf PJ, Livingston Bruce M, Tischler GL, et al: The relationship between demographic factors and attitudes toward mental health services. Journal of Community Psychology 15:275–284,1987Crossref, Medline, Google Scholar
27. Tijhuis MAR, Peters L, Foets M: An orientation toward help-seeking for emotional problems. Social Science and Medicine 31:989–995,1990Crossref, Medline, Google Scholar
28. Rodgers WL: Estimable functions of age, period, and cohort effects. American Sociological Review 47:793–796,1982Crossref, Google Scholar
29. Inglehart R: Culture Shift in Advanced Industrial Society. New Jersey, Princeton, 1990Google Scholar
30. Das Problem der Generationen [The problem of generations], in Mannheim K: Wissenssoziologie [Sociology of Science]. Berlin-Neuwied, Luchterhand, 1964Google Scholar
31. Menard S: Longitudinal research. Newbury Park, Calif, Sage, 1991Google Scholar



