Twelve-Month Outcomes of Trauma-Informed Interventions for Women With Co-occurring Disorders
Abstract
OBJECTIVE: Women with co-occurring mental health and substance use disorders frequently have a history of interpersonal violence, and past research has suggested that they are not served effectively by the current service system. The goal of the Women, Co-occurring Disorders, and Violence Study was to develop and test the effectiveness of new service approaches specifically designed for these women. METHODS: A quasi-experimental treatment outcome study was conducted from 2001 to 2003 at nine sites. Although intervention specifics such as treatment length and modality varied across sites, each site used a comprehensive, integrated, trauma-informed, and consumer-involved approach to treatment. Substance use problem severity, mental health symptoms, and trauma symptoms were measured at baseline, and follow-up data were analyzed with prospective meta-analysis and hierarchical linear modeling. RESULTS: A total of 2,026 women had data at the 12-month follow-up: 1,018 in the intervention group and 1,008 in the usual-care group. For substance use outcomes, no effect was found. The meta-analysis demonstrated small but statistically significant overall improvement in women's trauma and mental health symptoms in the intervention relative to the usual-care comparison condition. Analysis of key program elements demonstrated that integrating substance abuse, mental health, and trauma-related issues into counseling yielded greater improvement, whereas the delivery of numerous core services yielded less improvement relative to the comparison group. A few person-level characteristics were associated with increases or decreases in the intervention effect. These neither moderated nor supplanted the effects of integrated counseling. CONCLUSIONS: Outcomes for women with co-occurring disorders and a history of violence and trauma may improve with integrated treatment.
Research has demonstrated that high rates of traumatic childhood experiences are risk factors for adult psychological symptoms and problematic behaviors (1,2,3,4,5). Childhood experiences such as physical and sexual abuse, witnessing violence, and neglect—often in combination with adult trauma—have led some women into lives dominated by prolonged periods of co-occurring mental disorders and substance use disorders (6,7,8).
Historically, most treatment settings, regardless of whether they deal with mental health, substance abuse, primary care, or other issues, have not routinely assessed women for trauma or posttraumatic stress disorder (PTSD), leading to underrecognition and undertreatment of these important issues (9,10,11). Although some programs and systems have begun to address these issues, many still do not. Moreover, women with substance use problems have typically received the message that they need to be clean and sober for some period before trauma or PTSD can be addressed (12,13).
The Women, Co-occurring Disorders, and Violence Study (WCDVS) represents the first major federal effort to address the lack of appropriate services for women with co-occurring mental health and substance use disorders who also have a history of physical or sexual abuse. The primary goals of the WCDVS were to develop new service approaches and to evaluate their effectiveness for women with these problems, who have been frequent, or high-end, users of services (14,15). The intervention included eight core services, such as resource coordination and crisis intervention; staff knowledgeable about trauma; holistic treatment of mental health, trauma, and substance use issues; and the involvement of consumers in service planning and provision.
The WCDVS involved a quasi-experimental study of nine sites. Participants were interviewed and dependent variables were measured at baseline and two follow-up points. Previously, we reported the six-month outcomes (16,17) that showed small improvements in mental health symptoms, trauma symptoms, and drug use severity. These effects increased substantially when measured in sites where integrated counseling—the integration of trauma, substance abuse, and mental health issues across or within individual or group counseling—was greater in the intervention than in the comparison condition.
This issue of Psychiatric Services discusses the overall design features of the study (18) and gives the cost evaluations of this program at 12 months (19). In this article we focus on results at the final, 12-month follow-up to determine whether positive effects at six months were maintained at 12 months. Four research questions were addressed for each of the four outcomes—mental health symptoms, trauma symptoms, drug use severity, and alcohol use severity. First, are there any intervention effects at 12 months, and do these effects vary by key characteristics of the participating programs? Second, if there are significant intervention effects at 12 months, do they interact with or are they explained by person-level variables? Third, if there are significant effects related to program characteristics, do they interact with or are they explained by person-level variables? Finally, are the results clinically meaningful?
Methods
The WCDVS was conducted from 2001 to 2003 at nine intervention sites located in California (two sites), Colorado, Florida, Massachusetts (three sites), New York City, and Washington, D.C. In keeping with the quasi-experimental design (20), the intervention sites chose comparison agencies that served similar clients with care-as-usual services in the same or nearby communities. Eligible study participants were recruited independently at each location from a pool of women who had recently been referred for services. More detailed descriptions of the WCDVS research design (20), the prospective meta-analysis technique used to identify program-level effects (16), and the hierarchical linear modeling (HLM) process used to select covariates and to assess person-level effects are available elsewhere (17).
Sample
Among the 2,729 participants who completed baseline interviews, 2,087 (76 percent) also completed an interview approximately 12 months after baseline. Women were retained in the analysis if their interview date occurred within 12 weeks before or after the 12-month target date. This 24-week window was chosen to maximize the number of women retained in the analysis, while minimizing symptom outcome variability that might result from their being interviewed at very different points in their posttreatment recovery. As a consequence, 61 women (2.9 percent) were excluded, leaving 2,026 women in the analysis sample. Among these, 1,769 were included in the six-month sample of 2,006 women reported elsewhere (15,16,1720); the remaining 237 either were not interviewed at six months or were excluded because the interview did not occur within 12 weeks of the target date. (In a sensitivity check, the outcome analyses reported below were rerun with these 61 women included in the analysis sample with no change in the overall findings reported in this article.)
Data collection procedures and subject protections were approved by institutional review boards at each site and at each of three units that formed the coordinating center. All participants provided written informed consent to participate in the research.
Interventions
To be consistent with the overall WCDVS goals, all intervention sites were required to provide services meeting four criteria. First, they had to provide a comprehensive array of services that included outreach, assessment, crisis intervention, trauma-specific counseling, ongoing treatment, parent-skills training, resource coordination and advocacy, and peer-run services. Trauma-specific service interventions (cited below) addressed the behavioral, emotional, cognitive, and interpersonal consequences of exposure to sexual, physical, and prolonged emotional abuse. Second, staff providing these services were trauma informed—that is, they were sensitive to the trauma that these women had experienced. Third, counseling and other services integrated treatment for mental health, substance abuse, and trauma-related problems. And fourth, sites involved consumers (women with a similar history) in advisory and service provision roles.
Despite having common intervention elements, trauma-specific treatment implementation varied by site. One site used the Addiction and Trauma Recovery Integration Model (ATRIUM) (21); four used the Seeking Safety Model (22); three used the Trauma Recovery and Empowerment Model (TREM) (23); and one developed a hybrid model called Triad (24). All these interventions were guided by manuals. The interventions focused on maintaining personal safety, teaching empowerment and coping skills, and helping women understand the links between substance abuse, mental health problems, and trauma. Depending on the site, the trauma-specific intervention took place for one to two hours in residential or outpatient settings or both, and the duration varied from 12 to 33 group sessions, which were held once or twice per week.
The comparison condition represented care as usual in each site's region. Comparison services varied from site to site and sometimes included some of the same program elements offered by the intervention. However, none of these usual-care agencies provided trauma-specific treatment (20).
Outcome measures
The four dependent variables were measured in interviews with participants at baseline, six months, and 12 months. Problem severity of drug and alcohol use was assessed with the Addiction Severity Index (ASI) (25). The drug composite score (ASI-D) and the alcohol composite score (ASI-A) measure problem severity during the past 30 days. Possible scores range from 0 to 1, with higher scores indicating greater problem severity of substance use. The ASI-A score was modified slightly in consultation with the author of the ASI, but it was scored on the original scale (20). At baseline mean±SD scores were .16±.15 on the ASI-D and .20±.30 on the ASI-A, indicating a moderate level of severity.
Mental health symptoms were assessed with the Global Severity Index (GSI) of the Brief Symptom Inventory (26). The Brief Symptom Inventory is a 53-item self-report scale that measures nine symptom dimensions. Respondents are asked how much a problem has distressed them in the past seven days. Possible responses range from 0, not at all, to 4, extremely. The GSI is a mean severity measure. Possible scores range from 0 to 4, with higher scores indicating more severe symptoms. At baseline, the mean raw score was 1.34±.77, indicating a moderately elevated level of symptom severity. (Corresponding T scores range from 59 to 75, with a T score of 69 representing the mean raw score.)
Trauma symptoms were assessed with the Posttraumatic Symptom Scale (PSS) of the Posttraumatic Diagnostic Scale (27). The 17-item PSS was developed to assess the severity of trauma symptoms. Respondents were asked to indicate how often in the past month they have experienced a list of problems after a traumatic event. Possible responses range from 0, not at all or only once, to 3, five or more times or almost always. Possible scores range from 0 to 51, with higher scores indicating more severe trauma symptoms. At baseline, the mean score was 23.5±11.7, indicating a moderate-to-severe level of symptom severity. The baseline correlation between the PSS and the GSI was .76.
Analyses
An intent-to-treat approach was followed throughout the analyses—that is, study participants were categorized according to the condition in which they were initially enrolled, regardless of their subsequent participation in the intervention or other service use. Prospective meta-analysis was used to address whether there were any intervention effects at 12 months and whether these effects varied by key program characteristics. The meta-analyses used different effect size estimation techniques depending on whether there were baseline differences on the outcome variable (28). HLM techniques were used to address whether the intervention effects or program contrast effects interacted with or were explained by person-level variables. The HLM analyses controlled for any personal characteristics correlated with the outcome variable at baseline.
Meta-analysis
Prospective meta-analysis is a technique for analyzing the site-to-site variability in treatment effects (28). The analyses of the 12-month outcomes follow the procedures used at six months (16), which involved calculating both site and overall weighted effect sizes and then modeling the heterogeneity of site outcomes by using program-level contrast variables.
Program contrasts, developed a priori, provide a way to test hypotheses that might explain the site-to-site variation in outcomes (28). In this study each contrast represents a program element that varied across sites and was thought to be an important influence on women's treatment outcomes. The two contrasts that were significant at six months—integrated counseling and core services—were assessed at 12 months.
Integrated counseling is a measure representing the number of treatment foci (mental health, trauma, or substance abuse) addressed in either individual or group counseling. Core services is a measure representing the number of core services (six possible) that women received. Both measures were taken from women's three-month self-report of services received. For further details about program contrast measurement, see Cocozza and colleagues' (16) study.
Each site was classified according to the level of contrast for each program element. The classification of high contrast depended solely on whether the intervention provided significantly more (by statistical test) of the program element than its comparison condition. For example, if at site 1 the intervention condition integrated counseling significantly more than its comparison condition, then site 1 would be a high-contrast site for integrated counseling. If at site 2 the intervention condition integrated counseling to a similar or lesser degree than the usual-care condition, then site 2 would be a low-contrast site for this element. By grouping together high-contrast sites and comparing them (by analysis of variance) with low-contrast sites, the explanatory power of the underlying element can be tested.
Hierarchical linear modeling
The HLM analyses permit an exploration of person-level influences on outcomes in relation to the program-level influences. HLM was used to predict 12-month outcomes by using person-level variables, intervention condition, and program elements. The HLM analysis followed the same steps used for the six-month analysis and is described in detail elsewhere (17). The modeling procedure is briefly described below.
For each outcome measure a three-level HLM model was constructed: time at level 1, person at level 2, and site at level 3. Program contrasts is a categorical variable indicating whether there was high or low contrast for integrated counseling and core services at the participant's site (for example, low contrast for integrated counseling and high contrast for core services). The level 1 model is a function of time (baseline or 12 months) plus an error term. The level 2 model is a function of covariates (that is, personal characteristics), intervention (yes or no), and covariate × intervention interaction terms, with an error term (random effect) for the intercept but not for the slope. The level 3 model is a function of program contrasts, with an error term (random effect) for the intercept but not for the slope.
As part of the six-month analyses, the study team identified through literature review and discussion 45 potential covariates expected to be related to the outcome variables. The potential covariates were then screened on the basis of their correlations at baseline with each outcome measure. (For details of the screening process and results, see Morrissey and colleagues' [17] study.) In the analysis presented here, for each of the four outcomes, covariates that met or exceeded the minimum correlation threshold (|r|≥.10) were entered into a stepwise model selection process, and the program contrasts variable (including its interactions with intervention and time) was added to the selected model. Any person-level variable with a significant three-way interaction (covariate × intervention × time) was tested for a possible four-way interaction (× program contrasts), which was retained if significant at p<.05. In this way a final model was identified for each outcome measure. Covariates included in the final models are shown in Table 1. Several potential covariates did not meet the screening criteria or were deleted during the modeling process. A full list of potential covariates is available elsewhere (17). (Generic SAS code for the final models and model specification in vector notation are available from the primary author. The composite variables listed in Table 1 are described in detail elsewhere [29].)
The HLM results reported here are presented as two distinct categories of person-level effects, corresponding to effects related to the intervention and those related to the program contrasts. The program contrast effects involved higher-order interactions than the intervention effects. Consistent with standard practice, lower-order terms were not interpreted when there was a higher-order interaction involving the same covariates. To aid interpretation, the sign of each reported effect size and parameter estimate was adjusted such that a positive effect indicates improvement.
Results
Sample characteristics
The mean±SD age of women at baseline in the analysis sample (N=2,026) was 36±9. These women were from diverse racial and ethnic backgrounds: 349 participants, or 17 percent, were Hispanic; 1,018 participants, or 50 percent, were white non-Hispanic; 504 participants, or 25 percent, were black non-Hispanic; and 150 participants, or 7 percent, were other non-Hispanic. The median number of years of education was 12. About a third of the sample was married or partnered (783 participants, or 39 percent). A total of 574 participants (28 percent) had never married. Most had experienced homelessness (1,420 participants, or 70 percent), and half reported a current serious physical illness or disability (1,032 participants, or 51 percent). As a group these women reported long-term mental health problems, long-term substance use, and trauma experiences, as indicated by the first mental health problem by age 12 (1,043 participants, or 51 percent), regular use of alcohol to the point of intoxication for at least five years (1,054 participants, or 52 percent), regular use of drugs for at least ten years (1,078 participants, or 53 percent), and childhood sexual or physical abuse (1,586 participants, or 78 percent).
Preliminary analyses (not reported here) indicated that compared with participants in the comparison group (N=1,008), participants in the intervention group (N=1,018) were less likely to be white non-Hispanic, more likely to be black non-Hispanic, more likely to report currently receiving court-ordered mental health or substance abuse treatment, more likely to have received mental health treatment two or more times or for at least six months, and more likely to report ever having received mental health treatment. The intervention condition also had higher baseline means on two composite measures (29)—frequency of childhood abuse and lifetime frequency of interpersonal abuse—and on the PSS. The intervention condition had a lower mean number of perceived barriers to receiving services and lower mean baseline ASI-D scores. Each mean difference was approximately .1 standard deviation units. These differences are unlikely to be clinically significant. Most of the differences in baseline severity were in a direction that indicates greater severity in the intervention condition than in the comparison condition.
Logistic regression indicated no significant difference in attrition between the intervention and comparison conditions, but it did reveal some differences between the analysis sample and the group that was lost to follow-up (p<.001 to p<.05). The group that was lost to follow-up had fewer years of education (a baseline mean±SD of 11.0±2.3 compared with a mean of 11.6±2.3) and demonstrated more difficulties on three measured variables: exposure to current stressors other than interpersonal abuse (a mean of 3.4±2.0 compared with a mean of 3.0±2.0), drug use severity (a mean on the ASI-D of .19±.17 compared with a mean of.16±.15), and trauma symptoms (a mean score on the PSS of 25.1±12.1 compared with a mean of 23.5±11.7). However, proportionally fewer women in the group that was lost to follow-up had a serious physical illness or disability (312 participants, or 44 percent, compared with 1,032 participants, or 51 percent, at baseline). Consequently, the results may not be generalizable to women who resemble those in the group that was lost to follow-up.
Intervention effects
As shown in Table 2, the raw means of each sample demonstrate that outcomes of women in both conditions improved. However, when women were compared by site with meta-analysis, the 12-month effect sizes for mental health and trauma symptoms showed statistically significant improvements for women in the intervention condition relative to those in the comparison condition (Table 3, last row). The effect on mental health symptoms doubled from .09 to .18 between six and 12 months, and the effect on trauma symptoms increased from .11 to .16. The two substance use severity outcomes showed no improvement over the corresponding values at six months (ASI-D effect size=.004, 95 percent confidence interval [CI]=-.086 to .094; ASI-A effect size=.017, CI=-.073 to .107).
Across the nine sites, a high contrast on integrated counseling was associated with a significant positive effect, and a high contrast on core services was associated with a significant negative effect. As a test of the relative significance of these contrasts, each site was assigned to one of four categories on the basis of its levels of contrast on integrated counseling and core services. As shown in Table 3, three of these categories contained at least two sites, yielding pooled estimates of the intervention effect that can be viewed with greater confidence than a single-site estimate. When a low contrast was seen for integrated counseling and a high contrast was seen for core services, the pooled effects were near zero. When a high contrast was seen for integrated counseling and a low contrast was seen for core services, the pooled effects were the highest. And when a high contrast was seen for integrated counseling and a high contrast was seen for core services, the pooled effects were intermediate. These results suggest that a high contrast for core services dampens the effects of integrated counseling (Table 3).
Despite the apparent influence of integrated counseling on positive outcomes, one site was not a high-contrast site for either integrated counseling or core services; however, it produced the largest effect size for mental health and trauma symptoms. This site demonstrates that good outcomes can occur outside of sites that show a high contrast for integrated counseling. Because this was the only site in this category, it is unknown whether sample differences or program implementation differences contributed most significantly to the outcome observed. In either case, the results for this site suggest that there may be other, unexamined avenues to improving outcomes.
Person-level characteristics and intervention effects
For each significant intervention effect, addressing whether intervention effects interact with or are explained by person-level variables involves identifying any significant covariate × intervention × time interaction in order to describe the conditions under which the intervention effect varies and, if there is no interaction with the intervention effect, checking for selection bias by examining whether the intervention effect is reduced to nonsignificance when personal characteristics are included in the model.
If program contrasts and person-level variables were ignored, significant intervention effects occurred at 12 months for mental health and trauma symptoms but not for drug or alcohol use severity. At 12 months, unadjusted HLM models yielded intervention effect sizes for the GSI and the PSS of .149 (p<.001) and .165 (p<.001), respectively. Effect sizes were not significant for the ASI-D and the ASI-A. These estimates were similar to the total effect sizes reported in Table 3 from the prospective meta-analysis.
In the HLM model predicting GSI, no person-level variable had a significant interaction with the intervention effect, and the intervention effect was not reduced by including person-level variables in the model.
In the HLM model predicting PSS two person-level variables interacted with the intervention effect: hospital (that is, inpatient or emergency department) treatment for violence, abuse, or trauma in the three months before baseline was negatively associated with intervention gain (effect size=-.705, p<.01) and hospital treatment for injury or physical complaint was positively associated with intervention gain (effect size=.213, p<.05). A supplemental, exploratory analysis found no interaction between these two hospital treatment variables. It should be noted that only 69 women (3.4 percent) reported treatment for violence, abuse, or trauma, and 753 (37.2 percent) reported treatment for injury or physical complaint. The larger of the two effects was quite strong even though it involved a small percentage of participants.
Person-level characteristics and program contrast effects
For each significant program contrast effect (program contrast × intervention × time), addressing whether significant program contrast effects interact with or are explained by person-level variables involves identifying any significant four-way interaction in order to describe the conditions under which the program contrast effect varies and, if there is no such interaction, checking for selection bias by examining whether the program contrast effect is reduced to nonsignificance when personal characteristics are included in the model.
Of the two outcome variables with significant intervention effects, only the GSI had a significant program contrast effect (p<.01). No significant four-way interaction was found for a personal characteristic. Table 4 shows the program contrast effect adjusted for personal characteristics, along with the unadjusted HLM estimates.
The pattern of unadjusted effect sizes in Table 4 was similar to that represented by the pooled estimates in Table 3 that show the average intervention effects for sites falling in each combination of contrast levels for integrated counseling and core services, as derived by using prospective meta-analysis. Three of the four adjusted effects were slightly smaller than their unadjusted counterparts, suggesting that person-level variables may partially account for differences in outcomes within each program contrast condition. However, the significant program contrast effect was not reduced to zero or to nonsignificance, indicating that the person-level variables do not completely explain this effect.
Clinical significance
At six months, a clear trend emerged. For women with severe baseline values, a greater percentage improved substantially when treated with the study intervention in sites that showed a high contrast for integrated counseling. For both the trauma and mental health symptom outcomes, the trend seems to have strengthened at the 12-month follow-up.
For the trauma symptom outcomes at 12 months, 71 percent of the women in the intervention group who had severe baseline PSS scores (128 of 180 participants) improved to at least the moderately severe range of functioning, and significant differences were found between women in the intervention and comparison groups in the sites that showed high contrast for integrated counseling. For women in these sites who had severe baseline PSS scores (81 women in the intervention group and 82 women in the comparison group), a greater percentage of women in the intervention group than those in the comparison group (30 percent compared with 21 percent) improved substantially—that is, to a moderate or better range of trauma symptoms.
The results were similar for the mental health outcomes of women in the high-contrast sites for integrated counseling. For the women in these sites, those who started the study in the severely distressed range of the GSI (T score of 75 or greater) were more likely to improve to functional or near functional status if they were in the intervention condition. At these sites, 23 of 74 women (31 percent) in the intervention group, compared with 15 of 93 women (16 percent) in the comparison group, improved from severe to moderate or less distress (T score less than 69). And 66 of 137 women (48 percent) in the intervention group, compared with 47 of 148 women (32 percent) women in the comparison group, improved from moderately severe baseline symptoms (T score of 69 to 74) to barely or not elevated levels of distress (T score of less than 65).
Discussion
The 12-month meta-analysis and HLM results reported here showed that women in the intervention group improved more on average than those in the comparison group. Among those with severe mental health or trauma symptoms at baseline, proportionally more women in the intervention group attained meaningful clinical improvement. Both the drug use and alcohol use severity effects leveled off relative to those effects at six months, but on average women's substance use did not revert to baseline levels. This pattern suggests that the study intervention achieved results more quickly than care as usual and that the results were maintained over time. Although these effects were small, they are encouraging given that clients with severe problems were targeted in the WCDVS. The demonstrated improvement suggests that these women can be helped. Future research should focus on better defining the program components associated with improvement.
Although the intervention was associated with more improvement than the comparison condition, not all program components contributed positively or equally to these results. Whereas receiving counseling that integrates treatment for trauma, mental health, and substance abuse was associated with greater improvement, receiving more of the core study services was associated with less improvement in the intervention condition relative to the comparison condition. This finding is counterintuitive and contrary to our expectations. One possible explanation, which could be explored in future studies, is that providing more services may require greater interagency coordination and place excessive travel and time demands on clients. Combined with the findings related to integrated counseling, the results suggest that integration of services may be more effective at the client level than at the agency level (16).
These program contrast results did not interact with personal characteristics and were not explained by them. This finding suggests that within the context of the intervention, program characteristics are important in determining outcomes and are largely independent of the personal characteristics tested. However, one site produced significant improvement among women in the intervention condition without using significantly more integrated counseling or core services than its comparison. This site's sample may differ in important ways from the other study or comparison sites or it may have implemented the intervention in a key but unmeasured way.
Of the 45 potential covariates, only two were related to the intervention effect at 12 months. These findings indicate that the intervention effect on trauma symptoms has a strong negative association with recent hospital treatment as a result of violence, abuse, or trauma (reported by only 3 percent of participants) and a weaker, positive association with recent hospitalization as a result of injury or physical complaint. However, no firm conclusion can be drawn about the relationship between recent trauma and the ability of services to reduce trauma symptoms, because these two effects were not significant at six months and were among a large number of potential covariates tested in the analysis presented here, because the hospital treatment variables were based on self-reported data, which may not give an accurate picture of recent hospital treatment, and because the two effects seem contradictory. Future research in this area should focus on accuracy in measuring the occurrence of and reasons for recent hospital treatment. If this relationship is confirmed and clarified, efforts should be directed at improving interventions for women who have been recently victimized.
Both the six- and 12-month outcomes of the WCDVS are consistent with a growing body of literature showing positive results from various approaches to integrated treatment (30,31,32,33,34,35,36,37). Most previous studies have not focused on women or the combination of substance abuse, mental health, and trauma as the WCDVS has. Thus the results reported here are important in suggesting that this constellation of problems may be amenable to an integrated approach.
Moreover, most studies thus far that have evaluated integrated manual-based interventions for trauma and substance abuse have found significant improvements and, equally important, none has found worsening of PTSD trauma-related symptoms, substance use disorders, or any other major variables (38,39,40). Yet research addressing women with co-occurring disorders and a history of trauma remains at an early stage (18).
This study has a number of limitations. First, because this was an intent-to-treat analysis, it did not include information about the actual amount of services received by participants in the intervention and comparison groups. We were unable to compare across sites and conditions the proportion of participants enrolled and retained in group interventions or the dosage received. It is possible that the reported intervention and program contrast effects may be due in part to differences in enrollment, engagement, retention, or dosage.
Second, our measures of integrated counseling and core services relied on self-reported data, which we were not able to validate with attendance data. Furthermore, participants' ratings of integrated counseling may be related to their level of symptoms. For example, improved symptoms may lead to, or may be caused by, better insight about the degree to which mental health, substance abuse, and trauma issues are being addressed in group interventions. Future research should focus on the direct measurement of integrated counseling and other program-level factors through logs or other service records.
Finally, although the meta-analysis controlled for some baseline differences and the HLM analysis was designed to control more completely for measured differences, this study used a quasi-experimental design. Any of the effects detected may be due in part to unmeasured baseline differences between participants in different study conditions or program contrast conditions or due to imperfections in the rigorous but admittedly arbitrary methods used to control for measured differences. The use of randomized designs in future research would overcome a number of these constraints.
Conclusions
Despite these limitations, the observed improvements suggest that women with severe symptoms, a history of violence and trauma, and co-occurring disorders may benefit from these kinds of interventions. However, some program aspects may be more beneficial than others, and some may be no more beneficial than usual care. It is important to replicate the key program findings and to identify the key unmeasured program components related to the best outcomes.
Although this study's design limitations preclude firm conclusions, the program contrast results at six and 12 months suggest that integrated counseling may be one of the key program features. There may be other key components as well, which is suggested by the significant results produced at a site that did not use more integrated counseling than its comparison site. Future research should attempt to dismantle and standardize the intervention, providing a stronger test of the utility of each individual component. If the importance of integrated counseling is confirmed, its most important aspects—for example, intensity, duration, and scope—can be delineated. In addition, research is needed to identify other program components related to improvement.
Acknowledgments
This study was funded by the Guidance for Applicants grant, number TI-00-003, from Substance Abuse and Mental Health Services Administration's three centers: the Center for Substance Abuse Treatment, the Center for Mental Health Services, and the Center for Substance Abuse Prevention. This grant was entitled Cooperative Agreement to Study Women With Alcohol, Drug Abuse and Mental Health Disorders Who Have Histories of Violence: Phase II. The authors thank Stephen Banks, Ph.D., for his consultations on statistical methods.
Dr. Morrissey is affiliated with the department of health policy and administration and the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill, 725 Martin Luther King Jr. Boulevard, Campus Box 7590, Chapel Hill, North Carolina 27599 (e-mail, [email protected]). Dr. Jackson is with Innovation Research and Training in Durham, North Carolina. Mr. Ellis is with the Cecil G. Sheps Center for Health Services Research at the University of North Carolina at Chapel Hill. Dr. Amaro is with Northeastern University in Boston. Dr. Brown is with PROTOTYPES in Culver City, California. Dr. Najavits is with the women's health sciences division of the National Center for PTSD in the Department of Veterans Affairs Boston Healthcare System and with Harvard Medical School in Boston. This is the first of three papers in this issue reporting results from the Women, Co-occurring Disorders, and Violence Study funded by SAMHSA.
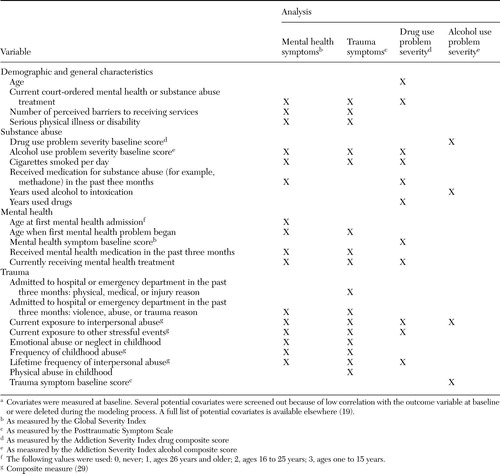 |
Table 1. Person-level covariates included in the final hierarchical linear modeling analyses in the Women, Co-occurring Disorders, and Violence Studya
aCovariates were measured at baseline. Several potential covariates were screened out because of low correlation with the outcome variable at baseline or were deleted during the modeling process. A full list of potential covariates is available elsewhere (19).
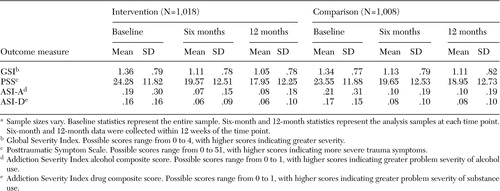 |
Table 2. Raw means and standard deviations of scores at baseline, six months, and 12 months, by type of treatment received in the Women, Co-occurring Disorders, and Violence Studya
aSample sizes vary. Baseline statistics represent the entire sample. Six-month and 12-month statistics represent the analysis samples at each time point. Six-month and 12-month data were collected within 12 weeks of the time point.
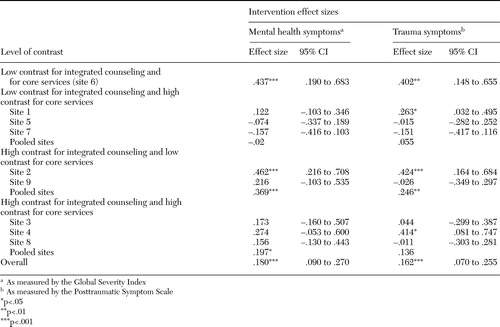 |
Table 3. Intervention effects at 12 months, by site and level of contrast for program elements in the Women, Co-occurring Disorders, and Violence Study
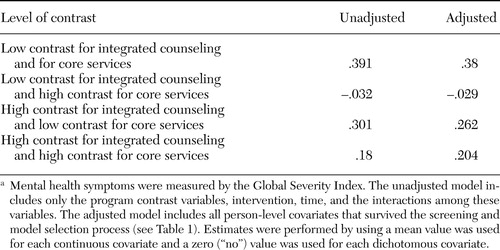 |
Table 4. Unadjusted and adjusted hierarchical linear modeling estimates of the intervention effect sizes for mental health symptoms at 12 months, by level of contrast for program elements in the Women, Co-occurring Disorders, and Violence Studya
aMental health symptoms were measured by the Global Severity Index. The unadjusted model includes only the program contrast variables, intervention, time, and the interactions among these variables. The adjusted model includes all person-level covariates that survived the screening and model selection process (see Table 1). Estimates were performed by using a mean value was used for each continuous covariate and a zero ("no") value was used for each dichotomous covariate.
1. Felitti V, Anda R, Nordenberg D, et al: Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine 14:245–258,1998Crossref, Medline, Google Scholar
2. Weiss M, Wagner S: What explains the negative consequences of adverse childhood experiences on adult health? Insights from cognitive and neuroscience research. American Journal of Preventive Medicine 14:356–360,1998Crossref, Medline, Google Scholar
3. Foege W: Adverse childhood experiences: a public health perspective. American Journal of Preventive Medicine 14:354–355,1998Crossref, Medline, Google Scholar
4. Dube S, Anda R, Felitti V, et al: Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors 27:713–725,2002Crossref, Medline, Google Scholar
5. Dube S, Anda R, Felitti V, et al: Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA 286:3089–3096,2001Crossref, Medline, Google Scholar
6. Kessler R, Sonnega A, Bromet E, et al: Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry 52:1048–1060,1995Crossref, Medline, Google Scholar
7. Ouimette P, Brown P: Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders. Washington, DC, American Psychological Association Press, 2002Google Scholar
8. Clark D, Lesnick L, Clark D, et al: Traumas and other adverse life events in adolescents with alcohol with alcohol abuse and dependence. Journal of the Academy of Child and Adolescent Psychiatry 36:1744–1751,1997Crossref, Medline, Google Scholar
9. Najavits L: Assessment of trauma, PTSD, and substance use disorder: a practical guide, in Assessment of Psychological Trauma and PTSD. Edited by Wilson J, Keane T. New York, Guilford, 2004Google Scholar
10. Davidson J: Recognition and treatment of posttraumatic stress disorder. JAMA 286:584–588,2001Crossref, Medline, Google Scholar
11. Dansky B, Roitzsch J, Brady K, et al: Posttraumatic stress disorder and substance abuse: use of research in a clinical setting. Journal of Traumatic Stress 10:141–147,1997Medline, Google Scholar
12. Brown P, Stout R, Gannon-Rowley J: Substance use disorder-PTSD comorbidity: patients' perceptions of symptom interplay and treatment issues. Journal of Substance Abuse Treatment 15:445–448,1998Crossref, Medline, Google Scholar
13. Ouimette P, Brown P, Najavits L: Course and treatment of patients with both substance use and posttraumatic stress disorders. Addictive Behaviors 23:785–795,1998Crossref, Medline, Google Scholar
14. Becker M, Noether C, Larson M, et al: Characteristics of women engaged in treatment for trauma and co-occurring disorders: findings from a national multi-site study. Journal of Community Psychology 33:429–443,2005Crossref, Google Scholar
15. Domino M, Morrissey J, Nadlick-Patterson T, et al: Service costs for women with co-occurring disorders and trauma. Journal of Substance Abuse Treatment 28:135–143,2005Crossref, Medline, Google Scholar
16. Cocozza J, Jackson E, Hennigan K, et al: Outcomes for women with co-occurring disorders and trauma: program-level effects. Journal of Substance Abuse Treatment 28:109–119,2005Crossref, Medline, Google Scholar
17. Morrissey JP, Ellis AR, Gatz M, et al: Outcomes for women with co-occurring disorders and trauma: program and person-level effects. Journal of Substance Abuse Treatment 28:121–133,2005Crossref, Medline, Google Scholar
18. Noether C, Finkelstein N, VanDeMark N, et al: Design strengths and issues of SAMHSA's Women, Co-occurring Disorders, and Violence Study. Psychiatric Services 56:1233–1236,2005Link, Google Scholar
19. Domino ME, Morrissey JP, Chung S, et al: Twelve-month service use and costs for women with co-occurring mental and substance use disorders and a history of violence. Psychiatric Services 56:1223–1232,2005Link, Google Scholar
20. McHugo G, Kammerer N, Jackson E, et al: Women, Co-occurring Disorders, and Violence Study: evaluation design and study population. Journal of Substance Abuse Treatment 28:91–107Google Scholar
21. Miller D, Guidry L: Addictions and Trauma Recovery: Healing the Body, Mind, and Spirit. New York, WW Norton, 2001Google Scholar
22. Najavits L: Seeking Safety: A Treatment Manual for PTSD and Substance Abuse. New York, Guilford, 2002Google Scholar
23. Harris M: T.R.E.M. Trauma Recovery and Empowerment: A Clinician's Guide for Working with Women in Groups. New York, Free Press, 1998Google Scholar
24. Clark C, Fearday F: Triad Women's Project Group Facilitator Manual and Workbook. Tampa, Fla, University of South Florida, 2001Google Scholar
25. McLellan A, Luborsky L, Woody G, et al: An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. Journal of Nervous and Mental Disease 168:26–33,1980Crossref, Medline, Google Scholar
26. Derogatis L: A Brief Form of the SCL-90-R: A Self-Report Symptom Inventory Designed to Measure Psychological Stress: Brief Symptom Inventory (BSI). Minneapolis, National Computer Systems, 1993Google Scholar
27. Foa E, Cashman L, Jaycox L, et al: The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psychological Assessment 9:445–451,1997Crossref, Google Scholar
28. Banks S, McHugo G, Williams V, et al: A prospective meta-analytic approach in a multisite study of homelessness prevention. New Directions for Evaluation 94:45–59,2002Crossref, Google Scholar
29. McHugo G, Caspi Y, Kammerer N, et al.: The assessment of trauma history in women with co-occurring substance abuse and mental disorders and a history of interpersonal violence. Journal of Behavioral Health Services and Research 32:113–127,2005Crossref, Medline, Google Scholar
30. Barrowclough C, Haddock G, Tarrier N, et al: Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. American Journal of Psychiatry 158:1706–1713,2001Link, Google Scholar
31. Donovan B, Padin-Rivera E, Kowaliw S: Transcend: initial outcomes from a posttraumatic stress disorder/substance abuse treatment program. Journal of Traumatic Stress 14:757–772,2001Crossref, Medline, Google Scholar
32. Drake R, Yovetich N, Bebout R, et al: Integrated treatment for dually diagnosed homeless adults. Journal of Nervous and Mental Disease 185:298–305,1997Crossref, Medline, Google Scholar
33. Hellerstein D, Rosenthal R, Miner C: Integrating services for schizophrenia and substance abuse. Psychiatric Quarterly 72:291–306,2001Crossref, Medline, Google Scholar
34. Judd P, Thomas N, Schwartz T, et al: A dual diagnosis demonstration project: treatment outcomes and cost analysis. Journal of Psychoactive Drugs 35(suppl 1):181–192,2003Medline, Google Scholar
35. Triffleman E, Carroll K, Kellogg S: Substance dependence posttraumatic stress disorder therapy: an integrated cognitive-behavioral approach. Journal of Substance Abuse Treatment 17:3–14,1999Crossref, Medline, Google Scholar
36. Ouimette P, Moos R, Finney J: Two-year mental health service use and course of remission in patients with substance use and posttraumatic stress disorders. Journal of Studies on Alcohol 61:247–253,2000Crossref, Medline, Google Scholar
37. Zlotnick C, Najavits L, Rohsenow D, et al: A cognitive-behavioral treatment for incarcerated women with substance use disorder and posttraumatic stress disorder: findings from a pilot study. Journal of Substance Abuse Treatment 25:99–105,2003Crossref, Medline, Google Scholar
38. Dumaine M: Meta-analysis of interventions with co-occurring disorders of severe mental illness and substance abuse: implications for social work practice. Research on Social Work Practice 13:142–165,2003Crossref, Google Scholar
39. Najavits L, Weiss R, Shaw S: The link between substance abuse and posttraumatic stress disorder in women: a research review. American Journal on Addictions 6:273–283,1997Medline, Google Scholar
40. RachBeisel J, Scott J, Dixon L: Co-occurring severe mental illness and substance use disorders: a review of recent research. Psychiatric Services 50:1427–1434,1999Link, Google Scholar



