Ethnic Differences in Substance Abuse Treatment Retention, Compliance, and Outcome From Two Clinical Trials
Abstract
OBJECTIVE: This study examined the results of two previous studies that evaluated African Americans and whites who were undergoing treatment for cocaine dependence to determine whether the groups differed in pretreatment characteristics, treatment retention, compliance, and cocaine use outcome. METHODS: Data were taken from two trials (N=111 in each), in which patients were randomly assigned to groups that used different behavioral treatments (cognitive-behavioral treatment and 12-step facilitation) and pharmacotherapies (desipramine and disulfiram). RESULTS: Few differences between African Americans and whites were found in terms of demographic characteristics, reasons for seeking treatment, or expectations of treatment. In both studies African Americans and whites did not differ significantly with respect to cocaine use outcomes, but African-American participants completed significantly fewer days of treatment than white participants. In study 2, which was not placebo controlled, African Americans who received disulfiram remained in treatment significantly longer than African Americans who did not receive disulfiram. However, in study 1, in which patients took either desipramine or a placebo, no interactions of ethnicity by medication were found. Among patients who expected improvement to take a month or longer in study 1, African Americans remained in treatment for fewer days than whites. CONCLUSIONS: The behavioral therapies evaluated did not significantly differ in effectiveness for African Americans and whites, suggesting that they are broadly applicable across these ethnic groups. Findings also suggest possible strategies for improving retention of African Americans in treatment. Such strategies might include offering treatment with a medication component and better addressing participants' treatment expectations.
Major problems in substance abuse treatment include patient's dropping out of treatment or failing to comply with treatment recommendations. Dropout rates are high, regardless of the type of treatment used (1,2,3). Because treatment retention and compliance are consistently linked to a better outcome, these factors remain important targets of substance abuse treatment (4,5).
Treatment retention and compliance are particularly important issues among ethnic minority populations, because the adverse effects of substance abuse and addiction are disproportionately manifested within these groups (6). For example, persons from ethnic minority groups who use drugs are at increased risk for HIV infection and AIDS, either because of their own or their partners' drug use or potential for risky sexual behavior (7,8). Moreover, several studies have suggested that persons from ethnic minority groups may have lower retention, higher dropout rates, and poorer compliance in substance abuse treatment than whites (8,9,10,11). Although several studies have noted differences in baseline functioning and baseline characteristics between African-American and white substance users, the implications of these differences have been inconsistent in relation to patient retention and compliance (12).
Few studies have considered ethnic differences in the context of clinical trials in which patients are randomly assigned to treatment groups. Data from these types of controlled trials may be particularly important in understanding the relationship between ethnicity and outcome in substance abuse treatment, because treatment duration, the nature of the interventions evaluated, and treatment outcomes are comparatively well defined in these types of clinical trials. In contrast to uncontrolled evaluations—in which content and length of treatment is variable and self-selection may affect treatments offered and received—randomized controlled trials have enhanced control over sources of extraneous variability that may offer a different perspective on the interaction of ethnicity and other predictors on the outcome of treatment.
To address these issues, we used data from two randomized, controlled clinical trials evaluating behavioral treatments and pharmacotherapies for cocaine dependence (13,14). The following questions were addressed: Do African-American and white participants differ in drug use habits or other demographic characteristics at baseline? Do they differ in treatment compliance or treatment outcome? Do they differ in response to specific behavioral or pharmacotherapeutic treatments?
Methods
The two, single-site clinical trials for this retrospective investigation (13,14) shared a number of methodological features, including 12 weeks of active psychotherapeutic treatment; similar inclusion and exclusion criteria; random assignment to study treatments; use of psychotherapy manuals for all conditions; delivery of treatments by therapists, most of whom had a doctorate; use of experienced therapists who received training and ongoing supervision; assessment by independent evaluators who were blind to the participants' treatment assignment (15); verification of patients' self-reported substance use by urine toxicology screens and breath analysis; evaluation of medication compliance by riboflavin testing; use of standardized assessment instruments; independent evaluation of the therapists' adherence and competence in delivering the manual-guided treatment (16,17); and a one-year follow-up after termination of the 12-week study treatments (18,19).
Participants in both studies were recruited from two substance abuse treatment centers in New Haven, Connecticut, and from the general population with public service announcements and newspaper advertisements. Institutional review board approval was obtained for both studies, and all participants provided written informed consent.
Overview of study 1
A total of 121 individuals meeting criteria for cocaine dependence were randomly assigned to one of four treatment conditions, using a 2 × 2 factorial design (14): cognitive-behavioral treatment plus desipramine; cognitive-behavioral treatment plus a placebo; clinical management—that is, a nonspecific psychotherapy that satisfied many of the requirements of a control condition—plus desipramine; and clinical management plus a placebo. The clinical trial data for this study were collected from 1989 to 1993. Findings from the original trial suggested an interaction between the severity of cocaine use and psychotherapy, in which cognitive-behavioral treatment appeared to be more effective in reducing cocaine use for more severe cocaine abusers. Rates of retention were not significantly different by treatment condition.
Overview of study 2
A total of 122 individuals meeting criteria for both cocaine and alcohol abuse and dependence were randomly assigned to one of five treatment conditions: cognitive-behavioral treatment plus disulfiram, 12-step facilitation plus disulfiram, clinical management plus disulfiram, cognitive-behavioral treatment plus no medication, and 12-step facilitation plus no medication (13). The clinical trial data for this study were collected from 1994 to 1997. Findings from the original study suggested rates of retention were significantly higher for participants who received disulfiram than for participants who did not take medication. Rates of retention among participants who received disulfiram were comparable across the three psychotherapy conditions. In the main phase of this study, the two active psychotherapies—cognitive-behavioral treatment and 12-step facilitation—were associated with significant reductions in cocaine use over time compared with clinical management. Disulfiram treatment was associated with significantly better retention in treatment, as well as with longer duration of abstinence from alcohol use and cocaine use.
Participants
Analyses in both studies were limited to comparisons of African-American and white participants, because of the small number of individuals from other ethnic groups. Ten of the 121 participants in study 1 and six of the 122 participants in study 2 were excluded because they indicated that they were neither African American nor white. Five additional individuals from study 2 were excluded from the analysis because of failure to comply with medication, medication side effects, and clinical deterioration. The final number of participants in each study totaled 111, with 53 African Americans and 58 whites in study 1 and 65 African Americans and 46 whites in study 2.
Assessments
For both studies, primary measures for assessing the effectiveness of treatment were treatment retention—the number of days in treatment—and treatment compliance—the number of days the participant abstained from cocaine use, which was assessed through self-report and weekly urine toxicology screens. Participants were assessed at baseline; weekly during the course of treatment; and at one, three, six, and 12 months following treatment. Severity of substance use and substance-related problems were measured by composite scores of the Addiction Severity Index (ASI) (20). Diagnoses were made at baseline using the Structured Clinical Interview for DSM-III-R (21).
Participants also completed questions assessing their pretreatment attitudes and expectations about drug treatment. Using Likert scales, participants rated how likely they would be to reduce or stop cocaine use with treatment and how soon they expected to notice positive treatment effects.
Data analysis
In both studies, questions assessing participants' expectations of treatment were grouped by confirmatory factor analyses (22) according to interventions consistent with cognitive-behavioral treatment, interpersonal therapy, clinical management, and medication. All goodness-of-fit indexes were greater than .9, indicating a good fit of the model for both studies.
Baseline differences between African Americans and whites were assessed by using chi square and t tests. Interactions of ethnicity by expectations, type of treatment, and type of medication were assessed in relation to outcomes by using analysis of variance (ANOVA) models. Aptitude treatment interactions (23,24), which enable modeling with a continuous variable, were used to evaluate outcome relationships by ethnicity and expectations of treatment.
Results
Ethnicity and baseline characteristics
Chi square tests compared the characteristics of study participants with the characteristics of nonparticipants. Nonparticipants included persons who were screened for the studies but did not meet inclusion criteria and those who met inclusion criteria but dropped out before they were randomly assigned to one of the treatment groups. In both studies, no significant differences were found in rates of eligible individuals who were randomly assigned to treatment.
In study 1, African Americans were significantly more likely than whites to fail to meet inclusion criteria; 44 percent of African American participants (42 of 95) failed to meet inclusion criteria compared with 27 percent of white participants (21 of 79) (χ2=8.4, df=2, p=.02). Rates of meeting inclusion criteria were not significantly different for African Americans and whites in study 2; 20 percent of African Americans (22 of 109) failed to meet inclusion criteria compared with 14 percent of whites (9 of 63). Of the 87 eligible African-American patients and 54 eligible white patients, only 65 African Americans and 46 whites participated in the study.
In both studies African Americans and whites tended to have similar baseline characteristics. As shown in Table 1, African Americans and whites did not differ significantly in either study with respect to gender, educational level, marital status, age, or baseline cocaine use. African Americans were significantly more likely than whites to smoke freebase cocaine than to use cocaine intranasally or intravenously. In both studies rates of lifetime major depression were significantly higher among white participants than among African Americans, and in study 2 white participants reported significantly greater depressive symptoms on the Beck Depression Inventory than African Americans.
In study 1, a comparison of pretreatment ASI composite scores suggested that African Americans and whites differed significantly only with regard to the employment composite, which indicated greater problem severity for African Americans. This finding was replicated in study 2. However, a comparison of other pretreatment ASI scores in study 2 indicated that whites had significantly greater problem severity with alcohol use, cocaine use, and psychological dimensions than African Americans.
Ethnicity and treatment expectations
As presented in Table 2, African-American and white participants in study 1 did not differ in their reasons for seeking treatment. In study 2, whites were significantly more likely than African Americans to cite employment, money, and emotional issues as reasons for seeking treatment. In both studies, African-American and white participants did not differ significantly in their goals for treatment, their expectations for time to improvement, or their expectation of what type of treatment would benefit them.
Ethnicity and treatment outcomes
As shown in Table 3, whites remained in treatment significantly longer than African Americans in both studies. However, across the two trials, no significant differences by ethnicity were found for cocaine use outcomes, including rates of cocaine-positive urine specimens, percentage of days abstinent from cocaine use, or medication compliance.
Ethnicity and type of intervention
No significant interaction of ethnicity by type of behavioral therapy for treatment retention or for outcome was seen in either study. In study 1, in which participants were taking either desipramine or a placebo, no significant interaction of ethnicity by medication type was found. However, in study 2, which was not placebo controlled, African Americans who received disulfiram remained in treatment significantly longer than African Americans who received no medication (F=4.3, df=1, 101, p=.03). In addition, African Americans assigned to cognitive-behavioral treatment or 12-step facilitation in study 2 were significantly more compliant with disulfiram treatment than African Americans assigned to clinical management, the psychotherapy control condition (F=4.1, df=1, 68, p=.05).
Ethnicity, baseline expectations, and outcomes
To test whether participants' baseline expectations of abstinence interacted with ethnicity for the major outcomes—number of days in treatment and treatment compliance—two-way ANOVAs were conducted in both studies. For both studies, no interactions between expectation of abstinence and ethnicity were found for either of the abstinence measures, self-reported cocaine use and urine toxicology screens. However, there was a significant interaction of expected time to improvement by ethnicity for retention in study 1 (F=5.7, df=1, 100, p=.02). Among participants who expected positive results only after completing a month or more of treatment, whites remained in treatment significantly longer. The mean±SD number of days in treatment was 74.6±18.0 days for whites and 33.6±29.7 for African Americans.
Discussion
The effects of ethnicity on treatment retention, compliance, and outcomes were evaluated in two clinical trials in which patients were randomly assigned to various groups to treat cocaine dependence. Overall, African Americans and whites tended to share similar baseline characteristics and treatment expectations. Moreover, no differences between ethnic groups were found in cocaine use outcomes. In both studies, African Americans were significantly less likely to complete treatment than whites. In study 2, which was not placebo controlled, African Americans who received disulfiram remained in treatment significantly longer than African Americans who were not assigned to a medication group. However, in study 1, in which participants received either desipramine or a placebo, no interaction was seen for medication by ethnicity on cocaine use outcome. Finally, there was a significant interaction of ethnicity and expectations for treatment in study 1; African Americans who expected positive treatment results to take a month or longer dropped out of treatment sooner than whites who held similar expectations.
Although most of the baseline characteristics of African Americans and whites were similar, three of these pretreatment variables were notably different by ethnicity in both studies: route of cocaine administration, rates of major depression, and employment problems. The finding that African Americans were more likely to report smoking freebase cocaine was similar to findings reported in previous work (9,25). These earlier studies also found that African Americans who reported using cocaine intravenously or smoking freebase cocaine as their primary route of administration were at greater risk for dropping out of treatment. Consistent with large-scale epidemiologic surveys (26), whites were significantly more likely to meet criteria for depressive disorders (27). African Americans also reported having more employment problems than whites in both studies. In study 1 no ethnic differences were found in reasons for seeking treatment. However, in study 2 employment, money, and emotional issues were more often cited by white participants as reasons for seeking treatment. Furthermore, in study 2, whites reported greater problem severity for cocaine use, alcohol use, and psychological issues than African Americans. Despite these differences, none of these variables appeared to be strongly related to outcome in either study. In both studies, African Americans and whites shared similar goals for treatment and expectations about the types of treatment they believed would be helpful to them.
The most salient difference between African Americans and whites in both trials was the poorer treatment retention among African Americans, which is consistent with other reports (8,9). Two interactions of ethnicity by treatment emerged that might be associated with differential attrition: medication effect and expectation for time to treatment benefits. The medication effect was seen only in study 1. Although both studies included a medication component, they differed with respect to whether or not patients knew they were assigned to active medication—study 1 was placebo controlled but study 2 was not. In study 1, there was no differential attrition by medication condition for either African Americans or whites. However, in study 2, African Americans who did not receive medication were significantly more likely to drop out of treatment than African Americans who received disulfiram. The better retention effect associated with the use of disulfiram among African Americans cannot be disentangled from the effects of merely taking medication. Offering a medication component may have had particular appeal to this group of African-American participants. For example, African Americans who more readily view their substance abuse as a serious problem may be more motivated to participate in and remain in treatment (28). However, African Americans may tend to regard substance abuse as an indication of personal weakness rather than a health concern (29). African Americans who received medication may have seen the medication as an explicit indicator of a health problem, instead of as a sign of weakness, and regarded treatment as more health focused. This fact may have improved their retention in the program. Further research is needed to evaluate this possibility.
A second factor associated with differential attrition among African Americans was expectations for time to treatment benefits. African Americans who expected treatment effects to be apparent in a month or more tended to drop out of treatment sooner than whites who held the same expectation. Discussing treatment expectations with African-American patients may help to develop realistic goals that are congruent with the treatments offered, which in turn may promote better retention among African Americans.
No effect of ethnicity by psychotherapy on outcome of treatment retention or cocaine use was found, suggesting that treatment was comparably effective for both groups. However, study 2 showed a significant effect of ethnicity by psychotherapy on medication compliance. This interaction may suggest a role for more active therapies such as cognitive-behavioral treatment or 12-step facilitation in enhancing medication compliance among African Americans.
Research has indicated that increased attrition in substance abuse treatment programs among African Americans may simply result from a number of health, social, and lifestyle differences that put them at a greater disadvantage than whites when seeking treatment (8,30). For example, employment problems reported by African Americans in the studies reported here may have interfered with their ability to remain in treatment.
Limitations of the study should be noted. First, findings reported here reflect a secondary analysis of ethnicity effects. Given the correlational nature of the findings, other variables that might covary with ethnicity—for example, socioeconomic status, perceived need for treatment, therapist-client alliance—may play an important role in these findings. Second, treatments offered were all short-term, outpatient behavioral approaches, with or without a medication component. Examining ethnic differences in outcomes across different types of programs—for example, intensive outpatient programs and inpatient treatment facilities—would be informative. Finally, the study focused on individuals who were randomly assigned to treatment in two clinical trials. These trials did not address factors associated with treatment entry and prerandomization attrition. However, our data suggest that ethnic differences in these areas were minor.
Conclusions
As one of a few reports available that addresses ethnic differences in treatment retention and outcome from well-controlled clinical trials of well-specified treatments, this report underlines the problem of retention among African Americans in substance abuse treatment. Although these data suggest that outcomes for African Americans and whites were comparable, we understand very little about the factors that prevent members of ethnic minority groups from seeking and being retained in treatment (31). Other studies replicating these methods may find significant differences between ethnic groups that in turn could contribute to different outcomes. Another concern is the tendency in such research to overstate the degree to which African Americans, or whites, constitute a homogeneous group (32). Additional research is necessary to better characterize the needs of African Americans and to design treatment programs that may be more responsive to their goals and expectations (8).
Overall, results suggest that the empirically supported behavioral therapies evaluated in these trials—cognitive-behavioral treatment and 12-step facilitation—are appropriate and effective for African Americans seeking treatment for cocaine dependence. Furthermore, the addition of a medication component to treatment may enhance treatment retention among African Americans.
The authors are affiliated with the psychiatry department at Yale University School of Medicine, Clinical Research Unit, 1 Long Wharf Drive, Suite 10, New Haven, Connecticut 06511 (e-mail, [email protected]).
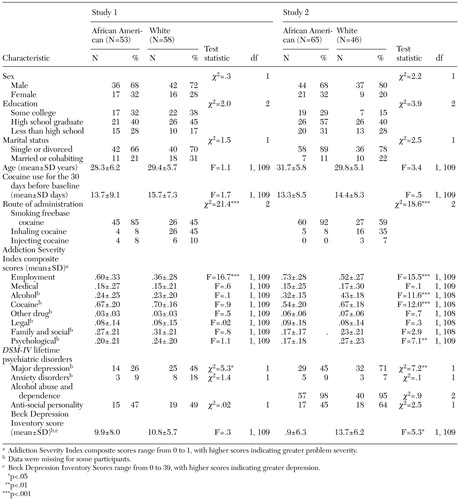 |
Table 1. Baseline characteristics of African-American and white participants in treatment for cocaine dependence
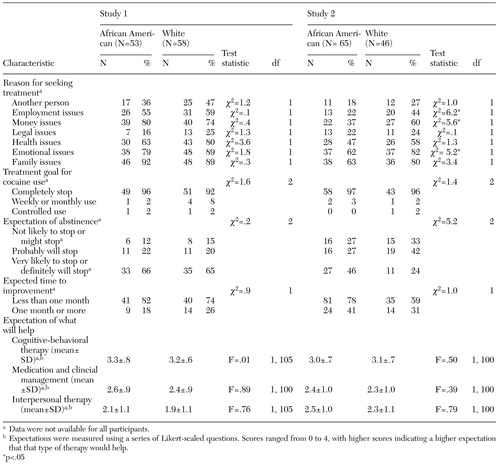 |
Table 2. Baseline differences among African-American and white participants in reasons for seeking cocaine treatment and in treatment goals and expectations
1. Simpson DD, Joe GW, Broome KM, et al: Program diversity and treatment retention rates in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors 11:279–293, 1997Crossref, Google Scholar
2. Simpson DD, Joe GW, Brown BS: Treatment retention and follow-up outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors 11:294–307, 1997Crossref, Google Scholar
3. Stark MJ: Dropping out of substance abuse treatment: a clinically oriented review. Clinical Psychology Review 12:93–116, 1992Crossref, Google Scholar
4. Mattson ME, DelBoca FK, Carroll KM, et al: Compliance with treatment and follow-up protocols in Project MATCH: predictors and relationship to outcome. Alcoholism: Clinical and Experimental Research 22:1328–1339, 1998Medline, Google Scholar
5. Principles of Drug Abuse Treatment: A Research-Based Guide. Bethesda, Md, National Institute on Drug Abuse, 2000Google Scholar
6. Allen K: Barriers to treatment for addicted African-American women. Journal of the National Medical Association 87:751–756, 1995Medline, Google Scholar
7. Longshore D, Hsieh S: Drug abuse treatment and risky sex: evidence for a cumulative effect. American Journal of Drug and Alcohol Abuse 24:439–451, 1998Crossref, Medline, Google Scholar
8. McCaul ME, Svikis DS, Moore RD: Predictors of outpatient treatment retention: patient versus substance use characteristics. Drug and Alcohol Dependence 62:9–17, 2001Crossref, Medline, Google Scholar
9. Agosti V, Nunes EV, Ocepeck-Welikson K: Patient factors related to early attrition from an outpatient cocaine research clinic. American Journal of Drug and Alcohol Abuse 22:29–39, 1996Crossref, Medline, Google Scholar
10. Longshore D: Help-seeking by African American drug users: a prospective analysis. Addictive Behaviors 24:683–686, 1999Crossref, Medline, Google Scholar
11. Sue S: Psychotherapeutic services for ethnic minorities: two decades of research findings. American Psychologist 43:301–308, 1988Crossref, Medline, Google Scholar
12. Castro FG, Proescholdbell RJ, Abeita L, et al: Ethnic and cultural minority groups, in Addictions: A Comprehensive Textbook. Edited by McCrady BS, Epstein EE. New York, Oxford University Press, 1999Google Scholar
13. Carroll KM, Nich C, Ball SA, et al: Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction 93:713–728, 1998Crossref, Medline, Google Scholar
14. Carroll KM, Rounsaville BJ, Gordon LT, et al: Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Archives of General Psychiatry 51:177–197, 1994Crossref, Medline, Google Scholar
15. Carroll KM, Rounsaville BJ, Nich C: Blind man's bluff? Effectiveness and significance of psychotherapy and pharmacotherapy blinding procedures in a clinical trial. Journal of Consulting and Clinical Psychology 62:276–280, 1994Crossref, Medline, Google Scholar
16. Carroll KM, Nich C, Rounsaville BJ: Use of observer and therapist ratings to monitor delivery of coping skills treatment for cocaine abusers: utility of therapist session checklists. Psychotherapy Research 8:307–320, 1998Crossref, Google Scholar
17. Carroll KM, Nich C, Sifry R, et al: A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence 57:225–238, 2000Crossref, Medline, Google Scholar
18. Carroll KM, Nich C, Ball, SA, et al: One year follow-up of disulfiram and psychotherapy for cocaine-alcohol abusers: sustained effects of treatment. Addiction 95:1335–1349, 2000Crossref, Medline, Google Scholar
19. Carroll KM, Rounsaville BJ, Nich C, et al: One year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: delayed emergence of psychotherapy effects. Archives of General Psychiatry 51:989–997, 1994Crossref, Medline, Google Scholar
20. McLellan AT, Kushner H, Metzger D, et al: The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:199–213, 1992Crossref, Medline, Google Scholar
21. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV, Patient Edition. Washington, DC, American Psychiatric Press, 1995Google Scholar
22. Bollen KA: Structural Equation Modeling With Latent Variables. New York, Wiley, 1989Google Scholar
23. Smith B, Sechrest L: Treatment of aptitude × treatment interactions. Journal of Consulting and Clinical Psychology 59:233–244, 1991Crossref, Medline, Google Scholar
24. Snow RE: Aptitude-treatment interactions as a framework for research on individual differences in psychotherapy. Journal of Consulting and Clinical Psychology 59:205–216, 1991Crossref, Medline, Google Scholar
25. Havassy BE, Wasserman DA, Hall SM: Social relationships and abstinence from cocaine in an American treatment sample. Addiction 90:699–710, 1995Crossref, Medline, Google Scholar
26. Kessler RC, Crum RM, Warner LA, et al: Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Study. Archives of General Psychiatry 54:313–321, 1997Crossref, Medline, Google Scholar
27. Kessler RC, McGonagle KA, Zhao S, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Study. Archives of General Psychiatry 51:8–19, 1994Crossref, Medline, Google Scholar
28. Longshore D, Grills C, Anglin MD, et al: Treatment motivation among African American drug-using arrestees. Journal of Black Psychology 24:126–144, 1998Crossref, Google Scholar
29. Wright EM: Substance use in African American communities, in Ethnocultural Factors in Substance Abuse Treatment. Edited by Straussner SL. New York, Guilford, 2001Google Scholar
30. Sanders-Phillips K: Factors influencing health behaviors and drug abuse among low-income black and Latino women, in Drug Addiction Research and the Health of Women. Edited by Wetherington C, Roman AB. NIH pub no 98–4290. Rockville, Md, National Institute on Drug Abuse, 1998Google Scholar
31. Wells K, Klap R, Koike A, et al: Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry 158:2027–2032, 2001Link, Google Scholar
32. Lillie-Blanton M, Parsons PE, Gayle H, et al: Racial differences in health: not just black and white, but shades of gray. Annual Review of Public Health 17:411–448, 1996Crossref, Medline, Google Scholar



