Comparison of Comorbid Physical Illnesses Among Veterans With PTSD and Veterans With Alcohol Dependence
Abstract
Posttraumatic stress disorder (PTSD) is associated with high rates of medical service use and with self-reported poor health. Male veterans admitted to a rehabilitation unit for PTSD (N=55) or alcohol dependence (N=38) were evaluated for comorbid psychiatric and medical conditions and health risk factors. Patients with PTSD were more likely to have osteoarthritis, diabetes, heart disease, comorbid depression, obesity, and elevated lipid levels. These findings suggest that there may be a relationship between specific medical conditions, possibly mediated by behavioral risk factors, among the aging population of veterans with PTSD.
Several studies of combat veterans with chronic posttraumatic stress disorder (PTSD) found that PTSD is associated with high rates of self-reported physical symptoms in multiple organ systems (1,2) and with an increased use of medical services (2). A review of discharge summaries revealed that 60 percent of veterans with chronic PTSD had an identified medical problem, and 42 percent of those persons had multiple problems (3).
Despite these findings, few reports have featured detailed assessments of medical conditions and health risk factors determined from direct clinical evaluations. The Centers for Disease Control and Prevention conducted comprehensive medical assessments in the Vietnam Experience Study (1); however, in that study, only veterans in their mid-30s were examined. A more recent study compared lipid levels of Vietnam veterans with chronic PTSD with those of a demographically matched group of volunteers from a substance abuse unit; the study found that the group of Vietnam veterans with PTSD had higher lipid levels (4). Volunteers with an alcohol or substance use problem were chosen as the comparison group because, like patients with chronic PTSD, they are a chronically ill population with high rates of comorbid psychiatric illness and health risk behaviors.
The study reported here investigated whether the prevalence of specific medical problems and health risk factors, such as smoking, obesity, and high lipid levels, differed significantly among veterans with chronic PTSD and veterans with alcohol dependence. This information, if validated further, may prove useful in addressing health care and medical education needs in this aging population.
Methods
We recruited male veterans who were admitted to a rehabilitation unit in the Miami Veterans Affairs Medical Center for chronic PTSD (N=55) or for alcohol dependence (N=38). Participants signed an informed consent form approved by the medical center's institutional review board. Patients were admitted for voluntary treatment following outpatient referral and screening, which established the need for residential intervention secondary to lack of or partial response to outpatient treatment. Patients with PTSD also needed to be alcohol- and drug-free for at least two months before admission. Length of stay for treatment was 12 weeks.
Patients with PTSD were recruited consecutively from 1997 to 1999. Patients with alcohol dependence were recruited during the same time period and were chosen because a review of their charts showed that they had demographic characteristics that matched those of patients with PTSD. Patients with alcohol dependence were excluded if they had any combat exposure or if they developed chronic PTSD because of another lifetime trauma.
Current and lifetime psychiatric diagnoses were assessed with the Structured Clinical Interview for DSM-III-R (SCID) (5) and then DSM-IV. Interviews were conducted during the first two to four weeks after the patient's admissions by a study investigator (DD or CW) and by one master's-level clinician under the supervision of study investigators (DD and TM).
A structured inquiry designed for this study addressed smoking pack-years (a pack year is one pack of cigarettes a day smoked in one year, or one-half pack a day smoked over two years), past history of intravenous drug use, and years of alcohol abuse, as well as any periods of abstinence from alcohol. Study investigators gathered this information at the interview at which they assessed current and lifetime psychiatric diagnoses. During this inquiry, the participant's body mass index (BMI) was calculated according to the Body Mass Index Nomogram (6).
Once patients were admitted to the treatment program, a medical history was taken and a physical examination was performed. Blood tests were performed to determine electrolytes, liver and thyroid functions, blood count, and fasting levels of glucose, triglycerides, and cholesterol. Additional laboratory and imaging studies and specialty consultant evaluations were performed as needed, on the basis of the patient's complaints about symptoms during the course of treatment.
After the participant completed treatment, the participant's medical data were reviewed by one of the study investigators (DD), who then determined the possible presence of a medical illness category, such as a cardiac, hepatic, or dermatologic condition. These diagnoses were determined from the patient's symptom reports and at least two of the following: supporting physical signs, positive laboratory tests or imaging tests or both, and a specialty consultant's opinion. Data that supported the presumptive diagnoses were then submitted to a board-certified internal medicine specialist (JE), who reviewed the information blind to the patient's diagnostic group. This final review resulted in the addition of eight more hepatic diagnoses, one more cardiac diagnosis, and four more pulmonary diagnoses and the deletion of one cardiac diagnosis.
Group differences for medical illness categories and health risk factors were analyzed by chi square and t tests. Odds ratios (ORs) were calculated for medical disorders found to be more prevalent in one of the two groups. Statistical analyses were performed with use of the SPSS software statistical package, version 6.
Results
Patients with PTSD and patients with alcohol dependence did not differ significantly in mean age, ethnicity, education level, employment, and homelessness status. Among patients with PTSD, the mean±SD age was 49.7± 5.7 years, compared with 48.3±8 years among patients with alcohol dependence. In the PTSD group, 62 percent of the patients (N=34) were white, 22 percent (N=12) were black, and 16 percent (N=9) were Hispanic. In the alcohol group, 71 percent (N=27) were white, 18 percent (N=7) were black, and 11 percent (N=4) were Hispanic. In the PTSD group, 58 percent (N=32) had graduated from high school, compared with 53 percent (N=20) from the alcohol group. In both groups, 18 percent were employed—ten in the PTSD group and seven in the alcohol group. In the PTSD group, 13 percent (N=7) were homeless, compared with 26 percent (N=10) in the alcohol group.
Patients with PTSD and patients with alcohol dependence did not differ in the lifetime prevalence of mania, dysthymia, panic and other anxiety disorders, substance abuse, and psychosis. Lifetime major depression was significantly more prevalent among patients with PTSD. Eighty-seven percent of patients with PTSD (N=48) experienced major lifetime depression, compared with 55 percent of patients with alcohol dependence (N=21) (χ2=11.0, df=1, p=.001). As expected, alcohol dependence was more prevalent in the alcohol group. Eighty-nine percent of patients with PTSD (N=49) had a history of alcohol dependence, compared with 100 percent of patients with alcohol dependence (N=38) (χ2=4.4, df=1, p=.04).
Patients with PTSD had significantly higher blood cholesterol and triglyceride levels, had higher BMIs, and were more frequently obese (defined as a BMI greater than 30). Among the 53 patients with PTSD for whom data were available, the mean cholesterol level was 213±38.7, compared with a mean cholesterol level of 188.5±38.3 among the 30 patients with alcohol dependence for whom data were available (t=2.8, df=81, p=.007). Among the 53 patients with PTSD with available data, the mean triglyceride level was 292.1±225.8, compared with a mean triglyceride level of 149.3±62.9 among the 23 patients with alcohol dependence with available data (t=3.0, df=74, p=.004). The mean BMI among patients with PTSD was 30.1± 6.6, compared with 25.1±4.6 among patients with alcohol dependence (t=4.1, df=89, p=.001). A total of 36 percent of patients with PTSD (N=20) were obese, compared with 16 percent of patients with alcohol dependence (N=6) (χ2=4.7, df=1, p=.03).
Patients with PTSD and patients with alcohol dependence did not differ in the lifetime prevalence of intravenous drug abuse. Patients with alcohol dependence had more years of alcohol abuse and more smoking pack-years. Patients with alcohol dependence had a mean of 26.6±9 alcohol abuse-years, compared with patients with PTSD who had a mean of 20.9±11 alcohol abuse-years (t=2.6, df=90, p=.01). Patients with alcohol dependence had a mean of 35.1±24.9 smoking pack-years, compared with a mean of 21.7±21.8 smoking pack-years among patients with PTSD (t=2.7, df=87, p=.008).
As shown in Table 1, patients with PTSD were more likely to have osteoarthritis, diabetes, and heart disease, whereas patients with alcohol dependence were more likely to have hepatic and pulmonary disease.
Patients with PTSD and patients with alcohol dependence did not differ with respect to the prevalence of other categories of medical illness reviewed, including dermatological, gastrointestinal, hematological, nephrological, neurological, prostatic and pulmonary illnesses, hypertension, and hearing and visual impairment.
Discussion
This study assessed the prevalence of medical illnesses and health risk factors among patients who had combat-related PTSD and compared the results with demographically matched patients who had alcohol dependence. The findings suggest a specific association between chronic PTSD or alcohol dependence and certain medical conditions, which is likely mediated by adverse health behaviors, such as smoking, alcohol abuse, and poor eating habits.
Diabetes and heart disease were more frequent among patients with PTSD, most likely because patients with PTSD have higher rates of risk factors associated with these diseases. The prevalence of diabetes among patients with PTSD in our study (23 percent) was significantly higher than that reported among adult males aged 44 to 65 years in the general population (6 percent) (7).
Despite the fact that 15 percent of patients with PTSD in our study were taking lipid-lowering agents (compared with none of the patients with alcohol dependence), cholesterol and triglyceride levels were significantly elevated in this group. Even with a conservative determination of obesity as a BMI greater than 30, patients with PTSD in our study were more frequently obese. These findings are consistent with those of Kagan and colleagues (4), who found that Vietnam veterans with PTSD had higher lipid levels than did a comparison group of patients with substance use problems
Osteoarthritis was also more prevalent among patients with PTSD in our study (56 percent), and this rate was significantly higher than that reported for arthritis, in general, among males aged 45 to 54 years (19 percent) (8). Obesity may contribute to the higher rates of osteoarthritis in patients with PTSD.
Not surprisingly, patients in rehabilitation for alcohol dependence were more likely to have hepatic disease, which is consistent with the known association between alcoholism and liver problems. The lower frequency of liver disease among patients with PTSD, who also had high lifetime alcohol abuse rates, may be related to the required abstinence before program admission; in fact, the mean alcohol abstinence period was significantly longer among patients with PTSD—50±63.9 months, compared with an average period of 3.1±7.9 months for patients with alcohol dependence (t=4.3, df=81, p<.001). Also, patients with PTSD may have had a lower alcohol intake over the years, a variable that was not measured in this study. Patients with alcohol dependence were also more likely to have pulmonary disease, mostly chronic obstructive pulmonary disease, a finding consistent with their having more smoking pack-years.
The study had several limitations. Veterans with PTSD frequently pursue service-connected disability benefits and may therefore attempt to document medical problems by reporting more symptoms, which may lead to more extensive medical evaluations. The question of whether the PTSD group had more imaging studies was therefore addressed. Patients with PTSD were more likely to have had a spine CT scan, an MRI, or a myocardial perfusion scan, but they were not more likely to have had plain x-rays, echocardiograms, exercise tolerance tests, or Holter monitoring studies. Patients with PTSD had a mean number of .7±1.1 imaging tests per patient, compared with an average of .06±0.2 imaging tests per alcohol patient (t=3.5, df=88, p<.001). Sixteen percent of patients with PTSD (N=9) had a myocardial perfusion scan, compared with 3 percent of patients with alcohol dependence (N=1) (χ2=4.4, df=1, p=.04).
When the medical illness analyses were restricted only to the patients who had imaging studies, osteoarthritis was still significantly more prevalent among patients with PTSD. Seventy-three percent of patients with PTSD (22 out of 30) had osteoarthritis, compared with 33 percent of patients with alcohol dependence (seven out of 21) (χ2=8.1, df=1, p<.005).
Heart disease was more prevalent among patients with PTSD who had imaging studies, but the difference was not statistically significant. Among patients who had imaging studies, 23 percent of patients with PTSD (six out of 26) had heart disease, compared with none of the patients with alcohol dependence (χ2=3.5, df=1, p=.06). The lack of heart disease among patients with alcohol dependence is striking, especially in view of their having had more smoking pack-years, and may be related to their having less extensive cardiac evaluations.
The number of patients in the study sample was relatively small, which may have limited the ability to detect meaningful differences between the two groups. A larger sample that is drawn from various sites may show different rates of medical and psychiatric morbidity. The study population was drawn from residential programs, which provide a more intensive level of care. Patients in the sample may have had more severe and chronic symptoms of PTSD or alcohol dependence, which would limit the generalizability of the results.
Nevertheless, because medical diagnoses were determined from extensive record review, prospective evaluations, and physical evidence, rather than from self-reports, our data suggest that veterans with chronic PTSD are at risk of developing specific medical illnesses. Similar findings have been reported by other investigators, who found that combat veterans with PTSD were more likely to develop several categories of medical diseases (9,10). The risk for elevated medical morbidity among veterans with PTSD may be enhanced by specific physiological alterations, additional psychiatric comorbidity, and, most likely, the high frequency of adverse behavioral risk factors.
Conclusions
The findings of our study suggest that the aging population of veterans with PTSD may be at increased risk of specific medical conditions, possibly mediated by behavioral risk factors. Further studies are needed to clarify the nature of this complex relationship, because this issue is becoming more pertinent among the aging veteran populations of World War II, Korea, and, especially, Vietnam.
Dr. David is affiliated with the department of psychiatry at the Miami Veterans Affairs Medical Center, 1201 Northwest 16th Street, 116A12, Miami, Florida 33125 (e-mail, [email protected]. gov), where Dr. Woodward and Dr. Esquenazi were affiliated at the time of the study. Dr. David is also with the department of psychiatry at the University of Miami. At the time of the study, Dr. Mellman was with the department of psychiatry at Dartmouth University in Lebanon, New Hampshire.
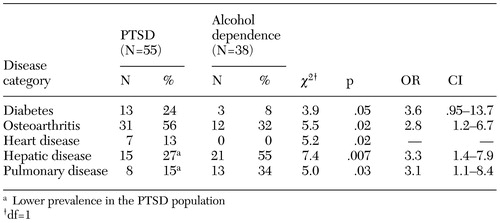 |
Table 1. Medical diagnoses among patients with chronic posttraumatic stress disorder (PTSD) and patients with alcohol dependence
1. Health status of Vietnam veterans: II. Physical Health. The Centers for Disease Control Vietnam Experience Study. JAMA 259:2708–2714, 1988Crossref, Medline, Google Scholar
2. Kulka RA, Schlenger WE, Fairbank JA, et al: Trauma and the Vietnam War Generation. New York, Brunner/Mazel; 1990Google Scholar
3. White P, Faustman W: Coexisting physical conditions among inpatients with post-traumatic stress disorder. Military Medicine 154:66–71, 1989Crossref, Medline, Google Scholar
4. Kagan BL, Leskin G, Haas B, et al: Elevated lipid levels in Vietnam veterans with chronic posttraumatic stress disorder. Biological Psychiatry 45:374–377, 1999Crossref, Medline, Google Scholar
5. Spitzer RL, Williams JBW, Gibbon M, et al: The Structured Clinical Interview for DSM-III-R (SCID): I. History, rationale, and description. Archives of General Psychiatry 49:624–629, 1992Crossref, Medline, Google Scholar
6. Obesity: Pathophysiology, Psychology, and Treatment. Edited by Blackburn GL, Kanders BS. New York, Chapman and Hall, 1994Google Scholar
7. Statistics: Diabetes Surveillance, 1999. Centers for Disease Control and Prevention, National Center for Health Statistics, Division of Health Interview Statistics, data from the National Health Interview Survey. US Bureau of the Census, census of the population and population estimates. Available at www.cdc.gov/diabetes/statistics/ survl99/chap2/table09.htmGoogle Scholar
8. Prevalence of arthritis—United States, 1997. Morbidity and Mortality Weekly Report 50:334–336, 2001Medline, Google Scholar
9. Beckham JC, Moore SD, Feldman ME, et al: Health status, somatization, and severity of posttraumatic stress disorder in Vietnam combat veterans with posttraumatic stress disorder. American Journal of Psychiatry 155:1565–1569, 1998Link, Google Scholar
10. Boscarino JA: Diseases among men 20 years after exposure to severe stress: implications for clinical research and medical care. Psychosomatic Medicine 59:605–614, 1997Crossref, Medline, Google Scholar



