Preferences for Schizophrenia Treatment Outcomes Among Public Policy Makers, Consumers, Families, and Providers
Abstract
OBJECTIVE: This study measured state public policy makers' ratings of the importance of several key schizophrenia treatment outcomes and compared them with the ratings of primary stakeholders in schizophrenia treatment. METHODS: Three groups of policy makers (40 administrative decision makers, 40 state legislators, and 20 legislative aides) and three groups of core stakeholders (20 persons with schizophrenia, 13 of their family members, and 20 of their mental health care providers) were recruited in Florida. Participants rated 12 descriptions of schizophrenia-related health states that reflected better and worse outcomes in six domains: psychotic symptoms, deficit symptoms, medication side effects, productive activity, daily activity, and social activity. RESULTS: All participants valued functional outcomes, such as improved productive and social activity, more than they valued improvements in symptoms. Public policy makers and primary stakeholders differed in the value they placed on two of the six outcomes. Compared with primary stakeholders, policy makers valued improvements in social functioning significantly more and improvements in medication side effects significantly less. CONCLUSIONS: Policy makers and primary stakeholders place similar value on some of the major goals of schizophrenia treatment, with both groups valuing functional outcomes most highly. However, the difference between groups in the importance placed on medication side effects may lead to conflicts in the allocation of resources to the provision of newer and more expensive medications, which are associated with fewer side effects. This initial examination of policy makers' views provides a starting point for developing consensus about schizophrenia treatment policies.
Public funds account for 64 percent of expenditures for the treatment of persons with schizophrenia (1), which makes public policy makers important—but often invisible—stakeholders in the treatment of this population. The legislative and administrative policy makers who allocate treatment resources at the federal, state, and local levels play major roles in shaping the nature and content of the public treatment system. Policy makers' decisions determine the types and amount of treatments that are available and who is eligible to receive them.
Given the importance of public policy makers, it is ironic that we have little systematic knowledge about their views of schizophrenia treatment outcomes or how their preferences for certain outcomes compare with those of primary stakeholders in the treatment process, such as patients, their families, and mental health care providers.
Policy makers and primary stakeholders may have different decision frameworks that lead to different patterns of outcome preferences. Public policy makers may consider the overall public good that is presumed to result from a particular policy or allocation decision rather than the more personal benefits or harms that may result for a primary stakeholder. Policy makers might therefore be expected to prefer outcomes that preserve public order and safety or that increase the overall productivity of communities. For example, the reduction of symptoms might be more highly valued than the reduction of side effects, and work productivity might be more highly valued than meaningful social relationships. Given the indirect relationships between policy decisions and outcomes for persons with schizophrenia, policy makers may prefer outcomes that appear to be directly related to their actions, such as improved housing status, over outcomes that appear to be more socially mediated and complex, such as meaningful interpersonal relationships. Finally, given the widely held attitudes toward the nature and legitimacy of mental disorders, policy makers may prefer clearly visible treatment outcomes, such as adaptive functioning, to those that are more difficult to observe, such as overall quality of life.
Policy makers clearly play an essential role in guiding public treatment systems, which effects treatment options and outcomes for primary consumers and their families. Thus understanding the outcome preferences of policy makers may be an important first step in framing public policy discussions. A better understanding of similarities and differences in the preferences of policy makers and other stakeholders can inform strategies to reduce areas of conflict and improve the coherence of public policy goals and personal outcomes.
Three groups of state policy makers play particularly important roles in shaping health and mental health care systems. Administrators, legislators, and legislative aides contribute to the interpretation and implementation of federal policies and regulations, design and execute state-level policies, and often oversee city and county health and mental health programs (2). Administrators in public health agencies have a wide range of oversight responsibilities, including licensing and quality control, administration of program funding, and operation of direct services (2). State legislators enact laws and regulations that span a similar range of health and mental health care activities, yet time and resource limitations often keep legislators from fully mastering all the issues that they must address. As a result, legislators often rely on career legislative staff for information, especially on complex issues that are not a high priority for the individual legislator or for his or her political party (3).
Given state policy makers' broad span of responsibility and limited time, some evidence suggests that their personal attitudes may be a key factor in shaping state health policy (4). Thus it is possible that personal attitudes and preferences may affect policy makers' decisions about schizophrenia treatment. In this study we undertook an initial examination of public policy makers' preferences for schizophrenia treatment outcomes. This study extended a study of patient, family, and provider preferences for such outcomes to include three groups of state-level public policy makers, with the goals of measuring policy makers' preferences for schizophrenia outcomes and comparing their preferences with those of primary stakeholders in schizophrenia treatment.
Methods
Participants
Three groups of policy makers and three groups of primary stakeholders were recruited in Florida. All phases of the study were approved by the University of South Florida's institutional review board, and all participants provided written informed consent after receiving both written and verbal explanations of the study.
Policy makers were recruited and interviewed between July 2000 and July 2001. The three groups of policy makers were administrators overseeing behavioral health and Medicaid programs (N=40), state legislators (N=40), and legislative aides (N=20). A list of eligible respondents was compiled for each group, and potential participants were contacted in random order and asked to participate in the study. Fifty-three administrators were approached, and 13 (25 percent) did not participate: five could not be reached, four were too busy, and four declined for other reasons. Eighty-nine legislators were approached, and 49 (55 percent) did not participate: eight could not be reached, 32 were too busy, and nine declined for other reasons. Thirty-five legislative aides were approached, and 15 (43 percent) did not participate: two could not be reached, four were too busy, and nine declined for other reasons.
The three primary stakeholder groups were persons receiving treatment for schizophrenia, their family members, and their mental health care providers. A sequential sample of 27 persons receiving schizophrenia treatment in the public mental health systems of Orange, Osceola, and Brevard counties who were enrolling in the Schizophrenia Care and Assessment Program (SCAP), a multisite observational study of schizophrenia and its treatment (5), were asked to take part in the preference assessment study. Seven potential participants (26 percent) declined to participate in the study: four refused and three could not be reached. With patients' permission, a family member (N=13) and a primary mental health care provider (N=20) were also asked to participate. We did not maintain detailed data on family members and providers who refused to participate, because patients were asked to provide the names of multiple potential participants. All primary stakeholder participants were interviewed between January and April 1999 and were compensated $20 for their participation.
Data collection and interview procedures
Data on preferences for schizophrenia treatment outcomes were collected during individual interviews that lasted for 30 to 45 minutes. Identical procedures were used for all participants. Interviewers and participants had matched copies of the interview materials (described below). To maximize comprehension and accuracy of responses, interviewers read the interview out loud and recorded participants' responses.
Most of the interview time was spent on rating 12 descriptions of health states associated with schizophrenia, employing methods developed and used in previous studies of preferences for schizophrenia treatment outcomes (6,7). The descriptions were presented as single paragraphs of "diary excerpts," which were written in the second person and described a health state lasting one year. The descriptions portrayed six key schizophrenia outcome domains, and each was described in two ways, reflecting better and worse outcomes. The levels and their descriptions were based on data collected from initial SCAP study participants and reflect the magnitude and nature of symptoms and functioning reported by persons receiving care for schizophrenia.
The six domains were psychotic symptoms (delusions and hallucinations), deficit symptoms (lack of interest and energy), side effects of standard antipsychotic medications (akathisia), productive activity (working or going to school), daily activity (shopping and household chores), and social activity (interactions with friends and family). The health state descriptions were created from the statements describing better and worse outcomes in each domain, using a fractional factorial design that permitted examination of relationships between domains (8).
The following is an example of one of the health state descriptions: "You often feel that people are spying on you and saying bad things about you. You don't do things very often with your friends or family. You sometimes feel fidgety. A lot of the time you feel tired and don't feel like doing anything. You don't have a job. Every day you do chores around the house like cleaning, cooking and shopping."
Participants were asked, "Think about how you would feel in the health state." Then they were asked to provide a global rating of each health state on a scale ranging from 0, the best possible health state, to 100, the worst possible health state. Policy makers provided some basic demographic data and characterized their knowledge about schizophrenia as "a little," "moderate," or "a lot."
Computing weights
Each participant's ratings of the health state descriptions were used to compute weights for his or her individual valuations of the six outcome domains; metric conjoint analysis was used for the computations (9,10). For each participant, the conjoint analysis produces a set of preference weights that sum to 1. The domains rated as more important have larger weights.
Results
Participants' characteristics
Characteristics of the three groups of policy makers are summarized in Table 1. The three groups differed significantly in their responses to a question about their knowledge of schizophrenia; administrators reported the highest level of knowledge and legislative aides the lowest. Characteristics of the three groups of primary stakeholders are summarized in Table 2.
Outcome preferences
Differences in preferences across outcome domains and stakeholder groups were examined by using a repeated-measures analysis of variance model in which the independent classification variable was the group and the within-subjects dependent variables were each participant's importance weights for the six outcome domains obtained from the conjoint analysis (participant-level data not shown). A significant main effect for domain was found, indicating that overall the outcome domains differed in importance to the participants (F= 15.21, df=5, 146, p<.001). As illustrated in Figure 1, all participants tended to value productive activity and social activity outcomes more highly than outcomes associated with medication side effects and deficit symptoms.
Figure 1 also illustrates the differences in outcome preferences between policy makers and primary stakeholders. At the aggregate level, the two groups differed in their preferences for two of the outcome domains. Compared with primary stakeholders, policy makers placed more value on improvements in social functioning (F=7.46, df=1, 150, p<.01) and placed less value on reductions in medication side effects (F=3.83, df= 1, 150, p=.05).
No statistically significant differences were found between the preferences of the three policy maker groups or the three primary stakeholder groups, which indicated relatively greater similarity within the policy maker and primary stakeholder groups than between them.
Discussion and conclusions
This initial examination of public policy makers' views of schizophrenia treatment outcomes suggests that policy makers and primary stakeholders have convergent views on some of the major goals of schizophrenia treatment. Both groups generally valued improvements in functioning, specifically productive and social activity, more than they valued improvements in symptoms, particularly deficit symptoms and medication side effects. This finding underscores the importance of including functional outcomes in evaluations of treatment effectiveness and improving our understanding of which policy alternatives best promote functional outcomes.
The results also indicate that, to a large extent, the differences in preferences that we might assume to exist between the more distally involved policy makers and persons more proximally involved in coping with schizophrenia are not as large as we might have expected. Both groups seem to place more value on outcomes related to community participation while being less concerned about symptoms of social withdrawal and medication side effects.
However, differences were found between the views of policy makers and primary stakeholders that may point to potential areas of conflict in the consequences of resource allocation strategies. The finding that policy makers view medication side effects as less important than do primary stakeholders may make policy makers less likely to allocate resources for the widespread purchase and use of atypical antipsychotic medications, which have more favorable side effect profiles but are substantially more expensive than conventional agents. Research that investigates the associations between use of the new medications and social participation, perhaps as a function of improved medication adherence, may be particularly important in this regard.
The modest size of the samples included in this study clearly limit the accuracy and specificity of the findings. The statistically significant differences among the primary stakeholder groups in the valuation of outcomes that have been observed in larger samples (7,11,12,13) were not evident in the small samples participating in this study. In addition, differences between the policy maker groups may emerge in studies of larger samples. However, because most policy decisions are local in character (14), it is not completely clear that policy makers who do not share a local context can be meaningfully pooled to increase sample size and power. In relation to this point, we had substantial difficulty recruiting policy makers for the study, particularly legislators. Fifty-five percent of the legislators we contacted declined to participate, compared with 25 percent of administrators and 26 percent of patients.
Given the potential biases that may result from the differences between groups in response rates, we must consider these findings suggestive and continue to develop methods for obtaining accurate data on policy makers' views that are less time-consuming, because legislators' time constraints were the primary reason for their nonparticipation. In addition, the data collected in this study focus only on ratings of importance and do not include measures of attitudes or beliefs or other factors that may have played a role in the participants' decision processes. Thus these data provide little insight into the formation of preferences for schizophrenia outcomes. The differences in preferences between policy makers and primary stakeholders would be more interpretable if we knew whether policy makers' preferences reflected those of the majority of their constituents and whether their preferences are based on previous knowledge of mental health issues or solely on the content of the preference assessment interviews.
Nonetheless, both the similarities and the differences in outcome preferences detected in this study provide a starting point for understanding the perspectives of public policy makers who shape publicly funded schizophrenia treatment. Collecting data on these preferences will promote more informed discussion of the relationships between resource allocation strategies, program designs, and anticipated outcomes. This information can be used to develop dissemination and education strategies that are tailored to the differential preferences of the multiple stakeholder groups involved in mental health care and to construct an initial framework for developing consensus on the most important effects of treatment and support for persons with schizophrenia.
Acknowledgments
This study was funded by Eli Lilly and Company as part of the Schizophrenia Care and Assessment Program (SCAP) study. The authors thank Lisa Pitram-Lamb for her contributions to the initial development of the study and Francine Rozewicz and Barbara Blackman for their data management assistance.
Dr. Shumway is affiliated with the department of psychiatry at the University of California, San Francisco, 2727 Mariposa Street, Suite 100, San Francisco, California 94110 (e-mail, [email protected]). The other authors are with the Louis de la Parte Florida Mental Health Institute of South Florida in Tampa. Ms. Saunders is also with the Children's Home Society, Gulf Coast Division, in Tampa. Ms. Pines and Mr. Beller are with STAR Consultants, Inc., in Altamonte Springs, Florida. Ms. Burbine is also with Halifax Medical Center in Daytona Beach, Florida.
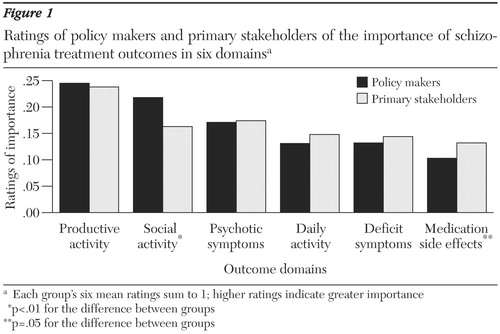
Figure 1. Ratings of policy makers and primary stakeholders of the importance of schizophrenia treatment outcomes in six domainsa
a Each group's six mean ratings sum to 1; higher ratings indicate greater importance
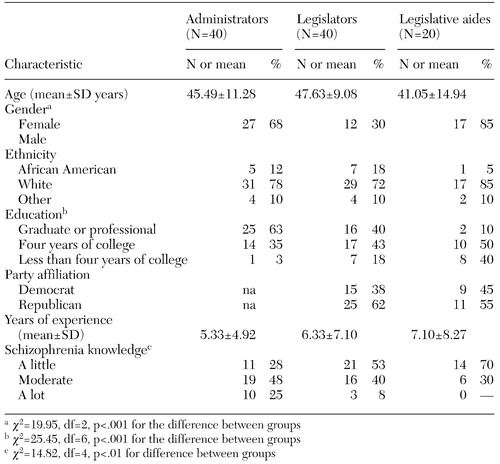 |
Table 1. Characteristics of three groups of public policy makers who participated in a study of their preferences for schizophrenia treatment outcomes
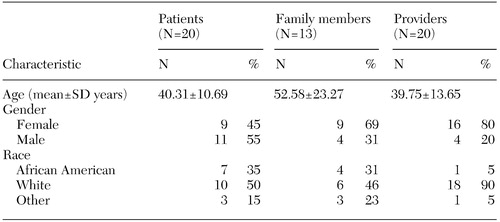 |
Table 2. Characteristics of three groups of primary stakeholders who participated in a study of their preferences for schizophrenia treatment outcomes
1. Rupp A, Keith SJ: The costs of schizophrenia: assessing the burden. Psychiatric Clinics of North America 16:413–423, 1993Crossref, Medline, Google Scholar
2. Weissert CS, Weissert WG: Governing Health: The Politics of Health Policy. Baltimore, Johns Hopkins University Press, 1996Google Scholar
3. Weissert CS, Weissert WG: State legislative staff influence in health policy making. Journal of Health Politics, Policy, and Law 25:1121–1148, 2000Crossref, Medline, Google Scholar
4. Buchanan RJ, Ohsfeldt RL: The attitudes of state legislators and state Medicaid policies related to AIDS. Policy Studies Journal 21:651–671, 1993Crossref, Google Scholar
5. Haley JC, Russo PA, Johnstone BM, et al: Prospective, naturalistic outcomes measurement: the Schizophrenia Care and Assessment Program (SCAP). Value in Health 1:89, 1998Crossref, Google Scholar
6. Shumway M, Chouljian T, Battle C: Stakeholder preferences for schizophrenia outcomes: an evaluation of assessment methods (abstract). Schizophrenia Research 24:258, 1997Crossref, Google Scholar
7. Shumway M: Preference weights for cost-outcome analyses of schizophrenia treatments: comparison of four stakeholder groups. Schizophrenia Bulletin, in pressGoogle Scholar
8. Cadman D, Goldsmith C: Construction of social value or utility-based health indices: the usefulness of factorial experimental design plans. Journal of Chronic Disease 39:643–651, 1986Crossref, Medline, Google Scholar
9. Kuhfeld WF: Conjoint Analysis Examples. Cary, NC. SAS Institute, 2000Google Scholar
10. Louvier JJ: Analyzing Decision Making: Metric Conjoint Analysis. Newbury Park, Calif, Sage, 1988Google Scholar
11. Fischer EP, Shumway M, Owen RR: Priorities of consumers, providers, and family members in the treatment of schizophrenia. Psychiatric Services 53:724–729, 2002Link, Google Scholar
12. Lee TT, Ziegler JK, Sommi R, et al: Comparison of preferences for health outcomes in schizophrenia among stakeholder groups. Journal of Psychiatric Research 34:201–210, 2000Crossref, Medline, Google Scholar
13. Lenert LA, Ziegler J, Lee T, et al: Differences in health values among patients, family members, and providers for outcomes in schizophrenia. Medical Care 38:1011–1021, 2000Crossref, Medline, Google Scholar
14. Miller JD, Kimmel LG: Biomedical Communications: Purposes, Audiences, and Strategies. San Diego, Academic Press, 2001Google Scholar



