Two-Year Trends in the Use of Seclusion and Restraint Among Psychiatrically Hospitalized Youths
Abstract
OBJECTIVES: This study examined characteristics associated with the use of seclusion and restraint among 442 psychiatrically hospitalized youths and sought to quantify changing trends in the rates of these modalities of treatment over time after the 1999 implementation of federal regulations and an institutional performance improvement program. METHODS: Demographic and clinical data related to all 5,929 incidents of seclusion and restraint that occurred during 2000 and 2001 at a child and adolescent state psychiatric hospital were analyzed. RESULTS: The two-year prevalence of use of seclusion was 61 percent and of restraint was 49 percent. Children and adolescents who were admitted on an emergency basis and those belonging to ethnic minority groups were more likely to undergo seclusion or restraint. Children aged 11 years and younger were more likely to undergo seclusion. The total number of episodes decreased by 26 percent and their cumulative duration decreased by 38 percent between the first quarter of 2000 and the last quarter of 2001. The decreases were the result of fewer seclusion and restraint incidents as well as shorter episodes of restraint. Over time, a concurrent increase was observed in the proportion of episodes associated with patient (but not staff) injuries and with as-needed use of medications. CONCLUSIONS: National reforms and institutional efforts can lead to downward trends in the use of seclusion and restraint among psychiatrically hospitalized youths. The active elements of these interventions warrant further study and replication.
Heightened legislative focus and media attention on the use of seclusion and restraint in psychiatric facilities, particularly among minors, has increased the need for reliable national data on such practices. Historically, clinicians have sought to refine the issue of seclusion and restraint by advocating that these interventions be used only in specific circumstances—to prevent harm to the patient or to other patients or staff, to prevent disruption to the treatment program, or to prevent physical damage to property, and in all of these circumstances only at times when less restrictive options have failed (1). Alternatively, some have posited that these interventions have significant therapeutic benefits beyond those of simply keeping a child safe (2). Some have even advocated the use of seclusion and restraint as a means of assisting children and adolescents in the development of mature defense mechanisms, of "learning control through the experience of control" (3).
The Department of Health and Human Services recently sought to address and reform the use of seclusion and restraint in psychiatric hospitals. Specifically, the Health Care Financing Administration (HCFA), now the Centers for Medicare and Medicaid Services, mandated in August 1999 the Interim Final Rule for the use of seclusion and restraint in all psychiatric treatment facilities that receive federal funding (4). The ruling states, in part, that mental health workers must have training in the use of these interventions, that a licensed independent practitioner must evaluate in person the need for each event within one hour of the its initiation, that the patient must be continually monitored by staff while undergoing seclusion or restraint, and that orders may not exceed a certain period, as determined by the patient's age. As a result of and concurrent with these reforms, many facilities implemented staff training programs aimed at reducing the use of seclusion and restraint, as articulated in the American Academy of Child and Adolescent Psychiatry's (AACAP's) practice parameters on the management of aggressive behavior (5).
It has been reasonable to expect that favorable changes in the use of seclusion and restraint would follow the implementation of the 1999 HCFA regulations. However, only one study has addressed whether these anticipated trends have occurred. In that study, the overall number of episodes of seclusion and restraint decreased by more than 50 percent and the mean duration of each episode by 41 percent during the three months after the institution of the HCFA rules (6). Those data, based on three adult inpatient units and one child unit, were not specifically analyzed with respect to patient demographic or clinical characteristics. Thus, to the best of our knowledge, seclusion and restraint among children and adolescents in psychiatric care facilities have not been reevaluated since the HCFA regulations were first implemented.
To further our understanding of the impact of these new administrative reforms and associated clinical interventions, we aimed in this study to examine demographic characteristics associated with the use of seclusion and restraint among psychiatrically hospitalized youths and also to quantify changing trends over a two-year period in the rates and patterns of these modalities of treatment.
Methods
Participants
This naturalistic study was based on data collected at Riverview Hospital for Children and Youth in Middletown, Connecticut. Riverview Hospital, with a licensed maximum inpatient bed count of 107 and an average of 244 admissions per year, is the largest psychiatric facility for children and adolescents in Connecticut and is run under the auspices of the Connecticut Department of Children and Families. Approval to review and abstract data was obtained from the institutional review boards of both the department and the Yale University School of Medicine. Clinical information was stripped of all personal identifiers, stored anonymously, and exclusively referenced through study-specific unique identifiers, according to published guidelines (7).
Demographic and clinical data were collected for all 442 patients who were hospitalized during the period between January 1, 2000, and December 31, 2001, including age, sex, race, admission status, primary diagnosis, and length of stay. Children and adolescents were admitted to the hospital through one of three mechanisms: a court order for mandated inpatient psychiatric evaluation and treatment (204 patients, or 46 percent), a Physician's Emergency Certificate (153 patients, or 35 percent), and voluntary admission, whereby a parent or caregiver provided written consent for admission (85 patients, or 19 percent). Diagnoses were based on intake information in the hospital's administrative database and were reduced to five mutually exclusive categories, the exact ICD-10 coding of which is available from the authors.
Measures and procedures
Data were collected in accordance with the internal performance improvement process outlined in the requirements of HCFA and the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO) and in full operation at Riverview Hospital as of January 1, 2000. Data were available for each of the 5,929 incidents of seclusion or restraint that took place during the study period, comprising 3,645 seclusion incidents (61 percent) and 2,284 restraint incidents (39 percent).
Event-specific information included the date and duration of each incident. In addition, for the events that occurred during 2001 (2,344 events, or 40 percent), information was available on injuries to patients or staff and on as-needed use of medications associated with each episode. These two variables were coded only as dichotomous yes or no variables, so qualitative information is not available on the type or severity of injuries, or on the type, dosage, or timing of the medications used.
Data analysis
Descriptive statistics and categorical analyses. Nominal and normally distributed continuous variables were compared across groups by using the chi square statistic and one-way analysis of variance, respectively. The likelihood of a child's undergoing any seclusion or restraint during his or her hospital stay was explored with multivariate logistic regression analysis. Separate models were run for the outcomes of each event. Odds ratios and 95 percent confidence intervals (CIs) are presented to quantify significant associations.
Adjusted time trends. The total number of events and their cumulative duration were summarized for each patient and expressed as total events per 1,000 patient days. This metric is common in national benchmarking surveys and allows for more ready interinstitutional comparisons. In an effort to understand the driving components of changing trends, we derived quarterly tallies per 1,000 patient days and episode duration in minutes separately for seclusion and restraint episodes. Averages for event-specific outcomes were derived through least-squares means to effectively adjust for the effects of age, sex, race, and admission status. Given that seclusion and restraint events were nested within patients and that characteristics of both the events and the patients were included in the regression models, the observations were not independent. To correct for the correlated nature of these data, the method of generalized estimation equations (GEE) was used in all adjusted analyses (8). Linear trend over time was evaluated by fitting identical models, except for the use of the quarterly period variable as a single ordinal (df=1), rather than as multiple dummy categorical parameters (df=7). The resulting slope (β), when divided by its standard error (SE), was compared with the normal distribution to yield a p value for linear trend.
All analyses were conducted with SAS, version 8.2; the PROC GENMOD function was used to derive adjusted means and GEE-adjusted parameters. The Cochran-Mantel-Haenszel chi square statistic was used to assess the linear trend of proportions over time.
Results
Sample characteristics
Demographic and clinical characteristics of the children and adolescents across the two study years are summarized in Table 1. Age and gender distributions remained stable over the two-year period, whereas racial composition changed—the proportion of Hispanic children hospitalized was higher in 2001. The source of admission changed significantly over the two-year period, with fewer court-ordered and more voluntary admissions in 2001. Diagnoses were relatively stable, with the notable exception of bipolar disorder, the frequency of which increased nearly fourfold between 2000 and 2001, from 4 percent to 14 percent. Length of stay increased significantly by five weeks (21 percent) over the two-year period. Despite this clear difference, the study participants had comparable effective times at risk (an average of 22 weeks) for which data were available. Notably, the one-year prevalence of use of seclusion and restraint did not change significantly across the two study years. However, this statistic does not address the number or the duration of separate events per child.
Demographic correlates of use
The two-year period prevalence of use of seclusion was 61 percent (269 patients) and of use of restraint was 49 percent (215 patients). A small number of patients (approximately 5 percent) accounted for a disproportionately high percentage of the seclusion and restraint episodes (approximately 50 percent for both seclusion and restraint). Demographic and clinical patterns emerged in the use of seclusion and restraint, even after multivariate adjustment (Table 2). Admission status was the single strongest and most consistent predictor: youths who were admitted to the hospital on an emergency basis were 3.5 times as likely to undergo seclusion and 4.6 times as likely to undergo restraint. Race was the second strongest predictor: black youths were more than twice as likely to undergo either type of intervention as white youths. Hispanic youths also had a higher likelihood of undergoing seclusion or restraint than white youths, but the difference was statistically significant only in the case of restraint. Age effects were significant only for the higher seclusion rates among younger children (ages five to 11 years). No differences were observed by gender or year (2000 versus 2001). Diagnosis variables were not included in the final regression models, because they did not significantly improve the model's fit and their administrative and intake source made their accuracy and clinical usefulness questionable. Moreover, substantial colinearity emerged between the diagnosis and admission status variables.
Adjusted time trends
The adjusted means and time trends for the use of seclusion and restraint during the study period are presented in Table 3. Even though the one-year prevalence of use did not change between 2000 and 2001, cumulative time spent in seclusion or restraint decreased by 3.1 hours, down to 5.2 hours per patient for the last quarter of 2001, representing a 38 percent reduction. The cumulative decrease was the result of fewer seclusion and restraint incidents as well as shorter episodes of restraint.
Injuries and as-needed use of medications
As can be seen from Table 4, the absolute number of patient injuries and as-needed use of medications associated with seclusion and restraint remained relatively stable throughout 2001. However, in light of the concurrent decrease in the number of episodes of seclusion or restraint, such injuries and as-needed medications evidenced a proportional increase during the same period (from 4 percent in the first quarter to 8 percent in the fourth for patient injuries and from 40 percent in the first quarter to 69 percent in the fourth for as-needed medications). Staff injuries were reported for a total of 205 incidents (9 percent), with no trend evident over time. These results should be interpreted with caution, given that the documentation of these variables had just recently been instituted.
Discussion and conclusions
This study represents the second collection of data on the use of seclusion and restraint since the HCFA rules were instituted in 1999 and is the first to analyze rates and time trends specific to psychiatrically hospitalized children and adolescents. Our data document a steady reduction over time in the number and duration of episodes of seclusion or restraint. Although the prevalence of use did not change over time, the number of episodes per patient and the duration of each episode (for restraint only) decreased. Even though this study could not address causality, the results do suggest that these trends are at least partly related to the instituted federal regulations. Moreover, we identified clinical and demographic characteristics that place patients at a higher risk of undergoing these interventions.
Our finding that younger patients have an increased risk of undergoing seclusion is consistent with the results of previous studies, whereas the lack of an age effect for restraint was unexpected. Specifically, it has been reported previously that within the child and adolescent population, younger patients are more likely to experience seclusion or restraint (9,10,11).
These data also demonstrate that patients from ethnic minorities are more likely to undergo seclusion or restraint than their white peers. Other studies have examined the role of ethnicity in the use of seclusion and restraint and have had conflicting results. In studies of adult inpatient units, it has been reported that black patients were more likely to be secluded than white patients (12,13). Other researchers have published similar findings, but after the data were stratified by age group, effects of ethnicity were not significant (14,15).
The racial disparities in aggressive behaviors and in the associated need for seclusion or restraint must be contextualized in relation to discrepancies in access to mental health care. It has been reported that African-American and Hispanic patients are significantly less likely to use psychiatric ambulatory care services than white patients (16) and are approximately half as likely to receive treatment from any source in the community (17). Rates of unmet need for mental health services have been shown to be consistently higher among children from ethnic minorities (18), whereas studies have shown that African Americans are overrepresented in inpatient treatment facilities (19,20), which suggests that when they do receive mental health treatment, their problems may be so severe as to warrant more restrictive levels of care. Hispanic patients are similarly underrepresented in all modalities of outpatient mental health care (19,21).
Taken together, these findings suggest that having less ready access to outpatient mental health services, minority youths may have more serious symptoms on entering the hospital, placing them at a higher risk of undergoing seclusion or restraint. Although contextual factors may provide a partial explanation for the higher risk of seclusion or restraint among persons from ethnic minorities, treatment providers should also remain vigilant regarding the potential for discrimination and the biased perception of assault risk and of the need for improved cultural competence training among staff.
Our data also show that admission status is an important independent predictor of both seclusion and restraint. Specifically, patients whose admission was either mandated by the courts or voluntary were less likely to undergo seclusion or restraint than those who were admitted to the hospital on an emergency basis. Several studies of adult inpatient units have shown that patients who were hospitalized involuntarily, either by a physician or by court order, were significantly more likely to undergo seclusion or restraint (12,15). However, other studies of adult inpatient populations did not replicate these results (22,23). It is important to note that many of the court-ordered evaluations in our study population were the result of nonviolent offenses, such as school or home truancy, petty theft, or failure to appear for a scheduled court date, which may explain the lower rates of seclusion and restraint among court-ordered youths.
This study documented an increase in the proportion of events associated with patient injuries and as-needed use of medications. This finding reflects a smaller denominator (number of seclusion and restraint episodes) rather than larger numerators (number of actual injuries or as-needed medications dispensed, both of which remained relatively stable). It is possible that as-needed medication was being used as an alternative technique for managing aggressive behavior more frequently and in keeping with AACAP's practice parameters, which consider such use of medication to be a valid technique for deescalating a crisis situation (5). These data suggest that as time progressed, the threshold for using seclusion and restraint increased, such that these interventions became selectively focused on the most dangerous patient behaviors. These same behaviors are more likely to be associated with patient injury and as-needed use of medication.
Given widely variable facility and population characteristics, it is difficult to compare seclusion and restraint rates across institutions. Nevertheless, it is necessary to put our data into context. A study conducted in 1997, based on 1994 survey results, may provide the most relevant data available for such a comparison. In that study (24), data were pooled across 124 inpatient state-sponsored facilities for adults, yielding 95th percentile rates for use of seclusion and restraint of 33 and 45 episodes per 1,000 patient days, respectively. Although the values we obtained in our study were clearly higher than those rates, the year of study and the younger patient population in our study may offer at least a partial explanation for the discrepancy and highlight the need for ongoing and accurate monitoring of seclusion and restraint practices.
Furthermore, our findings indicate that the prevalence of use of seclusion and restraint did not change over the study period. This finding does not signify that no reductions actually took place; rather, the number of incidents per patient and the duration of each episode decreased during the study period. These data suggest that seclusion and restraint remained necessary means of handling the most aggressive behaviors of individual patients and that the proportion of children requiring such interventions did not change substantially over time. However, the intensity of such interventions, as reflected in their number and duration, did appear malleable in response to different interventions.
Limitations
Several shortcomings need to be considered in the interpretation of our findings. First, this study examined data from a single public institution in Connecticut. As such, it may not be representative of most or even any other child and adolescent psychiatric hospitals. It remains to be seen whether similar trends become apparent at other institutions across the United States.
Second, although our data show a clear downward trend in the use of seclusion and restraint, the reasons for such reductions remain unclear and could not be addressed by this observational study. During the study period, two initiatives were under way within the institution: the HCFA rules themselves, and a performance improvement program, details of which are described in a column in this journal (25). Given the naturalistic and retrospective nature of this study, it was not possible to analyze the separate contributions or active elements of these initiatives. It is possible that any of these elements, alone or in combination, were responsible for the declines seen.
Third, our data did not address the use of interventions that, although they did not meet the JCAHO definitions of seclusion or restraint, may be considered restrictive nonetheless. Thus short physical holds (less than 15 minutes), "time-outs," "escorts," and "basket holds" were not included in our data set. As of July 2002, all these interventions are being routinely collected at Riverview Hospital. Future studies will assess trends associated with their use and specifically in relation to those of the "full" interventions addressed here.
Finally, our diagnostic data were limited to administrative data and were not formally structured diagnostic data. Another limitation was the paucity of qualifiers regarding the nature and severity of injuries or the characteristics of the as-needed medications used.
Clinical implications
This is the first study on seclusion and restraint patterns conducted specifically among minors after the implementation of national reforms mandated by HCFA in 1999. The results of this study demonstrate that significant reductions in the number and duration of episodes of seclusion and restraint are feasible as a result of concerted national and institution-specific efforts. Our results suggest that appropriate legislative action, together with concurrently implemented institutional performance improvement programs, can be successful in reducing the use of both seclusion and restraint. Further research is warranted to determine which training programs and elements thereof are most effective in reducing the use of these interventions.
Acknowledgments
This work was supported in part by PHS Scientist Career Development Award K01-MH01792 to Dr. Martin. The authors acknowledge the help with data management provided by Andrew Kass and Alex Speredelozzi. The authors dedicate this article to the memory of their friend and mentor Donald J. Cohen, M.D., director of the Yale Child Study Center since 1983 and chairman of the advisory board of Riverview Hospital of Children and Youth since 1993. Dr. Cohen, who died in October 2001, lived a life devoted to improving the lives of children, equally in Connecticut as throughout the world.
Ms. Donovan is affiliated with Yale University School of Medicine in New Haven, Connecticut. Dr. Plant, Dr. Siegel, and Dr. Martin are with the Child Study Center at Yale University School of Medicine. Ms. Peller is with Yale University School of Epidemiology and Public Health. Send correspondence to Dr. Martin, Yale University School of Medicine, 230 South Frontage Road, New Haven, Connecticut 06520-7900 (e-mail, andres. [email protected]).
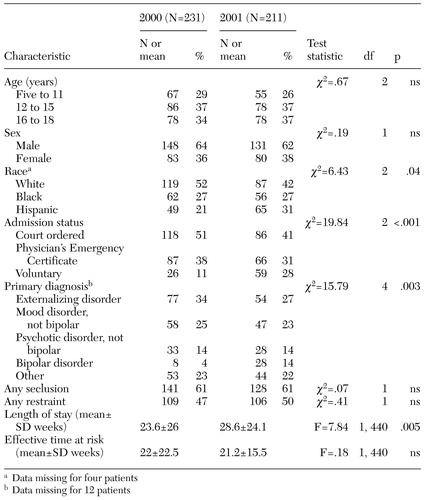 |
Table 1. Characteristics of 442 children and adolescents who participated in a two-year study of seclusion and restraint at a psychiatric hospital
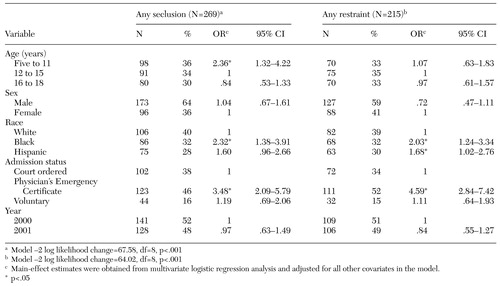 |
Table 2. Demographic correlates of use of seclusion and restraint in a sample of 442 psychiatrically hospitalized children and adolescents
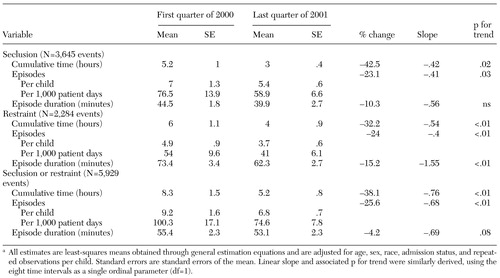 |
Table 3. Quarterly time trends for seclusion and restraint among 442 children and adolescents, 2000 to 2001a
a All estimates are least-squares means obtained through general estimation equations and are adjusted for age, sex, race, admission status, and repeated observations per child. Standard errors are standard errors of the mean. Linear slope and associated p for trend were similarly derived, using the eight time intervals as a single ordinal parameter (df=1).
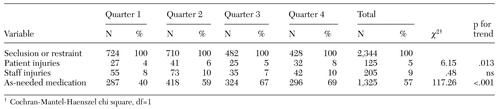 |
Table 4. Injuries and as-needed use of medications associated with seclusion and restraint among psychiatrically hospitalized children and adolescents in 2001
1. Gutheil T, Tardiff K: Indications and contraindications for seclusion and restraint, in The Psychiatric Uses of Seclusion and Restraint. Edited by Tardiff K. Washington, DC, American Psychiatric Press, 1984Google Scholar
2. Bath H: The physical restraint of children: is it therapeutic? American Journal of Orthopsychiatry 64:40–49, 1994Google Scholar
3. Cotton NS: The developmental-clinical rationale for the use of seclusion in the psychiatric treatment of children. American Journal of Orthopsychiatry 59:442–450, 1989Crossref, Medline, Google Scholar
4. Department of Health and Human Services, Health Care Financing Administration: Medicare and Medicaid Programs: Conditions of Participation: Patients' Rights. Interim Final Rule, 42 CFR 482. Federal Register 64:36069–36089, 1999Google Scholar
5. Masters KJ, Bellonci C, Bernet W, et al: Practice parameter for the prevention and management of aggressive behavior in child and adolescent psychiatric institutions, with special reference to seclusion and restraint. Journal of the American Academy of Child and Adolescent Psychiatry 41(2 suppl):4S- 25S, 2002Google Scholar
6. Currier GW, Farley-Toombs C: Use of restraint before and after implementation of the new HCFA rules. Psychiatric Services 53:138, 2002Link, Google Scholar
7. Simon GE, Unutzer J, Young BE, et al: Large medical databases, population-based research, and patient confidentiality. American Journal of Psychiatry 157:1731–1737, 2000Link, Google Scholar
8. Zeger SL, Liang KY, Albert PS: Models for longitudinal data: a generalized estimating equation approach. Biometrics 44:1049– 1960, 1988Crossref, Medline, Google Scholar
9. Mattson MR, Sacks MH: Seclusion: uses and complications. American Journal of Psychiatry 135:1210–1213, 1978Link, Google Scholar
10. Plutchik R, Karasu TB, Conte HR, et al: Toward a rationale for the seclusion process. Journal of Nervous and Mental Disease 166:571–579, 1978Crossref, Medline, Google Scholar
11. Garrison WT: Aggressive behavior, seclusion, and physical restraint in an inpatient child population. Journal of the American Academy of Child and Adolescent Psychiatry 23:448–452, 1984Crossref, Google Scholar
12. Soloff PH, Turner SM: Patterns of seclusion: a prospective study. Journal of Nervous and Mental Disease 169:37–44, 1981Crossref, Medline, Google Scholar
13. Flaherty JA, Meagher R: Measuring racial bias in inpatient treatment. American Journal of Psychiatry 137:679–682, 1980Link, Google Scholar
14. Carpenter MD, Hannon VR, McCleery G, et al: Ethnic differences in seclusion and restraint. Journal of Nervous and Mental Disease 176:726–731, 1988Crossref, Medline, Google Scholar
15. Way BB, Banks SM: Use of seclusion and restraint in public psychiatric hospitals: patient characteristics and facility effects. Hospital and Community Psychiatry 41:75–81, 1990Abstract, Google Scholar
16. Temkin-Greener H, Clark KT: Ethnicity, gender, and utilization of mental health services in a Medicaid population. Social Science and Medicine 26:989–996, 1988Crossref, Medline, Google Scholar
17. Freiman M, Cunningham P, Cornelius L: Use and Expenditures for Treatment of Mental Health Problems. Rockville, Md, Agency for Health Care Policy and Research, pub 94–0085, 1994Google Scholar
18. Shaffer D, Fisher P, Dulcan MK, et al: The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): description, acceptability, prevalence rates, and performance in the MECA Study: methods for the Epidemiology of Child and Adolescent Mental Disorders Study. Journal of the American Academy of Child and Adolescent Psychiatry 35:865–877, 1996Crossref, Medline, Google Scholar
19. Bui KV, Takeuchi DT: Ethnic minority adolescents and the use of community mental health care services. American Journal of Community Psychology 20:403–417, 1992Crossref, Medline, Google Scholar
20. Snowden LR, Cheung FK: Use of inpatient mental health services by members of ethnic minority groups. American Psychologist 45:347–355, 1990Crossref, Medline, Google Scholar
21. Yeh M, McCabe K, Hurlburt M, et al: Referral sources, diagnoses, and service types of youth in public outpatient mental health care: a focus on ethnic minorities. Journal of Behavioral Health Services Research 29:45–60, 2002Crossref, Medline, Google Scholar
22. Phillips P, Nasr SJ: Seclusion and restraint and prediction of violence. American Journal of Psychiatry 140:229–232, 1983Link, Google Scholar
23. Okin RL: The relationship between legal status and patient characteristics in state hospitals. American Journal of Psychiatry 143:1233–1237, 1986Link, Google Scholar
24. Crenshaw WB, Cain KA, Francis PS: An updated national survey on seclusion and restraint. Psychiatric Services 48:395–397, 1997Link, Google Scholar
25. Donovan A, Siegel L, Zera G, et al: Seclusion and restraint reform: an initiative by a child and adolescent psychiatric hospital. Psychiatric Services 54:958–959, 2003Link, Google Scholar



